Chest tube
A chest tube (chest drain, thoracic catheter, tube thoracostomy, or intercostal drain) is a flexible plastic tube that is inserted through the chest wall and into the pleural space or mediastinum. It is used to remove air (pneumothorax),[1] fluid (pleural effusion, blood, chyle), or pus (empyema) from the intrathoracic space. It is also known as a Bülau drain or an intercostal catheter.
| Chest tube | |
|---|---|
 The free end of the Chest Drainage Device is usually attached to an underwater seal, below the level of the chest. This allows the air or fluid to escape from the pleural space, and prevents anything returning to the chest. | |
| Other names | Intercostal drain |
| ICD-9-CM | 34.04 |
| MeSH | D013907 |
The concept of chest drainage was first advocated by Hippocrates when he described the treatment of empyema by means of incision, cautery, and insertion of metal tubes.[2] However, the technique was not widely used until the influenza epidemic of 1917 to drain post-pneumonic empyema, which was first documented by Dr. C. Pope, on "Joel", a 22-month-old infant.[3] The use of chest tubes in postoperative thoracic care was reported in 1922,[4] and they were regularly used post-thoracotomy in World War II, though they were not routinely used for emergency tube thoracostomy following acute trauma until the Korean War.[5]
Medical uses
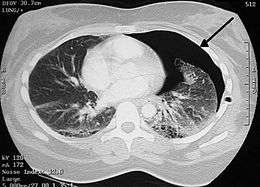
- Pneumothorax: accumulation of air or gas in the pleural space
- Pleural effusion: accumulation of fluid in the pleural space
- Chylothorax: a collection of lymphatic fluid in the pleural space
- Empyema: a pyogenic infection of the pleural space
- Hemothorax: accumulation of blood in the pleural space
- Hydrothorax: accumulation of serous fluid in the pleural space
Contraindications
Contraindications to chest tube placement include refractory coagulopathy and presence of a diaphragmatic hernia, as well as hepatic hydrothorax.[6] Additional contraindications include scarring in the pleural space (adhesions).
Complications
The most common complication of a chest tube is chest tube clogging. Chest tube clogging is widely recognized in published surveys of surgeons and nurses. In one study, 100% had seen chest tube clogging, and a majority had seen adverse patient outcomes from chest tube clogging.[7] In a prospective observational study, over 36% of patients had chest tube clogging after heart surgery.[8] Chest tube clogging can lead to retained blood around the heart and lungs that can contribute to complications and increase mortality.[9]
A common complication after thoracic surgery that arises within 30–50% of patients are air leaks.[10] Here, digital chest drainage systems can provide a remedy as they monitor intra-pleural pressure and air leak flow, constantly.[11]
Major insertion complications include hemorrhage, infection, and reexpansion pulmonary edema. Injury to the liver, spleen or diaphragm is possible if the tube is placed inferior to the pleural cavity. Injuries to the thoracic aorta and heart can also occur.[5]
Minor complications include a subcutaneous hematoma or seroma, anxiety, shortness of breath (dyspnea), and cough (after removing large volume of fluid). In most cases, the chest tube related pain goes away after the chest tube is removed, however, chronic pain related to chest tube induced scarring of the intercostal space is not uncommon.
Subcutaneous emphysema indicates backpressure created by undrained air, often caused by a clogged drain or insufficient negative pressure.
Device
Characteristics

Chest tubes are commonly made from clear plastics like PVC and soft silicone. Chest tubes are made in a range of sizes measured by their external diameter from 6 Fr to 40 Fr. Chest tubes, like most catheters, are measured in French catheter scale. For adults, 20 Fr to 40 Fr (6.7 to 13.3mm external diameter) are commonly used, and 6 Fr to 26 Fr for children. Conventional chest tubes feature multiple drainage fenestrations in the section of the tube which resides inside the patient, as well as distance markers along the length of the tube, and a radiopaque stripe which outlines the first drainage hole.[5] Chest tubes are also provided in right angle, trocar, flared, and tapered configurations for different drainage needs. As well, some chest tubes are coated with heparin to help prevent thrombus formation, though the effect of this is disputed.[13]
Chest tube have an end hole (proximal, toward the patient) and a series of side holes. The number of side holes is generally 6 on most chest tubes. The length of tube that has side holes is the effective drainage length (EDL). In chest tubes designed for pediatric heart surgery, the EDL is shorter, generally by only having 4 side holes.[14]
Channel style chest drains, also called Blake drains, are so-called silastic drains made of silicone and feature open flutes that reside inside the patient. Drainage is thought to be achieved by capillary action, allowing the fluids to travel through the open grooves into a closed cross section, which contains the fluid and allows it to be suctioned through the tube.[15] Though these chest tubes are more expensive than conventional ones, they are theoretically less painful.[16]
Chest drainage system

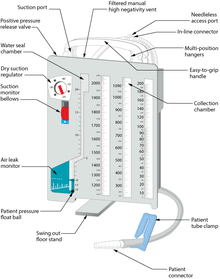
A chest drainage system is typically used to collect chest drainage (air, blood, effusions). Most commonly, drainage systems use three chambers which are based on the three-bottle system. The first chamber allows fluid that is drained from the chest to be collected. The second chamber functions as a "water seal", which acts as a one way valve allowing gas to escape, but not reenter the chest. Air bubbling through the water seal chamber is usual when the patient coughs or exhales but may indicate, if continual, a pleural or system leak that should be evaluated critically. It can also indicate a leak of air from the lung. The third chamber is the suction control chamber. The height of the water in this chamber regulates the negative pressure applied to the system. A gentle bubbling through the water column minimizes evaporation of the fluid and indicates that the suction is being regulated to the height of the water column. In this way, increased wall suction does not increase the negative pressure of the system. Newer drainage systems eliminate the water seal using a mechanical check-valve, and some also use a mechanical regulator to regulate the suction pressure. Systems which employ both these are dubbed "dry" systems, whereas systems that retain the water seal but use a mechanical regulator are called "wet-dry" systems. Systems which use a water seal and water column regulator are called "wet" systems. Dry systems are advantageous as tip-overs of wet systems can spill and mix with blood, mandating the replacement of the system. Even newer systems are smaller and more ambulatory so the patient can be sent home for drainage if indicated.[5]
More recently digital or electronic chest drainage systems have been introduced. An onboard motor is used as vacuum source along with an integrated suction control canister and water seal. These systems monitor the patient and will alert if the measured data are out of range. Due to the digital control of the negative pressure, the system is able to objectively quantify the presence of a pleural or system leak. Digital drainage systems allow clinicians to mobilize patients early, even for those on continuous suction, which is difficult to accomplish with the traditional water-seal system under suction.[10][17] Recently published clinical data indicates, that application of such systems can also lead to a reduction in complications.[18][19]
Technique
Tube thoracostomy
The insertion technique for emergency pleural drainage is described in detail in an article of the NEJM.[20] The free end of the tube is usually attached to an underwater seal, below the level of the chest. This allows the air or fluid to escape from the pleural space, and prevents anything returning to the chest. Alternatively, the tube can be attached to a flutter valve. This allows patients with pneumothorax to remain more mobile.
British Thoracic Society recommends the tube is inserted in an area described as the "safe zone", a region bordered by: the lateral border of pectoralis major, a horizontal line inferior to the axilla, the anterior border of latissimus dorsi and a horizontal line superior to the nipple.[21] More specifically, the tube is inserted into the 5th intercostal space slightly anterior to the mid axillary line.[22]
Chest tubes are usually inserted under local anesthesia. The skin over the area of insertion is first cleansed with antiseptic solution, such as iodine, before sterile drapes are placed around the area. The local anesthetic is injected into the skin and down to the muscle, and after the area is numb a small incision is made in the skin and a passage made through the skin and muscle into the chest. The tube is placed through this passage. If necessary, patients may be given additional analgesics for the procedure. Once the tube is in place it is sutured to the skin to prevent it falling out and a dressing applied to the area. Once the drain is in place, a chest radiograph will be taken to check the location of the drain. The tube stays in for as long as there is air or fluid to be removed, or risk of air gathering.
Chest tubes can also be placed using a trocar, which is a pointed metallic bar used to guide the tube through the chest wall. This method is less popular due to an increased risk of iatrogenic lung injury. Placement using the Seldinger technique, in which a blunt guidewire is passed through a needle (over which the chest tube is then inserted) has been described.
Postoperative drainage
The placement technique for postoperative drainage (e.g. cardiac surgery) differs from the technique used for emergency situations. At the completion of open cardiac procedures, chest tubes are placed through separate stab incisions, typically near the inferior aspect of the sternotomy incision. In some instances multiple drains may be used to evacuate the mediastinal, pericardial, and pleural spaces. The drainage holes are placed inside the patient and the chest tube is passed out through the incision. Once the tube is in place, it is sutured to the skin to prevent movement. The chest tube is then connected to the drainage canister using additional tubing and connectors and connected to a suction source, typically regulated to -20 cm of water.[15]
Dressings
After suturing, dressings are applied for hygienical reasons covering the wound. First, a y-slit compress is used around the tube. Second, a compress (10 x 10 cm) is placed on top and finally an adhesive plaster is added in a way that tension is avoided. A bridle rein is recommended to fix the tube to the skin. This tape bridge will prevent the tube from moving backwards and the possibility to cause clogging. It also prevents pain as it reduces tension on the fixation stitch. Alternatively, a large adhesive plaster that functions like a tape bridge may be used.[23]
Chest tube management
Chest tubes should be kept free of dependent loops, kinks, and obstructions which may prevent drainage.[24] In general, chest tubes are not clamped except during insertion, removal, or when diagnosing air leaks.
Manual manipulation, often called milking, stripping, fan folding, or tapping, of chest tubes is commonly performed to clear chest tube obstructions. No conclusive evidence has demonstrated that any of these techniques are more effective than the others, and no method has shown to improve chest tube drainage.[25] Furthermore, chest tube manipulation has proved to increase negative pressure, which may be detrimental, and painful to the patient.[25] For these reasons, many hospitals do not allow these types of manual tube manipulations.[7]
One option is active chest tube clearance without breaking the sterile field. According to a consensus of multiple experts in cardiac surgery, anesthesia and critical care in 2019 the ERAS Guidelines for Perioperative Care recommends active clearance of chest tubes to prevent retained blood and other complications.[26] This was given an IB-NR rating, meaning, it should routinely be performed. Makeshift efforts such as open chest tube clearing that involves breaking the sterile environment separating the chest tube from the drainage canister tubing to suction it out should not be performed (Class III, A).[27]
References
- Noppen M, Alexander P, Driesen P, Slabbynck H, Verstraeten A (May 2002). "Manual aspiration versus chest tube drainage in first episodes of primary spontaneous pneumothorax: a multicenter, prospective, randomized pilot study". American Journal of Respiratory and Critical Care Medicine. 165 (9): 1240–4. doi:10.1164/rccm.200111-078OC. PMID 11991872.
- Hippocrates (1847). Genuine Works of Hippocrates. Sydenham Society.
- Graham ME, Bell CR (1918). "Open Pneumothorax: Its relation to the treatment of empyema". J Med Sci. 156 (6): 839–871. doi:10.1097/00000441-191812000-00007.
- Lilienthal H (March 1922). "Resection of the lung for supportive infections with a report based on 31 consecutive operative cases in which resection was done or intended". Annals of Surgery. 75 (3): 257–320. doi:10.1097/00000658-192203000-00001. PMC 1399898. PMID 17864604.
- Miller KS, Sahn SA (February 1987). "Chest tubes. Indications, technique, management and complications". Chest. 91 (2): 258–64. doi:10.1378/chest.91.2.258. PMID 3542404.
- Runyon BA, Greenblatt M, Ming RH (July 1986). "Hepatic hydrothorax is a relative contraindication to chest tube insertion". The American Journal of Gastroenterology. 81 (7): 566–7. PMID 3717119.
- Shalli S, Saeed D, Fukamachi K, Gillinov AM, Cohn WE, Perrault LP, Boyle EM (2009). "Chest tube selection in cardiac and thoracic surgery: a survey of chest tube-related complications and their management". Journal of Cardiac Surgery. 24 (5): 503–9. doi:10.1111/j.1540-8191.2009.00905.x. PMID 19740284.
- Karimov JH, Gillinov AM, Schenck L, Cook M, Kosty Sweeney D, Boyle EM, Fukamachi K (December 2013). "Incidence of chest tube clogging after cardiac surgery: a single-centre prospective observational study". European Journal of Cardio-Thoracic Surgery. 44 (6): 1029–36. doi:10.1093/ejcts/ezt140. PMID 23520232.
- Balzer F, von Heymann C, Boyle EM, Wernecke KD, Grubitzsch H, Sander M (August 2016). "Impact of retained blood requiring reintervention on outcomes after cardiac surgery". The Journal of Thoracic and Cardiovascular Surgery. 152 (2): 595–601.e4. doi:10.1016/j.jtcvs.2016.03.086. PMID 27210474.
- Brunelli A, Cassivi SD, Salati M, Fibla J, Pompili C, Halgren LA, Wigle DA, Di Nunzio L (April 2011). "Digital measurements of air leak flow and intrapleural pressures in the immediate postoperative period predict risk of prolonged air leak after pulmonary lobectomy". European Journal of Cardio-Thoracic Surgery. 39 (4): 584–8. doi:10.1016/j.ejcts.2010.07.025. PMID 20801054.
- "Compact Digital Thoracic Drain Systems for the Management of Thoracic Surgical Patients: A Review of the Clinical Effectiveness, Safety, and Cost-Effectiveness". Canadian Agency for Drugs and Technologies in Health. October 1, 2014.
- "Chest Tube and Fuhrman Catheter Insertion". University of Bullfalo, The State University of New York. Archived from the original on 2010-04-08. Retrieved 2009-07-19.
- Kumar P, McKee D, Grant M, Pepper J (April 1997). "Phosphatidylcholine coated chest drains: are they better than conventional drains after open heart surgery?". European Journal of Cardio-Thoracic Surgery. 11 (4): 769–73. doi:10.1016/s1010-7940(96)01145-1. PMID 9151051.
- "PleuraFlow for Pediatric CT Surgery Clears Chest Tubes of Clots |". 2016-08-02.
- Obney JA, Barnes MJ, Lisagor PG, Cohen DJ (September 2000). "A method for mediastinal drainage after cardiac procedures using small silastic drains". The Annals of Thoracic Surgery. 70 (3): 1109–10. doi:10.1016/s0003-4975(00)01800-2. PMID 11016389.
- Frankel TL, Hill PC, Stamou SC, Lowery RC, Pfister AJ, Jain A, Corso PJ (July 2003). "Silastic drains vs conventional chest tubes after coronary artery bypass". Chest. 124 (1): 108–13. doi:10.1378/chest.124.1.108. PMID 12853511.
- Bertolaccini L, Rizzardi G, Filice MJ, Terzi A (May 2011). "'Six sigma approach' - an objective strategy in digital assessment of postoperative air leaks: a prospective randomised study". European Journal of Cardio-Thoracic Surgery. 39 (5): e128–32. doi:10.1016/j.ejcts.2010.12.027. PMID 21316980.
- Leo F, Duranti L, Girelli L, Furia S, Billè A, Garofalo G, et al. (October 2013). "Does external pleural suction reduce prolonged air leak after lung resection? Results from the AirINTrial after 500 randomized cases". The Annals of Thoracic Surgery. 96 (4): 1234–1239. doi:10.1016/j.athoracsur.2013.04.079. PMID 23866802.
- Miller DL, Helms GA, Mayfield WR (September 2016). "Digital Drainage System Reduces Hospitalization After Video-Assisted Thoracoscopic Surgery Lung Resection". The Annals of Thoracic Surgery. 102 (3): 955–961. doi:10.1016/j.athoracsur.2016.03.089. PMID 27234573.
- Dev SP, Nascimiento B, Simone C, Chien V (October 2007). "Videos in clinical medicine. Chest-tube insertion". The New England Journal of Medicine. 357 (15): e15. doi:10.1056/NEJMvcm071974. PMID 17928590.
- Laws D, Neville E, Duffy J (May 2003). "BTS guidelines for the insertion of a chest drain". Thorax. 58 Suppl 2 (90002): ii53–9. doi:10.1136/thorax.58.suppl_2.ii53. PMC 1766017. PMID 12728150.
- "Ventilatory management". University of Pretoria. Archived from the original on 2009-06-17. Retrieved 2009-09-16.
- Kiefer T (2017). Chest Drains in Daily Clinical Practice. Springer. pp. 102–103. ISBN 9783319323398.
- Schmelz JO, Johnson D, Norton JM, Andrews M, Gordon PA (September 1999). "Effects of position of chest drainage tube on volume drained and pressure". American Journal of Critical Care. 8 (5): 319–23. doi:10.4037/ajcc1999.8.5.319. PMID 10467469.
- Wallen M, Morrison A, Gillies D, O'Riordan E, Bridge C, Stoddart F (October 2004). "Mediastinal chest drain clearance for cardiac surgery". The Cochrane Database of Systematic Reviews (4): CD003042. doi:10.1002/14651858.CD003042.pub2. PMID 15495040.
- Engelman DT, Ben Ali W, Williams JB, Perrault LP, Reddy VS, Arora RC, et al. (May 2019). "Guidelines for Perioperative Care in Cardiac Surgery: Enhanced Recovery After Surgery Society Recommendations". JAMA Surgery. doi:10.1001/jamasurg.2019.1153. PMID 31054241.
- Halejian BA, Badach MJ, Trilles F (December 1988). "Maintaining chest tube patency". Surgery, Gynecology & Obstetrics. 167 (6): 521. PMID 3187876.
- Kartoun U (December 2018). "Improving the management of spontaneous pneumothorax". The European Respiratory Journal. 52 (6): 1801857. doi:10.1183/13993003.01857-2018. PMID 30523206.
- Porcel JM (December 2018). "Improving the management of spontaneous pneumothorax". The European Respiratory Journal. 52 (6): 1801918. doi:10.1183/13993003.01918-2018. PMID 30523207.
Further reading
- Catheter drainage is used for empyemas after chest-tube failure: vanSonnenberg E, Nakamoto SK, Mueller PR, Casola G, Neff CC, Friedman PJ, Ferrucci JT, Simeone JF (May 1984). "CT- and ultrasound-guided catheter drainage of empyemas after chest-tube failure". Radiology. 151 (2): 349–53. doi:10.1148/radiology.151.2.6709904. PMID 6709904.
- Commonly used after Percutaneous CT-Guided Lung Biopsies: Saji H, Nakamura H, Tsuchida T, Tsuboi M, Kawate N, Konaka C, Kato H (May 2002). "The incidence and the risk of pneumothorax and chest tube placement after percutaneous CT-guided lung biopsy: the angle of the needle trajectory is a novel predictor". Chest. 121 (5): 1521–6. doi:10.1378/chest.121.5.1521. PMID 12006438.
External links
