Buschke–Ollendorff syndrome
Buschke–Ollendorff syndrome, is a rare genetic disorder associated with LEMD3. It is believed to be inherited in an autosomal dominant manner.[5] It is named for Abraham Buschke and Helene Ollendorff Curth[6] who described it in a 45-year-old woman. Its frequency is almost 1 case per every 20,000 people and is equally found in both males and females.[4]
| Buschke–Ollendorff sign | |
|---|---|
| Other names | Dermatofibrosis lenticularis disseminata[1] |
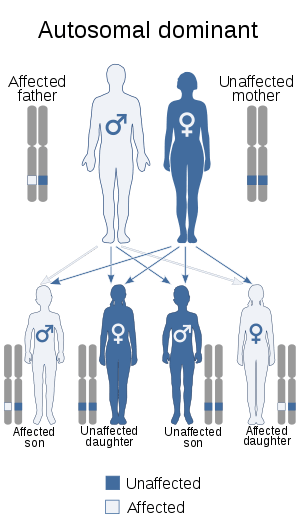 | |
| Buschke–Ollendorff syndrome has an autosomal dominant pattern of inheritance. | |
| Symptoms | Osteopoikilosis, bone pain[2] |
| Causes | Mutations in the LEMD3 gene.[2] |
| Diagnostic method | X-ray, ultrasound[3] |
| Treatment | Surgery for hearing loss(or complications)[4] |
Signs and symptoms

The signs and symptoms of this condition are consistent with the following (possible complications include aortic stenosis and hearing loss[2][4]):
- Osteopoikilosis
- Bone pain
- Connective tissue nevi
- Metaphysis abnormality
Pathogenesis
Buschke–Ollendorff syndrome is caused by one important factor: mutations in the LEMD3 gene (12q14), located on chromosome 12.
Among the important aspects of Buschke–Ollendorff syndrome condition, genetically speaking are:[7][8][9]
.jpg)
- LEMD3 (protein) referred also as MAN1, is an important protein in inner nuclear membrane.
- LEMD3 gene gives instructions for producing protein that controls signaling for transforming growth factor-beta.
- LEMD3 gene helps in the bone morphogenic protein pathway
- Both of the above pathways help grow new bone cells
- BMP and TGF-β pathways controls SMADs proteins, which then bind to DNA
- LEMD3 once mutated, causes a reduction of the protein, which in turn causes excess of the above two pathways.
Diagnosis

The diagnosis of this condition can be ascertained via several techniques one such method is genetic testing, as well as:[2][3]
- X-ray
- Ultrasound
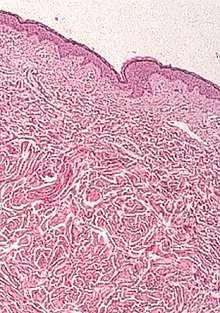
- Histological test
Differential diagnosis
The differential diagnosis for an individual believed to have Buschke–Ollendorff syndrome is the following:[3]
- Melorheostosis
- Sclerotic bone metastases.
Treatment
In terms of the treatment of Buschke–Ollendorff syndrome, should the complication of aortic stenosis occur then surgery may be required. Treatment for hearing loss may also require surgical intervention.[4]
See also
- Osteopoikilosis
- List of cutaneous conditions
- Melorheostosis
References
- Rapini, Ronald P.; Bolognia, Jean L.; Jorizzo, Joseph L. (2007). Dermatology: 2-Volume Set. St. Louis: Mosby. ISBN 978-1-4160-2999-1.
- "Buschke Ollendorff syndrome | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program". rarediseases.info.nih.gov. Retrieved 29 December 2017.
- RESERVED, INSERM US14 -- ALL RIGHTS. "Orphanet: Buschke Ollendorff syndrome". www.orpha.net. Retrieved 29 December 2017.
- Lukasz Matusiak (2 July 2008), Dermatofibrosis Lenticularis (Buschke–Ollendorf Syndrome), eMedicine, retrieved 2009-09-05
- Online Mendelian Inheritance in Man (OMIM) 166700
- A. Buschke, H. Ollendorff-Curth. Ein Fall von Dermatofibrosis lenticularis disseminata und Osteopathia condensans disseminata. Dermatologische Wochenschrift, Hamburg, 1928, 86: 257–262.
- Reference, Genetics Home. "Buschke-Ollendorff syndrome". Genetics Home Reference. Retrieved 2018-05-13.
- Worman, Howard J.; Fong, Loren G.; Muchir, Antoine; Young, Stephen G. (July 2009). "Laminopathies and the long strange trip from basic cell biology to therapy". The Journal of Clinical Investigation. 119 (7): 1825–1836. doi:10.1172/JCI37679. ISSN 1558-8238. PMC 2701866. PMID 19587457. Retrieved 13 May 2018.
- Reference, Genetics Home. "LEMD3 gene". Genetics Home Reference. Retrieved 2018-05-13.
- Hosen, Mohammad J.; Lamoen, Anouck; De Paepe, Anne; Vanakker, Olivier M. (2012). "Histopathology of Pseudoxanthoma Elasticum and Related Disorders: Histological Hallmarks and Diagnostic Clues". Scientifica. 2012: 1–15. doi:10.6064/2012/598262. ISSN 2090-908X.
-Creative Commons Attribution 3.0 Unported license
Further reading
- Pope, V.; Dupuis, L.; Kannu, P.; Mendoza-Londono, R.; Sajic, D.; So, J.; Yoon, G.; Lara-Corrales, I. (2016). "Buschke-Ollendorff syndrome: a novel case series and systematic review". The British Journal of Dermatology. 174 (4): 723–729. doi:10.1111/bjd.14366. ISSN 1365-2133. PMID 26708699.
- Helander, Martti Kormano, Ilmari Lindgren; with the collaboration of Inkeri; Lindgren, Ilmari (1999). Radiological findings in skin diseases and related conditions. Stuttgart: Thieme. ISBN 9783131161215. Retrieved 3 February 2018.
External links

- PubMed
| Classification | |
|---|---|
| External resources |
|