We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
Sympathetic crashing acute pulmonary edema (SCAPE)
From WikEM
Contents
Background
- Different from acute CHF exacerbation or hypotensive cardiogenic shock, which do not have sympathetic overdrive
- Patients can decompensate rapidly, so rapid intervention required
- Patients are generally more fluid depleted despite "wet" lungs, so do not give diuretics
- Usually history of poorly controlled hypertension
- Acute afterload increase causes pulmonary edema and poor peripheral perfusion
- Sympathetic surge occurs as a result of decreased systemic perfusion
- Afterload further increases and patient rapidly decompensates
Clinical Features
- Rales, crackles
- SBP >180 mmHg
- Tachycardic
Differential Diagnosis
Pulmonary Edema Types
Cardiogenic pulmonary edema
Noncardiogenic pulmonary edema
- Negative pressure pulmonary edema
- Upper airway obstruction
- Reexpansion edema
- Neurogenic causes
- Iatrogenic fluid overload
- Multiple blood transfusions
- IV fluid
- Inhalation injury
- Pulmonary contusion
- Aspiration pneumonia and pneumonitis
- Other
- High altitude pulmonary edema
- Hypertensive emergency
- ARDS
- Sympathetic crashing acute pulmonary edema (SCAPE)
- Immersion pulmonary edema
- Hantavirus pulmonary syndrome
Evaluation
- CBC (rule out anemia)
- Chem
- ECG
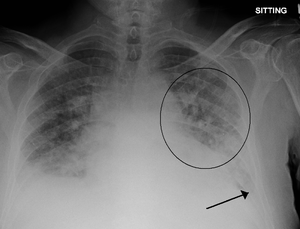
- CXR - signs of pulmonary congestion may not show for hours after acute flash pulmonary edema, so normal CXR is frequently seen
- Cephalization
- Interstitial edema
- Pulmonary venous congestion
- Pleural effusion
- Alveolar edema
- Cardiomegaly
- Troponin
- Ultrasound
- Bedside to assess global function, B lines, assessment of IVC
- Formal TTE/TEE
- Consider arterial line monitoring for titration of NTG
Brain natriuretic peptide (BNP)[1]
- Biologically active metabolite of proBNP (released from ventricles in response to increased volume/pressure)
- Utility is controversial and may not affect patient centered outcomes[2]
- May be trended to gauge treatment response in acute decompensated CHF
- May have false negative with isolated diastolic dysfunction
- Measurement
- <100 pg/mL: Negative for acute CHF (Sn 90%, NPV 89%)
- 100-500 pg/mL: Indeterminate (Consider differential diagnosis and pre-test probability)
- >500 pg/mL: Positive for acute CHF (Sp 87%, PPV 90%)
NT-proBNP[3][4][5]
- N-terminal proBNP (biologically inert metabolite of proBNP)
- <300 pg/mL → CHF unlikely
- CHF likely in:
- >450 pg/mL in age < 50 years old
- >900 pg/mL in 50-75 years old
- >1800 pg/mL in > 75 years old
Differential Diagnosis (Elevated BNP)
BNP In Obese Patients
- Visceral fat expansion leads to increased clearance of active natriuretic peptides[6]
- Obese patients also frequently treated for hypertension or coronary artery disease which may also contribute to lower BNP levels
Interpretation
- In one study of 204 patients with acute CHF, an inverse relationship between BMI and BNP was noted. The standard cutoff of 100pg/mL resulted in a 20% false-negative rate[7]
- Analysis of a subgroup of patients with documented BMI from the Breathing Not Properly study showed that a lower cutoff was more appropriate to maintain 90% sensitivity in obese and morbidly obese patients (54pg/mL)[8]
Management
Vasodilate arterial side, while maintaining oxygenation
- BiPAP with PEEP of 8 mmHg
- Titrate PEEP quickly to 12
- High dose nitroglycerin over 2 min (at these doses, NTG has vasodilation > venodilation[9])
- Goal BP at the patient's norm
- Load 800 mcg over 2 min (may start at 100 mcg/min, then titrate rapidly to 400 mcg/min for 2 min)
- Then start maintenance at 100 mcg/min, titrate up as needed
- NOTE: it takes time to set up NTG drip, so consider SL NTG in interim
- 0.4mg tab during 5 min = ~80 mcg/min (2 tabs = ~160 mcg/min, etc.)
- Difficult to titrate if giving more than 1-2 tabs
- Patients are likely more dehydrated that overloaded but should be recurrently volume assessed
- Consider captopril 12.5 - 25mg SL for continuation of afterload reduction[10]
- Wean CPAP after sustained BP at patient's baseline
- Decrease FiO2 to 40%
- Wean PEEP down 2 cm H2O q10 min
- At 5 cmH2O, trial of NC
Other Interventions
- Furosemide
- Targets kidneys which are poorly perfused in BOTH hypotension and catecholamine surge
- Consider waiting until BiPAP and NTG control hypertension first
- Nitroprusside, alternative when insufficient response to NTG
- Start 0.5 mcg/kg/min, titrate to blood pressure
- Max 10 mcg/kg/min for x10 min
- Cyanide toxicity risk increases proportionately with infusion rate as well as length of time[11]
- If intubation required, consider delayed sequence intubation
Disposition
- Admit
See Also
External Links
- EMCrit Podcast - Sympathetic Crashing Acute Pulmonary Edema
- EMCrit Podcast - When to wean the CPAP in SCAPE
- Emergency Medicine Cases Podcast - Acute Congestive Heart Failure
References
- ↑ Maisel AS, Krishnaswamy P, Nowak RM, et al. Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med. 2002;347(3):161-167. doi:10.1056/NEJMoa020233.
- ↑ Carpenter CR et al. BRAIN NATRIURETIC PEPTIDE IN THE EVALUATION OF EMERGENCY DEPARTMENT DYSPNEA: IS THERE A ROLE? J Emerg Med. 2012 Feb; 42(2): 197–205.
- ↑ Januzzi JL, van Kimmenade R, Lainchbury J, et al. NT-proBNP testing for diagnosis and short-term prognosis in acute destabilized heart failure: an international pooled analysis of 1256 patients: the International Collaborative of NT-proBNP Study. Eur Heart J. 2006 Feb. 27(3):330-7.
- ↑ Kragelund C, Gronning B, Kober L, Hildebrandt P, Steffensen R. N-terminal pro-B-type natriuretic peptide and long-term mortality in stable coronary heart disease. N Engl J Med. 2005 Feb 17. 352(7):666-75.
- ↑ Moe GW, Howlett J, Januzzi JL, Zowall H,. N-terminal pro-B-type natriuretic peptide testing improves the management of patients with suspected acute heart failure: primary results of the Canadian prospective randomized multicenter IMPROVE-CHF study. Circulation. 2007 Jun 19. 115(24):3103-10.
- ↑ Clerico A, Giannoni A, Vittorini S, Emdin M. The paradox of low BNP levels in obesity. Heart Fail Rev. 2011;17(1):81-96. doi:10.1007/s10741-011-9249-z.
- ↑ Krauser DG, Lloyd-Jones DM, Chae CU, et al. Effect of body mass index on natriuretic peptide levels in patients with acute congestive heart failure: A ProBNP Investigation of Dyspnea in the Emergency Department (PRIDE) substudy. Am Heart J. 2005;149(4):744-750. doi:10.1016/j.ahj.2004.07.010.
- ↑ Daniels LB, Clopton P, Bhalla V, et al. How obesity affects the cut-points for B-type natriuretic peptide in the diagnosis of acute heart failure. Results from the Breathing Not Properly Multinational Study. Am Heart J. 2006;151(5):999-1005. doi:10.1016/j.ahj.2005.10.011.
- ↑ Haber et al. Bolus intravenous nitroglycerin predominantly reduces afterload in patients with excessive arterial elastance. J Am Coll Cardiol. 1993;22(1):251-257.
- ↑ Hamilton RJ, Carter WA, Gallagher JE. Rapid Improvement of acute pulmonary edema with sublingual captopril. Acad Emerg Med 1996; 3: 205-12.
- ↑ GlobalRPH. Nitroprusside (Nipride®). http://www.globalrph.com/nitroprusside_dilution.htm