We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
Spontaneous pneumothorax
From WikEM
(Redirected from Spontaneous Pneumothorax)
"Spontaneous" essentially refers to all pneumothoraxes of "non-traumatic" etiologies
Contents
Background
- Primary Pneumothorax
- No underlying pulmonary disease
- Secondary Pneumothorax
- With underlying pulmonary disease
- Worse prognosis
Secondary Causes
- Smoking (90%)
- COPD
- Asthma
- Cystic fibrosis
- Necrotizing pneumonia
- Lung abscess
- PCP pneumonia
- TB
- Neoplasm
- Interstitial lung disease
- Connective tissue disease
- Pulmonary infarct
- Catamenial pneumothorax
Clinical Features
- Sudden onset pleuritic chest pain evolving to dull constant ache over days
- Most often occurs at rest, not during exertion
- Tachypnea, hypoxemia, increased work of breathing
- Reduced ipsilateral lung excursion
- Hypotension→ tension pneumothorax
Differential Diagnosis
Pneumothorax Types
- Tension pneumothorax
- Spontaneous pneumothorax
- Traumatic pneumothorax
Shortness of breath
Emergent
- Pulmonary
- Airway obstruction
- Anaphylaxis
- Aspiration
- Asthma
- Cor pulmonale
- Inhalation exposure
- Noncardiogenic pulmonary edema
- Pneumonia
- Pneumocystis Pneumonia (PCP)
- Pulmonary embolism
- Pulmonary hypertension
- Tension pneumothorax
- Idiopathic pulmonary fibrosis acute exacerbation
- Cardiac
- Other Associated with Normal/↑ Respiratory Effort
- Other Associated with ↓ Respiratory Effort
Non-Emergent
- ALS
- Ascites
- Uncorrected ASD
- Congenital heart disease
- COPD exacerbation
- Fever
- Hyperventilation
- Neoplasm
- Obesity
- Panic attack
- Pleural effusion
- Polymyositis
- Porphyria
- Pregnancy
- Rib fracture
- Spontaneous pneumothorax
- Thyroid Disease
Evaluation
Clinically Stable
Defined as having all of the following:
- Resp rate < 24
- Heart rate 60-120 beats per minute
- Normal BP
- SaO2 >90% on room air and patient can speak in whole sentences
Workup
- CXR
- Displaced visceral pleural line without lung markings between pleural line and chest wall
- Upright is best
- Expiratory films DO NOT improve accuracy[1]
- Supine CXR = deep sulcus sign
- CT Chest
- Very sensitive and specific
- Ultrasound
- NO comet tail artifact
- No sliding lung sign
- Bar Code appearance on M-mode (absence of "seashore" waves)
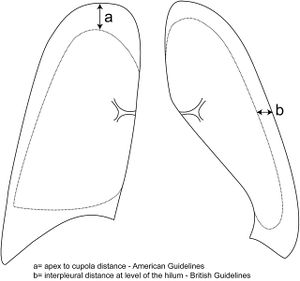
Estimating Pneumothorax Size
- On a conventional, upright posterior-anterior chest radiograph:
- Very small: <1 cm interpleural distance (confined to upper 1/3 of chest) OR only seen on CT
- Small: ≤3cm lung apex to cupola (chest wall apex) on CXR
- Large: >3cm lung apex to cupola (chest wall apex) on CXR
- 3cm apex to cupola measurement is roughly equivalent to 2cm interpleural distance (at the level of the hilum)
- Both roughly correlate with a 50% pneumothorax by volume
Management[2]
Supplemental oxygen (non-rebreather mask) initially for all
Unstable
- Needle decompresion followed by chest tube insertion
Primary Spontaneous Pneumothorax (Stable)
First Episode
- Small AND asymptomatic (no dyspnea)
- Observe on supplemental oxygen (non-rebreather mask) for 6 hours; repeat CXR and discharge if no progression; return in 24 hours for a recheck
- Large OR symptomatic (e.g. dyspnea)
- Aspiration (see below)
- If fail, admit with chest tube to suction for thoracoscopy (VATS)^
- Aspiration (see below)
Recurrent OR Hemopneumothorax
- Admit with chest tube for thoracoscopy (VATS)^
^If thoracoscopy (VATS) is not readily available, chemical pleurodesis through the chest tube
Secondary Pneumothorax (Stable)
- Asymptomatic AND very small (<1 cm interpleural distance)
- Observation with supplemental oxygen; repeat CXR in 12-24 hours
- Asymptomatic AND small
- Chest tube (some centers may choose needle aspiration under ultrasound guidance)
- Observation alone associated with some mortality
- Symptomatic OR large OR bilateral
- Admit all secondary pneumothoraxes
Needle Aspiration of Pneumothorax
- Use thoracentesis or "pig-tail" kit, if available
- Place in 2nd IC space in midclavicular line or 4th/5th IC space in anterior axillary line
- Withdraw air with syringe until no more can be aspirated
- Assume a persistent air leak (failure) if no resistance after 4 liters of air has been aspirated AND the lung has not expanded
- Once no further air can be aspirated:
- Option 1
- Place closed stopcock and secure catheter to the chest wall
- Obtain CXR four hours later
- If adequate lung expansion has occurred, remove catheter
- Following another two hours of observation, obtain another CXR
- If the lung remains expanded, may discharge patient
- Option 2
- Leave catheter in place
- Attached a Heimlich (one-way) valve
- May discharge with follow-up within two days
- Option 1
Adult Chest Tube Sizes
| Chest Tube Size | Type of Patient | Underlying Causes |
| Small (8-14 Fr) |
|
|
| Medium (20-28 Fr) |
|
|
| Large (36-40 Fr) |
|
Disposition
Primary
- See Management section
Secondary
- All admitted (even if small and clinically stable)
Special Instructions
Flying
- Can consider flying 2 weeks after full resolution of traumatic pneumothroax[2]
See Also
References
- ↑ Eur Respir J. 1996 Mar;9(3):406-9
- ↑ 2.0 2.1 "Management of spontaneous pneumothorax: British Thoracic Society pleural disease guideline 2010" British Thoracic Society Guidelines. Thorax 2010;65:ii18-ii31 doi:10.1136/thx.2010.136986 PDF