We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
Pericardial effusion and tamponade
From WikEM
Contents
Background
- Always consider in patient with PEA
- Always consider in patient with myocardial stab wound (80% result in tamponade)
- GSW is less likely to result in tamponade b/c pericardial defect is larger
- Pathophysiology
- Increased pericardial pressure > decreased RV filling > decreased CO
Etiology
- Hemopericardium
- Trauma
- Iatrogenic (misplaced central line)
- Bleeding diathesis
- Ventricular rupture (post-MI)
- Non-hemopericardium
- Cancer - most commonly lung, breast
- Melanoma has predilection for heart
- May be related to radiation, infection, chemotherapy
- Pericarditis
- Infectious
- Uremic (renal failure)
- HIV complications (infection, Kaposi sarcoma, lymphoma)
- SLE
- Post-radiation
- Myxedema
- Cancer - most commonly lung, breast
Differential Diagnosis
Chest pain
Critical
- Acute Coronary Syndromes
- Aortic Dissection
- Cardiac Tamponade
- Pulmonary Embolism
- Tension Pneumothorax
- Boerhhaave's Syndrome
- Coronary Artery Dissection
Emergent
- Pericarditis
- Myocarditis
- Pneumothorax
- Mediastinitis
- Cholecystitis
- Pancreatitis
- Cocaine-associated chest pain
Nonemergent
- Stable angina
- Asthma exacerbation
- Valvular Heart Disease
- Aortic Stenosis
- Mitral valve prolapse
- Hypertrophic cardiomyopathy
- Pneumonia
- Pleuritis
- Tumor
- Pneumomediastinum
- Esophageal Spasm
- Gastroesophageal Reflux Disease (GERD)
- Peptic Ulcer Disease
- Biliary Colic
- Muscle sprain
- Rib Fracture
- Arthritis
- Chostochondirits
- Spinal Root Compression
- Thoracic outlet syndrome
- Herpes Zoster / Postherpetic Neuralgia
- Psychologic / Somatic Chest Pain
- Hyperventilation
- Panic attack
Clinical Features
- Chest pain, shortness of breath, cough, fatigue
- CHF-type appearance
- Narrow pulse pressure
- Friction rub
- Pulsus paradoxus (dec in BP on inspiration)
- Beck's Triad (33% of patients)
- Hypotension, muffled heart sounds, JVD
Evaluation
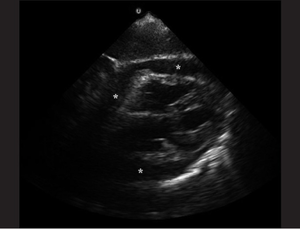
Ultrasound
- Pericardial effusion
- In acute cases, even a relatively small build up of pericardial fluid can lead to hemodynamic compromise
- Diastolic collapse of the right atrium (in atrial diastole)
- Diastolic collapse of the right ventricle
- Plethoric IVC
- Valvular pulsus parodoxus
- Doppler interrogation across the mitral valve will demonstrate exaggerated respiratory variability of transvalvular flow
ECG
- Can be normal
- Tachycardia (bradycardia is ominous finding)
- Electrical alternans
- Low voltage
- All limb lead QRS amplitudes <5 mm or I+II+III<15;[1]
- OR All precordial QRS amplitudes <10 mm or V1+V2+V3<30
CXR
- Enlarged cardiac silhouette
Pulsus Paradoxus
- >10mmHg change in systolic BP on inspiration
Management
Hemorrhagic Tamponade
- Can occur if ECG read as STEMI/NSTEMI and heparin started
- Pericardiocentesis
- Temporizing measure until thoracotomy can be performed
- IVF to increase RV volume and maintain preload
- Medications
Non-hemorrhagic Tamponade
- Pericardiocentesis
- Dialysis for patients with known renal failure
Disposition
- Admit with cardiology/CT surgery consult
See Also
References
- ↑ Mattu A, Brady W. ECGs for the Emergency Physician 2, BMJ Books 2008.