We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
Anemia
From WikEM
Contents
Background
- Affects 1/3 of the world's population
- Most common causes are uterine and GI bleeding
Pathophysiology
4 mechanisms:
- Loss of RBCs by hemorrhage (e.g. GI bleed)
- Increased destruction (SCD, hemolytic anemia)
- Impaired production (iron deficiency, folate deficiency, B12 deficiency, aplastic anemia/myelodysplastic syndrome)
- Dilutional (rapid IVF infusion)
Clinical Features
General Anemia Symptoms
- Most patients begin to be symptomatic at ~7gm/dL
- Weakness, fatigue, lethargy, dyspnea on exertion, palpitations
- Skin, nail bed, mucosal pallor
- Widened pulse pressure
- Jaundice, hepatosplenomegaly (hemolysis)
- Peripheral neuropathy (B12 deficiency)
Differential Diagnosis
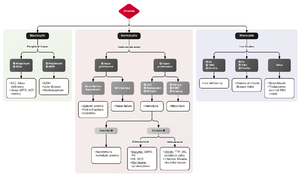
Anemia
RBC Loss
- Hemorrhage
RBC consumption (Destruction/hemolytic)
- Hereditary
- Acquired
- Microangiopathic Hemolytic Anemia (MAHA)
- Autoimmune hemolytic anemia
Impaired Production (Hypochromic/microcytic)
- Iron deficiency
- Anemia of chronic disease
- Thalassemia
- Sideroblastic anemia
Aplastic/myelodysplastic (normocytic)
Megaloblastic (macrocytic)
- Vitamin B12/folate deficiency
- Drugs (chemo)
- HIV
Evaluation
Severe anemia is defined as a hemoglobin level of 5 to 7 g/dL with symptoms of hypoperfusion including lactic acidosis, base deficit, shock, hemodynamic instability, or coronary ischemia[1]
Acute Anemia
Assess for any signs of bleeding or trauma before considering other causes of chronic anemia.
Chronic Anemia
CBC for evaluation, look at MCV
- Microcytic: Iron Levels, Reticulocyte Count, Ferritin, TIBC
- Macrocytic: Folate Level, B12 Level, Reticulocyte Count
Microcytic Anemia (<81 fL)
- RDW high -> evaluate Ferritin, which is a measurement of iron storage
- Ferritin low: Iron deficiency anemia
- Ferritin normal: Anemia chronic disease or sideroblastic anemia (e.g. lead poisoning)
- RDW normal
- RBC count low: Anemia chronic disease, hypothyroidism, Vitamin C deficiency
- RBC count nl or high: Thalassemia
Normocytic Anemia (81-100 fL)
- Retic count normal
- RDW normal: Anemia chronic disease, anemia of renal insufficiency
- RDW high: Iron, Vit B12, or folate deficiency
- Retic count high
- Coombs Positive: Autoimmune cause
- Coombs negative: G6PD, SCD, spherocytosis, microangiopathic hemolysis
Macrocytic Anemia (MCV>100 fL)
- RDW high: Vit B12 or folate deficiency
- RDW normal: ETOH abuse, liver disease, hypothyroidism, drug induced, myelodysplasia
Management
- Consider if patient is symptomatic, hemodynamically unstable, hypoxic, or acidotic
- Using a restrictive transfusion strategy (transfusing <6-8) has found to be beneficial, as liberal transfusion strategy (transfusing <10) not showing any benefit and has shown harm
- GI bleeds using restrictve transfusion strategy saw a decreased mortality and rebleed rate
- Always draw labs necessary for diagnosis prior to transfusing
- 1 unit PRBCs should raise the Hgb by 1gm/dL
Iron-deficiency anemia
- PO: Ferrous sulfate 325mg (65mg elemental iron) with Vitamin C (to aid in absorption)
- IV: Ferrous Sucrose 300mg in 250mL NS over 2hrs
See Also
External Links
References
- ↑ Posluszny JA Jr, Napolitano LM. How do we treat life-threatening anemia in a Jehovah's Witness patient? Transfusion. 2014;54(12):3026-3034