Nutrition/Physical Activity/Obesity
Download this page [PDF – 652K]
Progress has been mixed in this Winnable Battle.
The proportion of infants who are breastfed at 6 months has been increasing. This indicator has exceeded the original Winnable Battles target of 50% by 3.6%.
Physical activity helps prevents heart disease, stroke, type 2 diabetes, depression, and some cancers. In 2008, 43.5% of adults met the aerobic Physical Activity Guidelines for Americans. That percentage increased to 49.8% in 2015.
For children and adolescents aged 2 – 19 years, the prevalence of obesity has remained fairly stable at about 17% and affects approximately 12.7 million children and adolescents. The prevalence of obesity among children aged 2 to 5 years decreased significantly from 13.9% in 2003 – 2004 to 8.4% in 2011 – 2014. Children who have obesity are more likely to become adults with obesity. For adults, the prevalence of obesity has remained high at 37.7% in 2013 – 2014. Adult obesity is associated with a number of serious health conditions including heart disease, diabetes, metabolic syndrome, and cancer.
Trends in Nutrition / Physical Activity / Obesity Winnable Battle Indicators
Trends in the prevalence of obesity among U.S. children and adolescents aged 2 – 19, 2006 – 2014
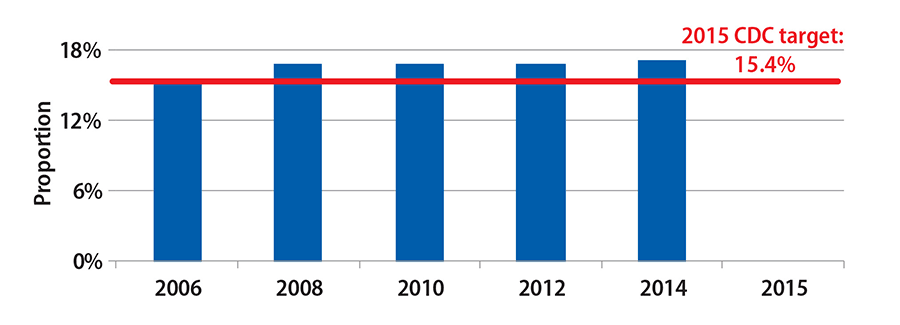
Source: National Health and Nutrition Examination Survey (NHANES)
Trends in the percentage of infants who are breastfed at 6 months, 2006 – 2013
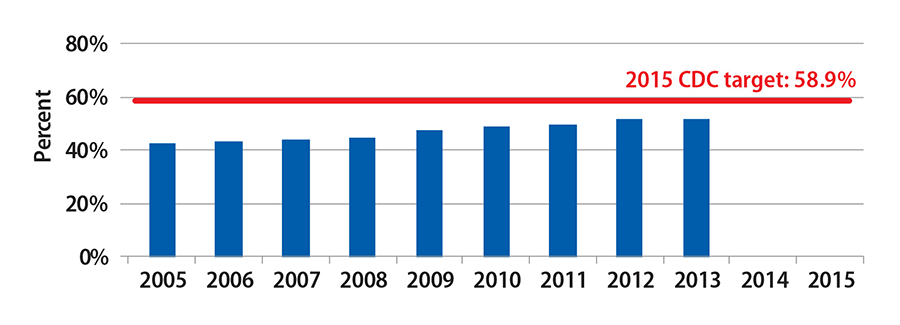
Source: National Immunization Survey (NIS)
Considerations in Choosing Nutrition / Physical Activity / Obesity as Winnable Battle
- Obesity is common, serious and costly.
- Childhood obesity has both immediate and long-term effects on health and well-being for individuals and the nation.
- Breastfeeding is the optimal form of nutrition for infants, and provides numerous health benefits for both children and mothers.
- Regular physical activity helps improve overall health and fitness, and reduces the risk for many chronic diseases including type 2 diabetes, heart disease, high blood pressure, stroke, certain cancers and depression.
State Spotlight: Alabama Supports Breastfeeding Friendly Environments
The Alabama Breastfeeding Committee (ABC) works to ensure that community breastfeeding services are an essential component of healthcare for all Alabama families. Through coordination and partnering, ABC implemented local lactation groups in each of the state’s perinatal regions to address breastfeeding issues at a grassroots level and provide education to local health professionals. Through funding from the CDC and the United States Breastfeeding Committee, ABC and the Alabama Department of Public Health established breastfeeding support groups in birthing facilities, increased the number of Baby Cafés® across the state, provided baby scales to support groups, facilitated provider education, and supported certification or licensing of lactation care providers.
Challenges / Obstacles
- Childhood obesity is a complex societal issue. The main causes of excess weight in youth are similar to those in adults, including individual causes such as behavior and genetics. Behaviors can include dietary patterns, physical activity, inactivity, medication use, and other exposures. Additional contributing factors in our society include the food and physical activity environment, education and skills, and food marketing and promotion.
CDC Contributions in Nutrition / Physical Activity / Obesity Winnable Battle Initiative
This team is collaborating across the agency and with federal partners including the Food and Drug Administration, the Office of the Surgeon General, the General Services Administration (GSA) and Let’s Move on focused and cross-cutting initiatives to improve nutrition, physical activity, obesity, and breastfeeding outcomes.
Promoting improved nutrition standards and access to healthier foods for children and adults
- CDC supports work in all 50 states and D.C. in ensuring healthier foods are available in early care and education (ECE) settings for children aged 0 to 5 years by implementing improved standards and offering child care provider training. Between 2010 and 2015, 26 states made 455 improvements to nutrition standards in their state licensing regulations.
- As of June 2016, over 1,500 ECE programs serving over 145,000 young children participated learning collaborates designed to help them meet high priority nutrition standards.
- As of July 2016, over 19,800 ECE providers pledged to meet best practices for food, beverages, breastfeeding support, physical activity, and screen time through participation in Let’s Move Child Care (LMCC) serving over 1 million children.
- CDC is leveraging opportunities provided by the new Every Student Succeeds Act to strengthen nutrition and physical education activities and programs in schools.
- CDC works to improve the school nutrition environment with partners such as states, USDA and Let’s Move.
- Between 2008 and 2014 there has been a 23% increase in the number of schools that did not sell less healthy food and drinks (School Health Profiles).
- Between 2000 and 2014 there was a 29% increase in the number of schools offering vegetables, and a significant increase in the number of schools implementing strategies to reduce sodium in meals (School Health Policies and Practices Study).
- CDC has supported the Let’s Move Salad Bars to Schools initiative of the First Lady and as of July 2016 there are over 4,600 salad bars granted nationally, serving over 2.3 million kids.
- CDC played a key role in drafting standards, Smart Snacks in Schools, and implementation plans for other components of the Healthy Hunger Free Kids Act.
- CDC published Healthy Hunger Free Kids Act resource materials, including
- Increasing Access to Drinking Water in Schools Toolkit,
- Putting Local School Wellness Policies into Action and
- Competitive Foods and Beverages in Schools: A State Policy Analysis.
- CDC published the School Health Guidelines to Promote Healthy Eating and Physical Activity in 2011 and has trained school personnel in all 50 states on the guidelines. CDC’s School Health Index, an online school health and safety assessment and planning tool, has been adopted by the Alliance for a Healthier Generation and Action for Healthy Kids.
- CDC supported the adoption and use of the 2011 Food Service Guidelines (FSG).
- CDC led the development of FSG resources including tools to enable FSG use, case reports, and research.
- CDC works with the National Prevention Council to promote implementation of FSG among its members, representing 20 federal departments, agencies and offices.
- CDC co-led the creation of the Food Service Guidelines Collaborative, which consists of 25 partners representing federal agencies, national non-profits, universities, and state health departments committed to normalizing the availability of more healthful foods in key settings.
- An update to the 2011 FSG was led by HHS / CDC and the General Services Administration (GSA) to align food and nutrition standards with the Dietary Guidelines for Americans, 2015 – 2020. The updated FSG are under review and expected to be released in late 2016.
- Through the CDC Sodium Reduction in Communities Program (SRCP), ten grantees across the country are working with partners to increase accessibility of healthier food options, focusing on lower sodium products. For example, San Antonio Metropolitan Health District, an SRCP grantee, worked with a large private worksite cafeteria to implement sodium reduction strategies, which resulted in a 22% reduction in average sodium content across the menu.

Promoting increased physical activity in communities, schools, and workplaces
- CDC collaborated with the Surgeon General to develop and release Step It Up! The Surgeon General’s Call to Action to Promote Walking and Walkable Communities, which recognizes the importance of physical activity for people of all ages and abilities. Released in September 2015, the initiative calls on Americans to be more physically active through walking and calls on the nation to better support walking and walkability for better health. A status report reflecting progress of activities will be released Fall 2016.
- CDC collaborated with CDC Foundation, Hartsfield- Jackson Airport, and the Kresge Foundation to develop and release, “Promoting Airport Walking: A Guide” in May 2016. The guide helps airport managers and staff to encourage healthy walking habits in airports.
- On June 16, 2016, CDC released the MMWR “Disparities in Adolescents’ Residence in Neighborhoods Supportive of Physical Activity — United States, 2011 – 2012” which assessed whether the proportion of adolescents who live in neighborhoods supportive of physical activity varied between populations. Results indicated about 2 / 3 of adolescents 10 – 17 years lived in neighborhoods that support physical activity. The proportion was lower among adolescents who were non-Hispanic black or Hispanic, overweight or obese, from households with lower socioeconomic status, or in rural areas.
- A Vital Signs-like MMWR and graphic, “Physical Inactivity Among Adults 50 Years and Older — United Sates, 2014,” was released September 2016. CDC also hosted a town-hall meeting and conducted 16 calls and meetings reaching 44 partner groups.
- CDC developed the Comprehensive School Physical Activity Program (CSPAP) Guide to assist schools and school districts to develop, implement, and evaluate comprehensive physical activity programs. School faculty in all 50 states have been trained to implement a CSPAP and CDC has developed an eLearning series to facilitate additional trainings.
- CDC published a report that summarized the findings from a roundtable of physical activity and measurement experts convened by CDC and American College of Sports Medicine in 2014. This report identified an overarching strategy to develop a national plan for physical activity surveillance similar to the U.S. National Physical Activity Plan. The purpose of the surveillance plan would be to enhance coordination and collaboration within and between sectors, such as transportation and public health, and to address identified strategic priorities.
- CDC supports work in all 50 states and D.C. in supporting implementation of physical activity standards in early care and education (ECE) settings for children aged 0 to 5 years by implementing improved standards and offering child care provider training.
- Between 2010 and 2015, 26 states made 222 improvements to physical activity standards in their state licensing regulations.
- As of June 2016, over 1,500 ECE programs serving over 145,000 young children participated in a learning collaboratives designed to help them meet high priority obesity prevention standards, including physical activity.
- Between February 2014 and June 2016, nearly 3,000 ECE providers completed online professional development training on physical activity standards developed by Penn State University’s Better Kid Care Program and CDC.
Increasing breastfeeding rates by improving breastfeeding support
- More than 18% of all births in the U.S. occur at Baby- Friendly hospitals, up from less than 2% in 2007. This achievement surpasses the Healthy People 2020 goal of 8.1%.
- The CDC-funded Best Fed Beginnings project contributed to the acceleration of Baby-Friendly designated U.S. hospitals. As of July 2016, 72 of the 89 Best Fed Beginnings Hospitals achieved Baby-Friendly designation, the global standard for hospital care to support breastfeeding.
- CDC funded the EMPower Breastfeeding Initiative that is assisting 93 hospitals from 24 states to become Baby-Friendly. As of July 2016, three EMPower hospitals achieved Baby-Friendly designation. Two of these hospitals were in Arkansas, the first hospitals in the state to achieve Baby-Friendly designation.
- Breastfeeding rates continue to rise. More than half of infants born in 2013 were breastfed at six months.
- From 2006 through 2016, the number of International Board Certified Lactation Consultants increased from 2.1 to 3.8 per 1,000 live births. Professional breastfeeding support can help mothers start and continue breastfeeding to meet personal goals and national health recommendations.
- From 2007 to 2015 the national average hospital quality score from the CDC Maternity Practices in Infant Nutrition and Care (mPINC) survey increased from 63 to 79 out of 100. Breastfeeding duration continues to increase as CDC assists more hospitals to adopt evidence-based maternity care practices as measured in the mPINC survey.
- Page last reviewed: November 8, 2016
- Page last updated: November 8, 2016
- Content source:


 ShareCompartir
ShareCompartir