Food Safety
Illness due to E. coli has decreased significantly; there is still room to make additional progress on E. coli and other foodborne infections, such as Salmonella.
Each year, 1 in 6 Americans gets sick by consuming contaminated foods or beverages.
Medical and industry costs of these illnesses exceed $15.5 billion. CDC estimates that reducing foodborne infections by just 10 percent would keep approximately 5 million Americans from getting sick each year.
Salmonella infections result in more hospitalizations and deaths than any other bacteria found in food and incur approximately $365 million in direct medical costs annually.
Trends in Food Safety Winnable Battle Indicators
Trends in the rate of infections caused by Salmonella, 2006 – 2015
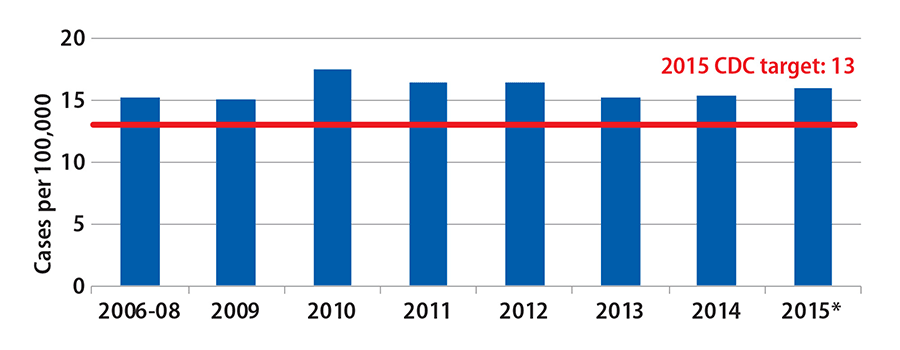
Source: Foodborne Diseases Active Surveillance Network (FoodNet)
*2015 data are preliminary
Trends in the rate of infections caused by Shiga toxin-producing Escherichia coli (STEC) O157:H7, 2006 – 2015
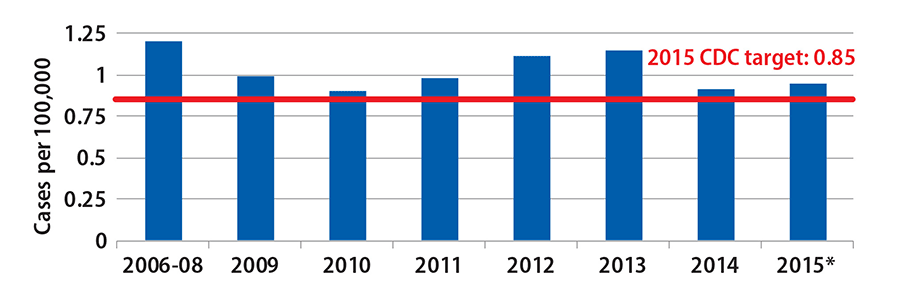
Source: Foodborne Diseases Active Surveillance Network (FoodNet)
*2015 data are preliminary
Considerations in Choosing Food Safety as Winnable Battle
- Foodborne illness is a common, costly — yet preventable — public health problem.
- Effective strategies exist to decrease the foodborne illness health burden.
- The Food Safety Modernization Act passed in 2011 underscored the importance of addressing food safety as a CDC Winnable Battle.
Challenges / Obstacles
- Declining state and local resources have impaired the ability to reduce food-related illness outbreaks.
- Changes in food production and supply, including more imported foods.
- New and emerging bacteria, toxins and antibiotic resistance.
- Unexpected sources of foodborne illness, such as ice cream and raw sprouted nut butter.
The Effect of AMD on Food Safety
Since CDC began applying advanced molecular detection (AMD) and enhanced epidemiology methods for nationwide surveillance of Listeria infections, CDC has been able to detect seven clusters of illness that would not have been detected by the older methods. The number of cases linked to a food source increased from 13 in 2013 to 103 by the end of 2015. One example is a Listeria outbreak that affected at least 32 people in 11 states between October and December 2014. Seven of those people died. Using whole genome sequencing, CDC was able to identify the illnesses as a cluster one week faster than would have occurred with the older methods. CDC worked with state and local health departments, the Food and Drug Administration, and food industries to identify prepackaged caramel apples as the source of the outbreak. Investigation partners were then able to take action to inform the public and get caramel apples off the shelves to keep more people from becoming ill.
CDC Contributions in Food Safety Winnable Battle
The Food Safety Winnable Battles team transformed its approach from outbreak response to combat foodborne illnesses to a proactive, comprehensive program to improve food safety.
Detect and investigate outbreaks to stop the spread and learn how to prevent the next one
- Since CDC adopted whole genome sequencing (WGS) for Listeria outbreaks, the median number of Listeria illnesses per outbreak has declined by 50%. In FY 2015, outbreak investigations identified caramel apples and ice cream as two food sources of Listeria, neither of which had previously been considered as an important source of this severe infection. Those industries are adopting more stringent control measures as a result.
- More than half of all foodborne illness outbreaks are associated with restaurants, banquet halls, and schools and other institutions. The environmental factor data collected through the National Environmental Assessment Reporting System (NEARS) will be used to help determine the causes of outbreaks in these settings, improve outbreak response efforts, and prevent future outbreaks. In 2014, for 62 out of 110 (56%) closed outbreaks, the underlying environmental factors were identified. As of October 2016, 21 health departments (13 state and eight city / county) are participating in NEARS.
Drive policy and prevention with data and analyses
- CDC data and the results of many CDC-led investigations were formative in shaping the final FDA regulations for the produce safety and preventive controls rules mandated by the Food Safety Modernization Act. CDC data were also used by USDA for its performance standards, further limiting the frequency of Salmonella allowed in poultry carcasses, parts, and ground poultry. Ongoing CDC surveillance will be central to tracking the impact of these new prevention measures.
- To enable tailored prevention efforts targeted at specific serotypes, CDC made available online the Atlas of Salmonella in the United States, 1968 – 2011, which summarizes surveillance data on 32 types of Salmonella isolates from people, animals, and other sources. The information is organized by demographic, geographic and other categories and enables the reader to compare trends in Salmonella serotypes by following their spread or decline over time and location.
- An analysis published in 2016 found that PulseNet, the national laboratory network that detects foodborne disease outbreaks, prevents an estimated 270,000 illnesses every year from the three most common causes of foodborne illness: Salmonella, E. coli O157 and Listeria monocytogenes. As a result, an estimated $507 million is saved every year in medical costs and lost productivity. Outbreak investigations supported by PulseNet help identify problems in food production and distribution systems — for example, ground beef, nut butter, and cookie dough. These investigations have led to changes in food production and new federal recommendations – all of which are making our food safer to eat. Analyses have also found that PulseNet speeds up identification and recalls of tainted foods.

- Illustrating the return on investment in food safety programs, CDC estimates prevention of a single fatal case of E. coli O157 infection saves $7 million. In addition, an analysis concluded that the Colorado PulseNet system would recover all its costs if it averted as few as five cases of E. coli O157 infection annually.
- Using data from CDC research showing that kitchen manager certification is consistently linked to food safety, CDC staff was successful in petitioning the Conference for Food Protection (CFP) to strengthen the kitchen manager certification provision in the Food and Drug Administration’s (FDA) Food Code. CFP is an influential organization and is the primary means through which the FDA Food Code is revised. The FDA Food Code greatly influences state and local food safety codes and policies, and CDC strongly encourages its adoption. The strengthened kitchen manager certification provision will be in the 2017 FDA Food Code.
- CDC staff led the effort to develop food safety guidelines for the Federal Food Service Guidelines. These guidelines are developed by HHS and GSA for federal food service contractors, and greatly influence food service contractors’ actions. Again, data from CDC research was used to support the inclusion of a kitchen manager certification provision, in addition toother important food safety provisions.
Work with partners (public health, industry, consumer groups, etc.) to share food safety data and information to improve practices
- CDC highlighted the focus on preventing foodborne illness through four Vital Signs reports, emphasizing pathways and partnerships that can improve prevention of specific foodborne infections and identifies persons who are particularly susceptible, like the very young, the elderly, and those with impaired immune systems. In 2015, the CDC Foundation reached out to all companies through Business Pulse, to encourage them to improve food safety in the workplace and make food safety a part of company culture.
- CDC partnered with the country’s largest grocery retailer to decrease pathogens such as Salmonella and Campylobacter in chicken products provided by its suppliers. The program requires the retailer’s poultry suppliers to implement holistic controls from farm to final product and is designed to significantly reduce potential contamination levels, including fresh whole chickens and chicken parts. It also requires suppliers to validate that the measures they have implemented are effective through specialized testing.
- CDC educates retail food safety stakeholders (food retailers, food safety program staff, and food safety researchers) to enable improved food safety practices.
- A CDC-funded study on “Restaurant Manager and Worker Food Safety Certification and Knowledge” (December 2014 Foodborne Pathogens and Disease) found that certified managers have better food safety knowledge and improved food safety practices in their establishments.
- Researchers also identified gaps in restaurant policies and practices concerning ill workers (e.g., lack of policies requiring sick workers to stay home), that if addressed, could help prevent foodborne illness outbreaks, according to a CDC-funded study on “Managerial Practices Regarding Workers Working While Ill” (January 2015 Journal of Food Protection).
- CDC also provides training to help professionals identify the root causes of foodborne illness outbreaks. Since 2014, more than 4,400 people (1,005 in the past year) have registered for NCEH’s free, innovative, online training for food safety and environmental health professionals on collecting environmental factor data during foodborne illness outbreak investigations.

Stop the spread of antibiotic resistant bacteria
- In August 2015, CDC released the 2013 National Antimicrobial Resistant Monitoring System (NARMS) Annual Human Isolates Report to aid in better understanding trends in antibiotic resistance among Salmonella, Shigella, and Campylobacter, E.coli O157, and Vibrio species (other than V. cholerae). Findings from this report can help doctors prescribe effective treatments for these infections and aid public health officials in more quickly investigating outbreaks from these germs. In FY2016, CDC is awarding $30 million to states and cities to track, investigate and prevent foodborne disease, $14 million of which is funded from the Antibiotic Resistance (AR) Initiative in support of the National Action Plan for the Combating Antibiotic-Resistant Bacteria. These grants will help states and cities protect Americans from foodborne outbreaks and improve laboratory-based surveillance for foodborne germs, particularly including antibiotic-resistant bacteria. The grants will support:
- Training to ensure that state and local health departments have the ability to use advanced technologies, including whole genome sequencing which will make it possible to detect and respond to outbreaks earlier. Whole genome sequencing also allows us to detect known markers of antibiotic resistance and is an essential tool in combatting antibiotic resistance.
- Thirty-two whole genome sequencers for state public health laboratories to improve detection of and surveillance for antibiotic-resistant intestinal bacteria found in ill people.
- Page last reviewed: November 9, 2016
- Page last updated: November 9, 2016
- Content source:


 ShareCompartir
ShareCompartir