HIV in the United States
Download this page [PDF – 365K]
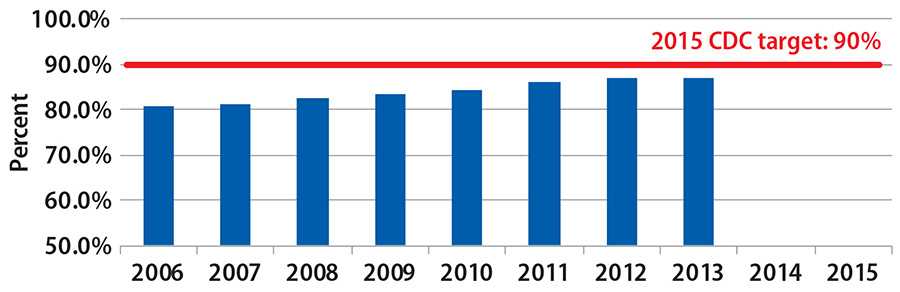
The percentage of people living with HIV who know their status is steadily increasing toward the 90% target.
- CDC estimates that 1,242,000 persons aged 13 years and older were living with HIV infection at the end of 2013, including 161,200 (13.0%) who are unaware of their infection.
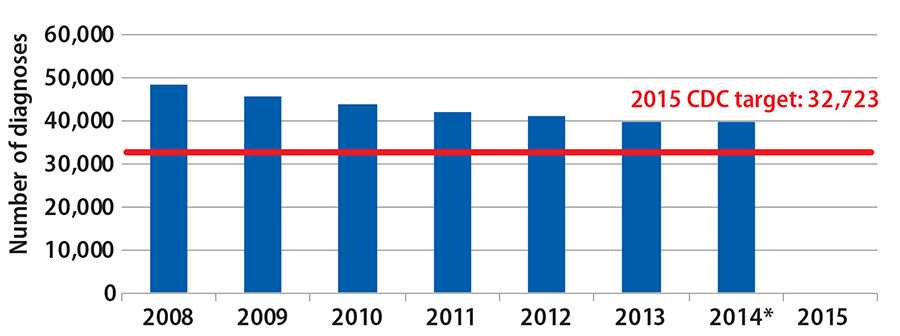
- In 2014, an estimated 39,718 people received a diagnosis of HIV infection. The annual number of diagnoses declined by 17.9% from 2008 to 2014.
Trends in HIV Disparities
HIV Diagnosis by Race / Ethnicity, 2005 – 2014
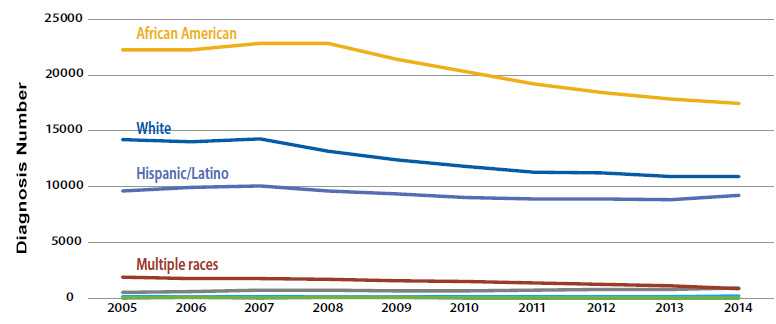
Source: CDC Fact Sheet: Trends in U.S. HIV Diagnoses, 2005 – 2014.
Note: Data are not adjusted for reporting delays.
HIV Diagnosis among MSM age 13 – 24 , by Race / Ethnicity, 2005 – 2014
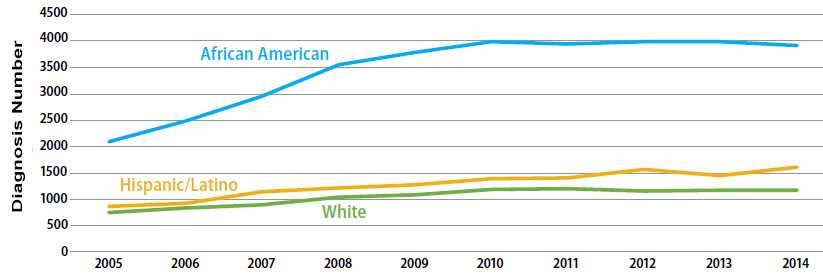
2015 National HIV Prevention Conference, CDC HIV surveillance data
Trends in HIV Winnable Battle Indicators
Considerations in Choosing HIV in the United States as Winnable Battle
- Serious health disparities among populations and risk groups:
- In 2008, Africans Americans accounted for 40% of people living with HIV and Hispanics accounted for 20%, respectively.
- Also in 2008, almost 52% of people living with HIV were infected through male-to-male sexual contact and 16% through injection drug use.
- Estimated lifetime cost of more than $400,000 per person for direct medical care.
- Opportunity to collaborate and leverage federal initiatives and partnerships including National HIV / AIDS Strategy (released July 2010 and updated in July 2015 to 2020), and the Presidential Advisory Council on HIV / AIDS.
State Spotlight: New Jersey & Linkage to Care
With CDC’s support, the New Jersey Department of Health is working to quickly link people with newly diagnosed HIV to care, maintain the continuity of their care, and help them adhere to their HIV medications.
To accomplish this, health department staff use fourth-generation HIV testing technology that can detect acute HIV infection, and then quickly connect people who test positive to HIV prevention “patient navigators.” These professionals are embedded in infectious disease practices and other clinics statewide, and can help people obtain a second confirmatory test and get linked to HIV care within 24 hours of diagnosis or on the next business day. Once people are receiving care, patient navigators can also help them access the prevention services and other support they need to adhere to their medications and protect others from infection.
Challenges / Obstacles
- HIV and AIDS remain a persistent problem for the United States and countries around the world.
- Gay, bisexual, and other men who have sex with men (MSM) of all races and ethnicities remain the population most profoundly affected by HIV in the U.S.
- In the United States, the burden of HIV and AIDS is not evenly distributed across states and regions. The rates of HIV and AIDS diagnoses are higher in the South.
- Too many people living with HIV are not receiving ongoing care and achieving viral suppression.
- Not enough providers and individuals know about effective, new prevention tools, including prevention medications.
CDC Contributions in CDC Winnable Battle
Since 2010, CDC has adopted a high-impact prevention (HIP) approach aimed at identifying and implementing cost-effective and scalable interventions and aligning them with the geographic and demographic burden of HIV infection. CDC expanded efforts to maximize the percent of people with HIV who have suppressed viral load by improving diagnosis, linkage and retention in care, and antiretroviral provision and adherence. CDC also has led a national shift in the use of data for program improvement, public accountability, and public health action by implementing a number of changes aimed at increasing state health department and other CDC grantee use of data for program improvement.
Improved awareness and diagnosis of HIV
- CDC has expanded its testing efforts, especially focusing on communities that have a high burden of HIV infection among African Americans and Hispanics.
- CDC has developed recommendations on emerging testing technologies, including antigen/antibody combination tests (4th generation), to enable earlier diagnosis and prompt linkage to care.
- Through its Act Against AIDS (AAA) initiative, CDC raises awareness among patients, providers, and the public about HIV. Collectively, AAA efforts have reached millions of people through extensive ad placement, social media engagement, provider information kits and meetings, conferences and trainings. In December of 2015, CDC launched the AAA – Doing IT media campaign, which is designed to motivate all adults to get tested for HIV and know their status.
- CDC provides tools to medical providers to support increased testing and increased implementation of CDC’s HIV testing recommendations.
Maximizing Viral Suppression
- Viral suppression not only improves health outcomes for people living with HIV, it also prevents HIV transmission.
- In recognition of the benefits of early treatment, and thus the need for immediate linkage to HIV medical care for all persons newly diagnosed with HIV, CDC changed its linkage to care goal from within three months of diagnosis to linkage to care within one month of diagnosis.
- CDC and our state partners are increasingly using surveillance data to identify HIV-infected persons not in HIV care and target efforts to get these persons back in care and virally suppressed. In 2015, CDC initiated a demonstration project to support efforts to improve state’s ability to use these “data to care” strategies to achieve higher viral suppression rates.
- CDC, in collaboration with partners, published Recommendations for HIV Prevention with Adults and Adolescents with HIV in the United States, 2014 which update and expand recommendations from 2003. The updated recommendations address recent advances in biomedical, behavioral and structural interventions and are directed to a broad range of health professionals and organizations focused on optimizing health outcomes for people with HIV and reducing their risk of exposing others to HIV.
- In 2015, 44 states and D.C. (up from 42 states in FY2014) required reporting of all CD4 and viral load values to health departments for surveillance purposes, which supports CDC’s emphasis on using data to track improvements in viral suppression rates.
Expanding the utilization of new prevention tools
- In 2014, CDC updated its Compendium of Evidence-Based Interventions which is divided into three chapters: Linkage to, Retention in, and Reengagement in HIV Care, Medication Adherence, and Risk Reduction. The updated Compendium provides a comprehensive list of up-to-date, scientifically proven, HIV behavioral interventions that reduce sexual or injection risk behaviors that can be used to guide programmatic planning throughout the U.S. CDC updates the Compendium annually with new best practices and interventions.
- In May 2014, the U.S. Public Health Service and CDC released the first comprehensive clinical practice guidelines for PrEP, which is a way for people who do not have HIV but who are at substantial risk of getting it to prevent HIV infection by taking a pill every day.
- Not many providers know about PrEP (Pre-Exposure Prophylaxis), so CDC is educating clinicians about the potential of PrEP as a powerful, new prevention tool by: creating and supporting PrEPline, a consultative telephone service to support clinicians who have questions; developing medical provider resource kits and medical education courses; and sharing medical provider screening tools.
- In 2015, CDC funded a demonstration project to increase the update of PrEP in MSM and transgender persons at substantial risk of acquiring HIV.
- To raise general awareness about PrEP, CDC has developed materials for the public and incorporated PrEP information into relevant communication campaign materials.
Using Data to Inform Public Health Action
- CDC revised the algorithms for allocating funding to health departments for HIV prevention programs and surveillance. The new funding approach better aligns resources to reflect the geographic burden of HIV today, so that those areas with the greatest burden of disease also receive proportionately more support.
- To meet the needs of national, state, and local partners as well as the general public, CDC has created an interactive platform for accessing data about HIV, viral hepatitis, sexually transmitted diseases (STDs), and tuberculosis (TB). The NCHHSTP Atlas is the one-stop shop for CDC’s most recent surveillance data on HIV, viral hepatitis, STDs, and TB. The Atlas provides access to more than 10 years of the most essential CDC data for these diseases at the national, state, and county levels, and by populations. The Atlas can also be used to see disease trends over time and the burden of these diseases in various communities.
- Page last reviewed: November 28, 2016
- Page last updated: November 28, 2016
- Content source:


 ShareCompartir
ShareCompartir