Preventing Tooth Decay

The Problem
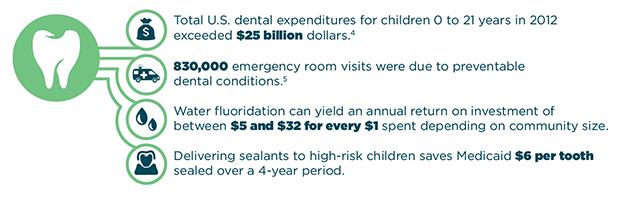
One in five people have untreated tooth decay which can lead to pain and infection and ultimately to problems speaking, eating, working, and playing. When tooth decay in very young children requires extensive treatment under general anesthesia in a hospital operating room, costs can increase by thousands of dollars. Timely delivery of fluorides and dental sealants to at-risk people reduces tooth decay and treatment costs. Residence in a fluoridated community also can reduce the percentage of young children receiving dental treatment in a hospital operating room.3
What Can Be Done?
- Fluoride varnish re-mineralizes weakened tooth enamel and prevents almost 40 percent of cavities in primary teeth.6 Experts recommend that all infants and children receive fluoride varnish starting when the first tooth erupts.7,8 Integrating preventive dental care into well child visits can magnify the community impact of the intervention by increasing the number of children receiving fluoride varnish.
- Dental sealants provide a physical barrier on the chewing surfaces of permanent molars and prevent over 80 percent of cavities 2 years after placement.9 Experts recommend sealant programs administered through schools to increase the number of children who receive sealants. These programs typically target schools attended by a large number of children at high risk for tooth decay. Studies indicate that delivering sealants to high-risk children can offer Medicaid a positive return on investment at 2 years.10
- Community water fluoridation is a safe and effective way to provide optimal levels of fluoride to prevent tooth decay. Experts recommend community water fluoridation to reduce tooth decay among children and adults. Children living in communities initiating water fluoridation have 2.25 fewer decayed teeth11 and lower treatment costs3,12,13 than similar children living in non-fluoridated communities. For the general population, there is an estimated annual return on investment for fluoridated communities between $5 and $32 per person depending on the size of the community.14
Resources for Action
Public Health Practitioners
Additional resources for state health officials, local health department officials, or other public health practitioners:
- CDC Division of Oral Health : The CDC’s Division of Oral Health homepage features the latest scientific research, guidelines, and recommendations.
- Health Investments that Pay Off: Strategies to Improve Oral Health : A policy brief prepared by the National Governors Association to inform state decision makers about evidence-based interventions that can improve population health outcomes and health care quality and reduce the cost of health care as part of an overall agenda for state health care transformation.
- Community Preventive Services Task Force Oral Health Recommendations and Findings : The Community Preventive Services Task Force recommendations and findings for oral health interventions based on a systematic review of available studies.
- Association of State and Territorial Dental Directors Best Practices Approach Report on Community Water Fluoridation : A report on water fluoridation describing the public health strategy, strength of evidence, and current examples of implementation.
- Association of State and Territorial Dental Directors Best Practices Approach Report on School-based Dental Sealant Programs : A report on school-based dental sealant programs describing the public health strategy, strength of evidence, and current examples of implementation.
- Association of State and Territorial Dental Directors Research Brief "Fluoride Varnish: an Evidence-Based Approach" : A research brief presenting the best available evidence to help professionals design and evaluate community-based programs that use fluoride varnish.
- Children's Dental Health Project Issue Brief on Dental Sealants : An issue brief that explores factors influencing the implementation of school sealant programs.
- Children's Dental Health Project Resources on Fluoride and Water Fluoridation : Information and links to additional resources on fluoride and community water fluoridation.
State Decision Makers
Additional resources for governors, health policy advisors, legislators, budget officers, or other decision makers:
- Community Preventive Services Task Force Oral Health Recommendations and Findings :The Community Preventive Services Task Force recommendations and findings for oral health interventions based on a systematic review of available studies.
- Health Investments that Pay Off: Strategies to Improve Oral Health :A policy brief prepared by the National Governors Association to inform state decision makers about evidence-based interventions that can improve population health outcomes and health care quality and reduce the cost of health care as part of an overall agenda for state health care transformation.
- CDC Public Health Grand Rounds: Community Water Fluoridation: A Vital 21st Century Public Health Intervention : A presentation of the public health impact, communications challenges, and innovative state approaches to community water fluoridation.
- Children's Dental Health Project Resources on Fluoride and Water Fluoridation : Information and links to additional resources on fluoride and community water fluoridation.
- The Pew Center on the States report: Falling Short; Most States Lag on Dental Sealants :A report on progress in all 50 states and D.C. to meet Pew benchmarks for prevention and state efforts to improve access to sealants for low-income children.
- Fluoride Legislative User Information Database (FLUID) :A comprehensive database of U.S. legal decisions and policies regarding community water fluoridation.
- Children’s Dental Health Project: Presentation on Implementation of the Pediatric Dental Benefit in the Affordable Care Act : A presentation on the implementation of the pediatric dental benefit in the Affordable Care Act.
State Medicaid Officials
Additional resources for state Medicaid programs:
- Medicaid State Dental Association : Information about evidence-based Medicaid/Children's Health Insurance Program oral health best practices and policies.
- Health Investments that Pay Off: Strategies to Improve Oral Health : A policy brief prepared by the National Governors Association to inform state decision makers about evidence-based interventions that can improve population health outcomes and health care quality and reduce the cost of health care as part of an overall agenda for state health care transformation.
- The Children's Dental Health Project "Dental Visits for Medicaid Children: Analysis and Policy Recommendations" : A policy brief examining the various factors related to a recent increase in dental visits for children enrolled in Medicaid, how these children received care, and policy recommendations to further improve access to and quality of dental care for underserved populations.
- The Children's Dental Health Project "A Roadmap for Implementation- Part 1: Oral Health Provisions in Health Reform" : A policy brief focusing on the importance of oral health promotion provisions in the Patient Protection and Affordable Care Act and recommendations for how to implement the provisions.
- Dental Care for Medicaid and CHIP Enrollees : The Dental Care page on Medicaid.gov includes information on coverage of dental benefits for children and adults enrolled in Medicaid and CHIP and many tools to help states improve access to and delivery of dental and oral health care services.
Health System Stakeholders
Additional resources for stakeholders affiliated with a health system, including health providers, health insurers, or other health system stakeholders:
- American Dental Association: Topical fluoride for caries prevention: Executive summary of the updated clinical recommendations and supporting systematic review : The most recent recommendations regarding professionally applied topical fluoride from the Council on Scientific Affairs of the American Dental Association.
- Health Investments that Pay Off: Strategies to Improve Oral Health : A policy brief prepared by the National Governors Association to inform state decision makers about evidence-based interventions that can improve population health outcomes and health care quality and reduce the cost of health care as part of an overall agenda for state health care transformation.
- American Dental Association: Executive summary of evidence-based clinical recommendations for the use of pit-and-fissure sealants : The most recent recommendations regarding pit-and-fissure sealants from the Council on Scientific Affairs of the American Dental Association.
- U.S. Preventive Services Task Force Recommendation on Fluoride Varnish : The U.S. Preventive Services Task Force evidence-based recommendations for preventing dental carries in children under five years of age.
- Academy of Pediatrics: Fluoride Use in Caries Prevention in the Primary Care Setting : A clinical report clarifying the use of available fluoride modalities for caries prevention in a primary care setting, including suggestions for pediatricians on assessing risk, and providing fluoride varnish for caries prevention.
- American Dental Association Dental Quality Alliance: "Dental Caries in Children Measures Set" : Detailed specifications for the Dental Quality Alliance oral health care performance measures.
- Bright Futures in Practice: Oral Health - Pocket Guide : A tool for dentists, dental hygienists, physicians, physician assistants, nurse practitioners, nurses, dieticians, and others for preventive oral health care for pregnant and postpartum women, infants, children, and adolescents.
State Examples
Wisconsin
The Wisconsin Seal-A-Smile program decreased Medicaid dental treatment and parent travel costs by $380,091 over 9 years after a one-time placement of dental sealants and prevented 6,741 fillings over 4 years and 10,718 over 9 years. The mission of the Seal-A-Smile Program is to prevent tooth decay and promote oral health as part of a child's total health by increasing the number of dental sealants on their teeth provided by school-based sealant programs.17 The number of children who received sealants from the program increased nearly eight times, from 2,670 in 2003 to 20,073 in 2012.18
North Carolina
North Carolina’s Into the Mouths of Babes/Connecting the Docs program has reduced dental treatment needs for children younger than 18 months by 49 percent.19 Into the Mouths of Babes/Connecting the Docs is a dental health program model aimed at preventing and reducing early childhood tooth decay. The program trains medical providers to deliver a variety of preventive oral health services to children insured by North Carolina’s Medicaid program. Medical providers deliver an oral preventive procedure which includes an oral evaluation and risk assessment, counseling with primary caregivers, and the application of fluoride varnish. The services are provided to children from the time their first tooth erupts through age 3½ years. Medical providers are reimbursed by North Carolina Medicaid at a bundled rate of approximately $50 for oral health services, which has led to increased adoption of these procedures in Medicaid programs in North Carolina.
Strategies for Improved Population Health
Expand Dental Sealant Programs
Expanding low-income children’s access to dental sealants through school-based sealant programs improves the health of children and provides savings to state Medicaid programs. One economic analysis suggests that allowing dental hygienists to place sealants without a prior examination by a dentist can increase sealant receipt and lower program costs by 18 to 29 percent depending on program size.15
Integrate Dental Care into Primary Care Settings
Care delivery models that integrate preventive dental interventions (e.g., fluoride varnish) into primary care, such as well child visits, can reduce tooth decay among very young children. Providing adequate reimbursement for these services increases the likelihood that children receive fluoride varnish.20
Expand and Maintain Community Water Fluoridation Systems
In 2012, 74.6 percent of the U.S. population on public water systems had access to fluoridated water.21 The useful life of equipment needed to fluoridate water at the public water system is about 15 years.22 Based on this estimate, up to 10 percent of systems may need to replace equipment annually. Maintaining or increasing water fluoridation coverage will ensure continued broad access to this cost-effective intervention.
Improve Data Analytics Capabilities
States may consider strategies that improve their ability to collect and analyze Medicaid and Children’s Health Insurance Program data to evaluate program performance and inform policy decisions. To ensure that the data can be used to generate useful, comparable information, states could consider using age and risk categories consistent with recommended measures for performance-based care such as those put forth by the Dental Quality Alliance and endorsed by the National Quality Forum.
Maximize Current Workforce Efforts
To increase access to effective interventions that show cost-savings, states may consider maximizing dental workforce efforts by implementing recommendations from the Institute of Medicine. These include expanding scope of practice laws and changing Medicaid reimbursement policies to allow oral health professionals to practice to the top of their training.23 A recent issue brief by the National Governors Association discusses in depth the expanding dental health workforce.24
Unless year is specified, all values are reported in 2014 $US.
1
NCHS Data Brief
2 Griffin SO, Gooch B, Beltrán ED. Dental services, costs and factors associated with hospitalization for Medicaid eligible children, Louisiana 1996–1997. J Publ Health Dent 2000; 60(1):21–27.
3 Water fluoridation and costs of Medicaid treatment for dental decay—Louisiana, 1995–1996. MMWR Morb Mortal Wkly Rep 1999; 48(34): 753‐7.
4 Agency for Healthcare Research and Quality. Dental Services-Mean and Median Expenses per Person with Expense and Distribution of Expenses by Source of Payment: United States, 2012. Medical Expenditure Panel Survey Household Component Data. Generated interactively. (February 6, 2015)
5 PEW Charitable Trusts,
A Costly Dental Destination
, (February 2012), p.1.
6 Marinho VCC, Worthington HV, Walsh T, Clarkson JE. Fluoride varnishes for preventing dental caries in children and adolescents. Cochrane Database of Systematic Review 2013, no. 7: CD002279 (May 13, 2013): 1-92.
7 Recommendation Summary. U.S. Preventive Services Task Force. May 2014.
Dental Caries in Children from Birth Through Age 5 Years: Screening
8 Weyant RJ, Tracy SL, Anselmo T, et al. Topical fluoride for caries prevention: Executive summary of the updated clinical recommendations and supporting systematic review. J Am Dent Assoc 2013; 144(11): 1279-1291.
9 Community Preventive Services Task Force, “Preventing Dental Caries: School-Based Dental Sealant Delivery Programs, Task Force Finding and Rationale Statement,” Available at:
Preventing Dental Caries: School-Based Dental Sealant Delivery Programs, Task Force Finding and Rationale Statement
(accessed October 18, 2014).
10 Weintraub JA, Stearns SC, Rozier RG, Huang CC. Treatment outcomes and costs of dental sealants among children enrolled in Medicaid. Am J Public Health 2001; 91(11): 1877‐81.
11 Community Preventive Services Task Force, “Preventing Dental Caries: Community Water Fluoridation,” Available at
Preventing Dental Caries: Community Water Fluoridation
, (accessed October 18, 2014).
12 Kumar JV, Olubunmi A, Melnik TA. Geographic Variation in Medicaid Claims for Dental Procedures in New York State: Role of Fluoridation Under Contemporary Conditions. Public Health Reports 2010; 125: 647‐654.
13 Texas Department of Health. Water fluoridation costs in Texas: Texas Health Steps (EPSDT‐MEDICAID). May 2000.
14 Calculations from the Centers for Disease Control and Prevention, based on a re-analysis: Griffin S, Jones K, Tomar S. An Economic Evaluation of Community Water Fluoridation. Journal of Public Health Dentistry 2001; 61(2): 78-86.
15 Scherrer CR, Griffin PM, Swann JL. Public Health Sealant Delivery Programs: Optimal Delivery and the Cost of Practice Acts. Med Decis Making 2007; 27: 762-771.
16 Griffin SO, Jones K, Crespin M. Calculating averted caries attributable to school-based sealant programs with a minimal dataset. J Pub Health Dent 2014; 74(3): 202-9.
17
Wisconsin Oral Health Program - Seal-A-Smile Program
18
Wisconsin Seal-A-Smile 2000-2012
19 North Carolina Department of Health and Human Services, “
Into the Mouths of Babes/Connecting the Docs
,” "Into the Mouths of Babes/Connecting the Docs". (accessed October 15 2014).
20 Okunseri C, et al. Increased Children’s Access to Fluoride Varnish Treatment by Involving Medical Providers: Effect of a Medicaid Policy Change. Health Services Research 2009; 44(4): 1144-1156.
21 CDC. Community water fluoridation:
2012 water fluoridation statistics
[cited 2015 May 1]. Available at: 2012 Water Fluoridation Statistics
22 Garcia AI. Caries incidence and costs of prevention programs. J Public Health Dent 1989; 49(5 Spec No): 259-71.
23 Institute of Medicine; National Research Council. Improving access to oral health care for vulnerable and underserved populations. Washington, DC: The National Academies Press; 2011.
24 National Governors Association. The Role of Dental Hygienists in Providing Access to Oral Health Care.
- Page last reviewed: May 29, 2015
- Page last updated: May 29, 2015
- Content source:


 ShareCompartir
ShareCompartir