Controlling Asthma

The Problem
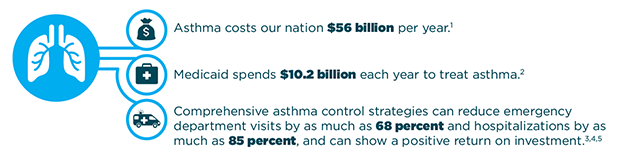
Asthma ranks as the third-highest cause of hospitalizations among children under the age of 15 and is one of the most common chronic medical conditions among children. Asthma costs the country nearly $56 billion a year in medication, office visit costs, hospitalizations, emergency department visits, mortality, and work and school absenteeism. Asthma cannot be prevented or cured, but with appropriate treatment and services, people with asthma can lead symptom-free, fully active lives.
What Can Be Done?
There are three interventions that, when delivered as a package and in a stepwise sequence, can reduce the costs of hospitalizations and emergency department visits and improve health outcomes.
- Improve clinical asthma management by helping health care providers and physician practices adhere to recommended clinical guidelines in diagnosing, assessing, treating, and monitoring patients with asthma;
- Improve personal asthma management by providing self-management education for people with asthma in a variety of settings, including medical facilities, homes, schools, and the community; and
- Improve home environments through home visits that provide education and identify and address indoor asthma “triggers” that make asthma worse.
Resources for Action
Public Health Practitioners
Find additional resources for state health officials, local health department officials, or other public health practitioners.
-
CDC’s National Asthma Control Program
: CDC’s National Asthma Control Program website includes:
- National- and state-level data and statistics on asthma
- Resources for people with asthma, health care professionals, and schools
- CDC’s Learning and Growing Through Evaluation modules for evaluating asthma-related activities and interventions
- Links to other agencies working on asthma
- Health Investments That Pay Off: Strategies for Addressing Asthma in Children : A policy brief prepared by the National Governors Association to inform state decision makers about evidence-based interventions that can improve population health outcomes and health care quality and reduce the cost of health care as part of an overall agenda for state health care transformation.
- The Community Preventive Services Task Force Asthma Control Recommendations and Findings : The Community Preventive Services Task Force recommendations and findings for home-based multi-trigger, multicomponent environmental interventions based on a scientific systematic review of available studies.
- Public health interventions for asthma: an umbrella review, 1990-2010 : An assessment and summary of existing systematic reviews of asthma-related non-clinical interventions that might be carried out or supported by state or community asthma control programs, including several reviews of the effectiveness of self-management education.
- The Agency for Healthcare Research and Quality’s Asthma ROI Calculator : An asthma return on investment (ROI) calculator that uses scientific research and de-identified patient claims data to estimate the net impact of an asthma program on state or local spending and health outcomes. It allows the user to estimate the differences in ROI achieved by focusing on people with poor control of their asthma and/or more severe asthma.
-
CDC’s Chronic Disease Cost Calculator
: CDC’s Chronic Disease Cost Calculator provides the following estimates for six chronic condition, including asthma, for the population of each of 50 states and D.C.:
- Medical expenditures for all payers and the uninsured, and separately for Medicaid, Medicare, and privately insured
- Absenteeism costs and estimates of missing work days
- Projections of medical costs until 2020
- Asthma prevalence among treated patients
- Asthma and Allergy Foundation of America: Validated Asthma Education Programs : Health education program materials that have demonstrated effectiveness.
- The Asthma Educator Institute : A two-day preparatory course for those qualified to take the National Asthma Educator Certification Board (NAECB) examination. The curriculum covers the content outlined in the NAECB Candidate Handbook and includes case reviews, hands-on skills demonstration, and practice.
- American Lung Association: Open Airways For Schools : The most widely recognized asthma management program for children in the nation.
- Seattle King County Asthma Program Resources: CDC translational grant tools and documents : A large number of tools and protocols developed by the Seattle and King County Asthma Program related to home visits and home-based trigger reduction, including training materials for community health workers.
- Community Asthma Prevention Program (CAPP), Children’s Hospital of Philadelphia : Tools for health care professionals, including home visiting assessment forms and aFour Visit Education Plan for the Asthma Prevention Office Visit.
- Using Medicaid to Advance Community-Based Childhood Asthma Interventions: A Review of Innovative Medicaid Programs in Massachusetts and Opportunities for Expansion under Medicaid Nationwide : A white paper summarizing delivery system innovations and new reimbursement models that promote community-based interventions to reduce asthma triggers in homes and community settings.
State Decision Makers
Find additional resources for governors, health policy advisors, legislators, budget officers, or other decision makers.
-
CDC’s National Asthma Control Program
: CDC’s National Asthma Control Program website includes:
- National- and state-level data and statistics on asthma
- Resources for people with asthma, health care professionals, and schools
- CDC’s Learning and Growing Through Evaluation modules for evaluating asthma-related activities and interventions
- Links to other agencies working on asthma
- Health Investments That Pay Off: Strategies for Addressing Asthma in Children : A policy brief prepared by the National Governors Association to inform state decision makers about evidence-based interventions that can improve population health outcomes and health care quality and reduce the cost of health care as part of an overall agenda for state health care transformation.
- The Community Preventive Services Task Force Asthma Control Recommendations and Findings : The Community Preventive Services Task Force recommendations and findings for home-based multi-trigger, multicomponent environmental interventions based on a scientific systematic review of available studies.
- Public health interventions for asthma: an umbrella review, 1990-2010 An assessment and summary of existing systematic reviews of asthma-related non-clinical interventions that might be carried out or supported by state or community asthma control programs, including several reviews of the effectiveness of self-management education.
- The Agency for Healthcare Research and Quality’s Asthma ROI Calculator : An asthma return on investment (ROI) calculator that uses scientific research and de-identified patient claims data to estimate the net impact of an asthma program on state or local spending and health outcomes. It allows the user to estimate the differences in ROI achieved by focusing on people with poor control of their asthma and/or more severe asthma.
- Using Medicaid to Advance Community-Based Childhood Asthma Interventions: A Review of Innovative Medicaid Programs in Massachusetts and Opportunities for Expansion under Medicaid Nationwide : A white paper summarizing delivery system innovations and new reimbursement models that promote community-based interventions to reduce asthma triggers in homes and community settings.
State Medicaid Officials
Find additional resources for state Medicaid programs.
-
CDC’s National Asthma Control Program
: CDC’s National Asthma Control Program website includes:
- National- and state-level data and statistics on asthma
- Resources for people with asthma, health care professionals, and schools
- CDC’s Learning and Growing Through Evaluation modules for evaluating asthma-related activities and interventions
- Links to other agencies working on asthma
- Health Investments That Pay Off: Strategies for Addressing Asthma in Children : A policy brief prepared by the National Governors Association to inform state decision makers about evidence-based interventions that can improve population health outcomes and health care quality and reduce the cost of health care as part of an overall agenda for state health care transformation.
- Using Medicaid to Advance Community-Based Childhood Asthma Interventions: A Review of Innovative Medicaid Programs in Massachusetts and Opportunities for Expansion under Medicaid Nationwide : A white paper summarizing delivery system innovations and new reimbursement models that promote community-based interventions to reduce asthma triggers in homes and community settings.
- The Agency for Healthcare Research and Quality’s Asthma ROI Calculator : An asthma return on investment (ROI) calculator that uses scientific research and de-identified patient claims data to estimate the net impact of an asthma program on state or local spending and health outcomes. It allows the user to estimate the differences in ROI achieved by focusing on people with poor control of their asthma and/or more severe asthma.
-
CDC’s Chronic Disease Cost Calculator
: CDC’s Chronic Disease Cost Calculator provides the following estimates for six chronic condition, including asthma, for the population of each of 50 states and D.C.:
- Medical expenditures for all payers and the uninsured, and separately for Medicaid, Medicare, and privately insured
- Absenteeism costs and estimates of missing work days
- Projections of medical costs until 2020
- Asthma prevalence among treated patients
Health System Stakeholders
Find resources for stakeholders affiliated with a health system, including health providers, health insurers, or other health system stakeholders.
-
CDC’s National Asthma Control Program
: CDC’s National Asthma Control Program website includes:
- National- and state-level data and statistics on asthma
- Resources for people with asthma, health care professionals, and schools
- CDC’s Learning and Growing Through Evaluation modules for evaluating asthma-related activities and interventions
- Links to other agencies working on asthma
- Health Investments That Pay Off: Strategies for Addressing Asthma in Children : A policy brief prepared by the National Governors Association to inform state decision makers about evidence-based interventions that can improve population health outcomes and health care quality and reduce the cost of health care as part of an overall agenda for state health care transformation.
- National Asthma Education and Prevention Program Guidelines for the Diagnosis and Management of Asthma, Expert Panel Report-3 (EPR-3) : Clinical guidelines developed by an expert panel commissioned by the National Asthma Education and Prevention Program Coordinating Committee, which is coordinated by the National Heart, Lung, and Blood Institute of the National Institutes of Health.
- Asthma Care Quick Reference Guide : A user-friendly, 12-page decision support tool that summarizes the EPR-3 clinical guidelines.
-
CDC Community Health Improvement Navigator
: A website for people who lead or participate in community health improvement work within hospitals and health systems, public health agencies, and other community organizations. It is a one-stop-shop that offers community stakeholders expert-vetted tools and resources for:
- Depicting visually the who, what, where, and how of improving community health
- Making the case for collaborative approaches to community health improvement
- Establishing and maintaining effective collaborations
- Finding interventions that work for the greatest impact on health and well-being for all
- The American Academy of Pediatrics Pedialink Asthma Curriculum : A curriculum to help health care professionals determine the severity and level of control of asthma in their patients, identify environmental triggers, understand their patient's special situations that will impact care, and learn the proper usage of asthma medication delivery devices.
- The American Academy of Pediatrics Education in Quality Improvement for Pediatric Practice (EQIPP) : EQIPP provides information, tools, and guidance to make systematic and continuous practice improvements in asthma care. It enables a practice to collect, analyze, and measure data over time and make small, rapid cycles of change.
- Seattle King County Asthma Program Resources: CDC translational grant tools and documents : A large number of tools and protocols developed by the Seattle and King County Asthma Program related to home visits and home-based trigger reduction, including training materials for community health workers.
- Community Asthma Prevention Program (CAPP), Children’s Hospital of Philadelphia : Tools for health care professionals, including home visiting assessment forms and a Four Visit Education Plan for the Asthma Prevention Office Visit.
- The Asthma Educator Institute : A two-day preparatory course for those qualified to take the National Asthma Educator Certification Board (NAECB) examination. The curriculum covers the content outlined in the NAECB Candidate Handbook and includes case reviews, hands-on skills demonstration and practice.
- Asthma and Allergy Foundation of America: Validated Asthma Education Programs : Health education program materials that have demonstrated effectiveness.
State Examples
Michigan
In 1999, the Asthma Network of West Michigan entered into the first-ever agreement between a community asthma coalition and a health plan for the reimbursement of asthma self-management education home visits at the standard Medicaid rate for a skilled nursing visit. As a result of the success of this partnership, the Michigan Department of Health and Human Services convened a payer summit in 2008 where insurers agreed to reimburse asthma self-management education home visits, expanding access to asthma home visits in the state. Home visits were conducted by registered nurses or respiratory therapists who are certified asthma educators and who provided home-based education, home environmental assessments, and resources to reduce exposures to environmental asthma triggers. Utilization data showed reductions in emergency department visits for patients with private insurance from 72 visits per 1,000 patients in 2002 to 40 in 2006, and from 250 to 189 for Medicaid members. Savings over time for members is estimated at $1.7 million, and the long-term return on investment5 (ROI) for insurers is $2.10 for every $1 of program costs.
Missouri
The CDC-funded Missouri Asthma Prevention and Control Program (MAPCP) joined with longtime partner University of Missouri Asthma Ready Communities to create “Teaming Up for Asthma Control” (TUAC), an initiative to train and equip school nurses to support students with persistent asthma. In many communities across the state, 54 TUAC-trained nurses focused on: (1) assessing asthma severity per National Asthma Education and Prevention Program (NAEPP) guidelines,6 (2) evaluating student self-care behaviors, and (3) educating students with persistent asthma and their families. The first phase of the rigorous evaluation plan, which included 164 school-age children, demonstrated improvements in symptoms, medication inhalation technique, lung function, and tobacco smoke exposure in the home. The analysis of Medicaid claims data showed the TUAC program resulted in lower emergency room use and annualized cost savings of approximately $1,200 per participant. When self-management education is linked to medical care consistent with EPR-3 guidelines even greater cost savings are achieved. A prior study revealed children with persistent asthma who were provided NAEPP guidelines–compliant care by a specialty clinic cost Medicaid about $5,400 (or 30 percent) less per year. The clinic’s use of self-management education was a critical factor that improved medication adherence and trigger avoidance and reduced total cost of care.
Strategies for Improved Population Health
This focused set of interventions represents a starting point for public health-health care collaboration and, when implemented as a comprehensive package, has been shown to yield a positive return on investment.
Assure Guidelines-Based Medical Management
Implementing guidelines-based medical management and facilitating adherence to recommended therapy decreases asthma symptoms, school and work absences, and asthma-related health care utilization. It also improves asthma-related quality of life. Incorporating recommended assessment, education, and treatment practices into electronic health records, reporting requirements, and quality improvement processes can promote uptake of guidelines-based care. Eliminating formulary restrictions and co-pays for medications and devices has been shown to lead to an uptake of these services and decreases in adverse health outcomes.7
Provide Self-Management Education
People with moderate-to-severe persistent asthma, especially people whose asthma is not well controlled with medical management alone, require more intense education and skills training to reinforce and expand upon the limited number of messages that can be delivered in the context of a health care visit. Providing asthma self-management education as an adjunct to guidelines-based medical management can improve asthma control and decrease hospitalizations and emergency department visits. Public health agencies play an important role in assuring the availability of evidence-based self-management education programs and appropriately-trained staff to deliver the programs.
Facilitate Home Visits
People whose asthma is not well controlled with medical management and self-management education may experience environmental conditions (triggers) or social problems in the home that make it difficult to control their asthma. Encouraging collaboration across programs and sectors that provide home visits by removing barriers to sharing resources, referrals, training, and even personnel across programs that serve similar populations increases the accessibility of these services. The recent Medicaid rule 42 CFR § 440.130(c) allowing non-licensed providers, like community health workers, to be reimbursed for providing covered preventive services in non-clinical settings gives agencies new options for financing and delivering those services. Electronic referral and communication tools enable health care providers to refer appropriate patients to home visit services and follow up on the information provided by the home visitors. Public health practitioners support these efforts by establishing curricula and credentialing guidelines for home visitors and sharing best practices and evidence about their cost effectiveness.
Establish Linkages across Health Sectors
Achieving both improved population health and a positive return on investment is dependent on the efficient provision of necessary services without duplication or waste. Investments in information-sharing mechanisms that resolve privacy and interoperability issues can streamline communication across sectors and allow direct referral from the clinic-based electronic health record to appropriate community- and home-based services. Efficient coordination and information sharing through these types of mechanisms can result in improved health outcomes and decreased costs.
Build Long-Term Support through Evaluation
A comprehensive evaluation strategy is critical for monitoring program implementation, improving efficiency and effectiveness, and can provide credible data on the costs, outcomes, and ROI achieved in the state or local context.
1 Costs of Asthma in the Unites States: 2002–2007, Journal of Allergy and Clinical Immunology 127, no. 1 (January 2011): 145–152, retrieved from
Costs of asthma in the United States: 2002-2007
April 20, 2015.
2 Calculations from the Centers for Disease Control and Prevention (CDC) based on 2003–2008 Medical Expenditure Panel Surveys and the CDC Chronic Disease Cost Calculator.
Chronic Disease Cost Calculator Version 2r
(accessed April 20, 2015).
3 Elizabeth R. Woods et al. Community Asthma Initiative: Evaluation of a Quality Improvement Program for Comprehensive Asthma Care, Pediatrics 129, no. 3 (March 2012): 465–472,
Community Asthma Initiative: Evaluation of a Quality Improvement Program for Comprehensive Asthma Care
.
4 Sibylle H Lob et al, “
Promoting Best-Care Practices in Childhood Asthma: Quality Improvement in Community Health Centers
, Pediatrics 128, no. 20 (2011): 20-28, retrieved from Promoting Best-Care Practices in Childhood Asthma: Quality Improvement in Community Health Centers (accessed April 22, 2015).
5 T. Nurmagambetov et al. Economic Value of Home-based, Multi-Trigger, Multicomponent Interventions with an Environmental Focus for Reducing Asthma Morbidity: A Community Guide Systematic Review, American Journal of Preventative Medicine 41, 2S1 (2011): S33–S47,
Economic Value of Home-Based, Multi-Trigger, Multicomponent Interventions with an Environmental Focus for Reducing Asthma Morbidity
.
5 Return on Investment (ROI) represents the ratio of all monetized benefits of the program over one dollar of program cost.
6 The expert panel organized the literature review and final guidelines report around four essential components of asthma care, namely: assessment and monitoring, patient education, control of factors contributing to asthma severity, and pharmacologic treatment. Subtopics were developed for each of these four broad categories. See more at
National Heart, Lung, and Blood Institute
.
7 Campbell JD, Allen-Ramey F, Sajjan SG, Maiese EM, Sullivan SD. Increasing pharmaceutical copayments: impact on asthma medication utilization and outcomes. The American Journal of Managed Care [2011, 17(10): 703-710].
- Page last reviewed: May 29, 2015
- Page last updated: May 29, 2015
- Content source:


 ShareCompartir
ShareCompartir