Key Findings: Persons with Disabilities as an Unrecognized Health Disparity Population

Reducing Health Disparities for People with Disabilities: A Public Health Challenge
The American Journal of Public Health published a commentary in its Framing Health Matters section focused on the importance of addressing health disparities among people with disabilities in relation to access to health care, health behaviors (such as smoking and physical inactivity), health status (the presence or absence of a long-standing disease like diabetes), and social factors that impact health (such as poverty). This work was the joint effort of disability researchers at the Department of Health and Human Services (including the Centers for Disease Control and Prevention and The National Institutes of Health) and Abt Associates.
You can read the full article here.
Main findings
The paper summarizes evidence demonstrating that people with disabilities across the lifespan experience health disparities, and provides recommendations in key areas for improving their health.
The paper also presents the discussion about disability and health in a historical context, illustrating past and current efforts, and what can be done in the future. Broad areas in which efforts can be promoted to improve the health of people with disabilities include improved access to health care and human services, increased use of data for decision-making, strengthening health and human services workforce capacity, renewed efforts to include people with disabilities in public health programs, and increased preparation for emergencies.
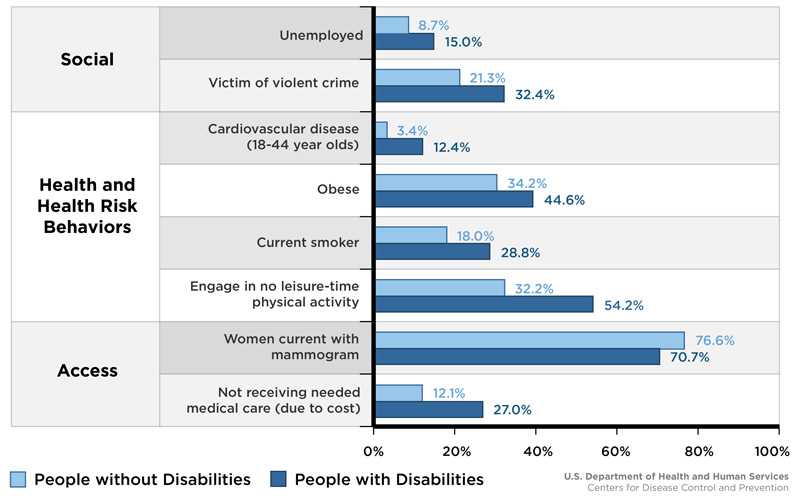
Data used to illustrate health disparities related to disability were presented from multiple data sources. Some examples of disparities between people with and without disabilities included measures of health care access, preventive care, physical activity, heart disease (cardiovascular disease), being a victim of a violent crime, and employment (see figure). Specifically, compared to adults without a disability, the data showed that adults with a disability were more likely to be affected by:
- Certain social factors; adults with a disability were more likely to be
- Unemployed
- A victim of a violent crime
- Health and health risk behaviors; adults with a disability were more likely to
- Have cardiovascular (heart) disease
- Be obese
- Be a current smoker
- Engage in no leisure-time physical activity
- Lack of health care access; adults with a disability were less likely to
- Have a current mammogram
- Be receiving needed medical care (because of the cost of care)
Factors Affecting the Health of People with Disabilities and without Disabilities
All estimates are for adults 18 and over, except for "victim of violent crime" which is for respondents 12 and over.
(1) Armour BS, Thierry JM, Wolfe LA. State-level differences in breast and cervical cancer screening by disability status: United States, 2008. Womens Health Issues. 2009;19:406-414.
(2) Rand MR, Harrell E. National crime victimization survey: crime against people with disabilities, 2007. Bur Justice Stat Spec Rep. 2009: NCJ 227814.

Implications/Recommendations:
The paper offers key recommendations to address the differences described above:
- Improve access to health care and human services. For example, use of accessible equipment in medical practice (such as wheelchair accessible scales) and compliance with the Americans with Disabilities Act (ADA) and the Affordable Care Act (ACA), which provide accessibility guidelines, could improve access.
- Improve data collection, and use it to advance public health standards. For example, routine use of disability status in analyses, to provide information about relationship of disability status with health and health behaviors (such as smoking, physical activity, use of preventive care), could help provide health systems, as well as medical and public health professionals, with the needed information on where to focus to improve the health of people with disabilities across the lifespan.
- Strengthen the workforce. For example, increased training of healthcare providers could support
- Earlier identification and intervention for children with disabilities;
- Improved services for youth with disabilities transitioning into the adult care system; and
- Improved health care and health promotion for all people with disabilities.
- Include people with disabilities in public health programs and practices. For example, organizations and systems would benefit from instituting specific policies and practices for including people with disabilities into mainstream programs and research.
- Often, the changes programs make to include people with disabilities will improve the ability for ALL people to participate.
- Plan for inclusion—facilities should be wheel-chair accessible, and information should be accessible by people who have trouble with vision, hearing, or understanding complex information.
- Prepare for emergencies with people with disabilities in mind. For example, considering people with all types of disabilities in all preparedness planning activities could help meet their differing needs during emergencies (such needs might include assistive equipment and animals; medications; and accessible shelter facilities).
CDC’s Work on Disability and Health Disparities
CDC monitors the health of people with and without disabilities, and supports the inclusion of people with disabilities in public health programs that prevent disease and promote healthy behaviors. CDC also works to eliminate barriers to health care and improve access to routine preventive services.
CDC supports 18 state-based disability and health programs and four National Public Health Practice and Resource Centers, which promote healthy lifestyles and work to improve quality of life for people with disabilities. The primary goals of the state programs are to:
- Increase health promotion opportunities for people with disabilities.
- Improve access to health care services for people with disabilities.
- Improve emergency preparedness for people with disabilities.
CDC also maintains the Disability and Health Data System (DHDS), an online interactive tool that provides instant access to state-level, disability-specific health data. Users can customize the disability and health data they view, making it easy to identify health differences between adults with and without disabilities.
Key Findings Reference
Krahn GL, Walker DK, Correa-De-Araujo R. Persons with disabilities as an unrecognized health disparity population. American Journal of Public Health. 2015 Feb 17:e1-e9.
More Information
To learn more about disability disparities and CDC’s work in this area, please visit: https://www.cdc.gov/ncbddd/disabilityandhealth/
Additional Resources
- Page last reviewed: March 31, 2015
- Page last updated: March 31, 2015
- Content source:


 ShareCompartir
ShareCompartir