Antibiotic Resistance Questions and Answers
Español: Preguntas y respuestas sobre la resistencia a los antibióticos
Questions about Bacteria, Viruses, and Antibiotics
Q: What are bacteria and viruses?
A: Bacteria are single-celled organisms found all over the inside and outside of our bodies. Many bacteria are not harmful. In fact, some are actually helpful, including the majority of bacteria that live in our intestines (guts). However, disease-causing bacteria can cause illnesses such as strep throat. Viruses, on the other hand, are microbes that are even smaller than bacteria that cannot survive outside the body's cells. They cause illness by invading healthy cells.
The Antibiotic resistance threats in the United States, 2013 report gives a first-ever snapshot of the burden and threats posed by the antibiotic-resistant germs having the most impact on human health. Read the report.
Q: What is an antibiotic?
A: Antibiotics, also known as antimicrobial drugs, are drugs that fight infections caused by bacteria in both humans and animals. Antibiotics fight these infections either by killing the bacteria or making it difficult for the bacteria to grow and multiply. Antibiotics do not have any effect on viruses.
The term "antibiotic" originally referred to a natural compound that kills bacteria, such as certain types of mold or chemicals produced by living organisms. Technically, the term "antimicrobial" refers to both natural and synthetic (man-made) compounds; however, many people use the word "antibiotic" to refer to both.
Q: Which infections are caused by viruses and should not be treated with antibiotics?
A: Viral infections should not be treated with antibiotics. Common infections caused by viruses include:
- Colds
- Flu
- Most sore throats
- Most coughs and bronchitis (“chest colds”)
- Many sinus infections
- Many ear infections
Questions about Antibiotic Resistance
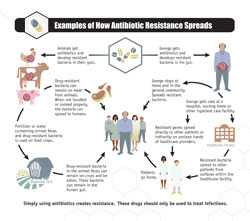
Examples of How Antibiotic Resistance Spreads
Q: What is antibiotic resistance?
A: Antibiotic resistance is the ability of bacteria to resist the effects of an antibiotic. Antibiotic resistance occurs when bacteria change in a way that reduces the effectiveness of drugs, chemicals, or other agents designed to cure or prevent infections. The bacteria survive and continue to multiply, causing more harm.
Q: Why should I care about antibiotic resistance?
A: Antibiotic resistance has been called one of the world's most pressing public health problems. Antibiotic resistance can cause illnesses that were once easily treatable with antibiotics to become dangerous infections, prolonging suffering for children and adults. Antibiotic-resistant bacteria can spread to family members, schoolmates, and co-workers, and may threaten your community. Antibiotic-resistant bacteria are often more difficult to kill and more expensive to treat. In some cases, the antibiotic-resistant infections can lead to serious disability or even death.
Although some people think a person becomes resistant to specific drugs, it is the bacteria, not the person, that become resistant to the drugs.
Q: Why are bacteria becoming resistant to antibiotics?
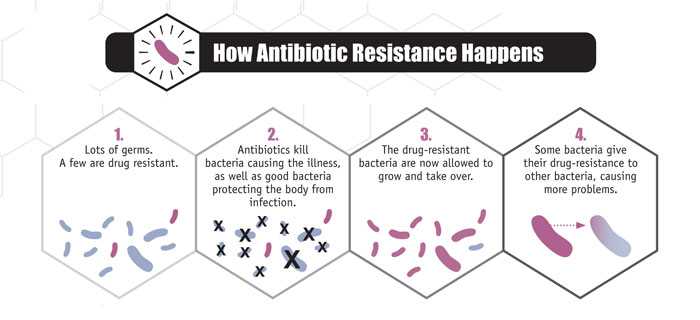
A: Overuse and misuse of antibiotics can promote the development of antibiotic-resistant bacteria. Every time a person takes antibiotics, sensitive bacteria (bacteria that antibiotics can still attack) are killed, but resistant bacteria are left to grow and multiply. This is how repeated use of antibiotics can increase the number of drug-resistant bacteria.
Antibiotics are not effective against viral infections like the common cold, flu, most sore throats, bronchitis, and many sinus and ear infections. Widespread use of antibiotics for these illnesses is an example of how overuse of antibiotics can promote the spread of antibiotic resistance. Smart use of antibiotics is key to controlling the spread of resistance.
Q: How do bacteria become resistant to antibiotics?
A: Bacteria can become resistant to antibiotics through several ways. Some bacteria can “neutralize” an antibiotic by changing it in a way that makes it harmless. Others have learned how to pump an antibiotic back outside of the bacteria before it can do any harm. Some bacteria can change their outer structure so the antibiotic has no way to attach to the bacteria it is designed to kill.
After being exposed to antibiotics, sometimes one of the bacteria can survive because it found a way to resist the antibiotic. If even one bacterium becomes resistant to antibiotics, it can then multiply and replace all the bacteria that were killed off. That means that exposure to antibiotics provides selective pressure making the surviving bacteria more likely to be resistant. Bacteria can also become resistant through mutation of their genetic material.
The Food and Drug Administration's (FDA's) Center for Veterinary Medicine (CVM) produced a nine-minute animation explaining how antimicrobial resistance both emerges and increases among bacteria.
Q: How should I use antibiotics to protect myself and my community from antibiotic resistance?
A: Here is what you can do to help prevent antibiotic resistance:
- Tell your healthcare professional you are concerned about antibiotic resistance.
- Ask your healthcare professional if there are steps you can take to feel better and get symptomatic relief without using antibiotics.
- Take the prescribed antibiotic exactly as your healthcare professional tells you.
- Discard any leftover medication.
- Ask your healthcare professional about vaccines recommended for you and your family to prevent infections that may require an antibiotic.
- Never skip doses or stop taking an antibiotic early unless your healthcare professional tells you to do so.
- Never take an antibiotic for a viral infection like a cold or the flu.
- Never pressure your healthcare professional to prescribe an antibiotic.
- Never save antibiotics for the next time you get sick.
- Never take antibiotics prescribed for someone else.
Q: How can healthcare professionals help prevent the spread of antibiotic resistance?
A: Healthcare professional can prevent the spread of antibiotic resistance by:
- Prescribing an antibiotic only when it is likely to benefit the patient.
- Prescribing an antibiotic that targets the bacteria that is most likely causing their patient’s illness when an antibiotic is likely to provide benefit.
- Encouraging patients to use the antibiotic as instructed.
- Collaborating with each other, office staff, and patients to promote appropriate antibiotic use.
- Continue reviewing and following the latest clinical practice guidelines for common infections, such as CDC's Adult and Pediatric Academic Detailing Sheets.
For more information on what healthcare professionals can do to help prevent antibiotic resistance, please see our Fact Sheet for Healthcare Providers [2 pages].
Questions about Antimicrobial Cleaning Agents, Acne Medication, and Probiotics
Q: Is it healthier to use antimicrobial-containing products (soaps, household cleaners) than regular products?
A: To date, studies have shown that there is no added health benefit for consumers (this does not include professionals in the healthcare setting) using soaps containing antibacterial ingredients compared with using plain soap. As a result, FDA released a proposed rule in December 2013 to require manufacturers to submit data supporting the efficacy and safety of antibacterial soaps and body washes. This proposed rule does not affect hand sanitizers, wipes, or antibacterial products used in healthcare settings. For more information, please see the CDC handwashing web page.
Q: Can antibiotic resistance develop from using acne medication?
A: Yes. Antibiotic use, appropriate or not, contributes to the development of antibiotic resistance. This is true for acne medications that contain antibiotics. Short- and long-term use of antibiotics for treatment or prevention of bacterial infections should be under the direction of a healthcare professional to ensure appropriate use and detection of resistance.
Q: Do probiotics have a role in helping to reduce antibiotic resistance?
A: Probiotics are defined as microorganisms that when administered in sufficient quantities may improve health. There are a variety of probiotics that have been studied for various health benefits. Their role in preventing drug-resistant infections in humans has not been established. CDC is actively researching the subject. Although some studies have shown benefit, the data are not conclusive enough for CDC to issue specific recommendations at this time.
- Page last reviewed: April 17, 2015
- Page last updated: April 17, 2015
- Content source:


 ShareCompartir
ShareCompartir