Plague (disease)
Plague is an infectious disease caused by the bacterium Yersinia pestis.[2] Symptoms include fever, weakness and headache.[1] Usually this begins one to seven days after exposure.[2] In the bubonic form there is also swelling of lymph nodes, while in the septicemic form tissues may turn black and die, and in the pneumonic form shortness of breath, cough and chest pain may occur.[1]
| Plague | |
|---|---|
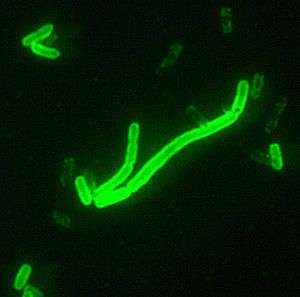 | |
| Yersinia pestis seen at 200× magnification with a fluorescent label. | |
| Specialty | Infectious disease |
| Symptoms | Fever, weakness, headache[1] |
| Usual onset | 1-7 days after exposure[2] |
| Types | Bubonic plague, septicemic plague, pneumonic plague[1] |
| Causes | Yersinia pestis[2] |
| Diagnostic method | Finding the bacterium in a lymph node, blood, sputum[2] |
| Prevention | Plague vaccine[2] |
| Treatment | Antibiotics and supportive care[2] |
| Medication | Gentamicin and a fluoroquinolone[3] |
| Prognosis | ~10% risk of death (with treatment)[4] |
| Frequency | ~600 cases a year[2] |
Bubonic and septicemic plague is generally spread by flea bites or handling an infected animal.[1] The pneumonitic form is generally spread between people through the air via infectious droplets.[1] Diagnosis is typically by finding the bacterium in fluid from a lymph node, blood or sputum.[2]
Those at high risk may be vaccinated.[2] Those exposed to a case of pneumonic plague may be treated with preventive medication.[2] If infected, treatment is with antibiotics and supportive care.[2] Typically antibiotics include a combination of gentamicin and a fluoroquinolone.[3] The risk of death with treatment is about 10% while without it is about 70%.[4]
Globally about 600 cases are reported a year.[2] In 2017 the countries with the most cases include the Democratic Republic of the Congo, Madagascar and Peru.[2] In the United States infections occasionally occur in rural areas, where the bacteria is believed to circulate among rodents.[5] It has historically occurred in large outbreaks, with the best known being the Black Death in the 14th century, which resulted in greater than 50 million deaths.[2]
Signs and symptoms
Bubonic plague

When a flea bites a human and contaminates the wound with regurgitated blood, the plague-carrying bacteria are passed into the tissue. Y. pestis can reproduce inside cells, so even if phagocytosed, they can still survive. Once in the body, the bacteria can enter the lymphatic system, which drains interstitial fluid. Plague bacteria secrete several toxins, one of which is known to cause beta-adrenergic blockade.[6]
Y. pestis spreads through the lymphatic vessels of the infected human until it reaches a lymph node, where it causes acute lymphadenitis.[7] The swollen lymph nodes form the characteristic buboes associated with the disease,[8] and autopsies of these buboes have revealed them to be mostly hemorrhagic or necrotic.[9]
If the lymph node is overwhelmed, the infection can pass into the bloodstream, causing secondary septicemic plague and if the lungs are seeded, it can cause secondary pneumonic plague.[10]
Septicemic plague

Lymphatics ultimately drain into the bloodstream, so the plague bacteria may enter the blood and travel to almost any part of the body. In septicemic plague, bacterial endotoxins cause disseminated intravascular coagulation (DIC), causing tiny clots throughout the body and possibly ischemic necrosis (tissue death due to lack of circulation/perfusion to that tissue) from the clots. DIC results in depletion of the body's clotting resources, so that it can no longer control bleeding. Consequently, there is bleeding into the skin and other organs, which can cause red and/or black patchy rash and hemoptysis/hematemesis (coughing up/ vomiting of blood). There are bumps on the skin that look somewhat like insect bites; these are usually red, and sometimes white in the center. Untreated, septicemic plague is usually fatal. Early treatment with antibiotics reduces the mortality rate to between 4 and 15 percent.[11][12][13] People who die from this form of plague often die on the same day symptoms first appear.
Pneumonic plague
The pneumonic form of plague arises from infection of the lungs. It causes coughing and sneezing and thereby produces airborne droplets that contain bacterial cells and are likely to infect anyone inhaling them. The incubation period for pneumonic plague is short, usually two to four days, but sometimes just a few hours. The initial signs are indistinguishable from several other respiratory illnesses; they include headache, weakness and spitting or vomiting of blood. The course of the disease is rapid; unless diagnosed and treated soon enough, typically within a few hours, death may follow in one to six days; in untreated cases mortality is nearly 100%.[14][15]
Cause
.jpg)

Transmission of Y. pestis to an uninfected individual is possible by any of the following means.[16]
- droplet contact – coughing or sneezing on another person
- direct physical contact – touching an infected person, including sexual contact
- indirect contact – usually by touching soil contamination or a contaminated surface
- airborne transmission – if the microorganism can remain in the air for long periods
- fecal-oral transmission – usually from contaminated food or water sources
- vector borne transmission – carried by insects or other animals.
Yersinia pestis circulates in animal reservoirs, particularly in rodents, in the natural foci of infection found on all continents except Australia. The natural foci of plague are situated in a broad belt in the tropical and sub-tropical latitudes and the warmer parts of the temperate latitudes around the globe, between the parallels 55 degrees North and 40 degrees South.[16] Contrary to popular belief, rats did not directly start the spread of the bubonic plague. It is mainly a disease in the fleas (Xenopsylla cheopis) that infested the rats, making the rats themselves the first victims of the plague. Infection in a human occurs when a person is bitten by a flea that has been infected by biting a rodent that itself has been infected by the bite of a flea carrying the disease. The bacteria multiply inside the flea, sticking together to form a plug that blocks its stomach and causes it to starve. The flea then bites a host and continues to feed, even though it cannot quell its hunger, and consequently the flea vomits blood tainted with the bacteria back into the bite wound. The bubonic plague bacterium then infects a new person and the flea eventually dies from starvation. Serious outbreaks of plague are usually started by other disease outbreaks in rodents, or a rise in the rodent population.[17]
Prevention
Since human plague is rare in most parts of the world, routine vaccination is not needed other than for those at particularly high risk of exposure, nor for people living in areas with enzootic plague, meaning it occurs at regular, predictable rates in populations and specific areas, such as the western United States. It is not even indicated for most travellers to countries with known recent reported cases, particularly if their travel is limited to urban areas with modern hotels. The CDC thus only recommends vaccination for: (1) all laboratory and field personnel who are working with Y. pestis organisms resistant to antimicrobials: (2) people engaged in aerosol experiments with Y. pestis; and (3) people engaged in field operations in areas with enzootic plague where preventing exposure is not possible (such as some disaster areas).[18]
A systematic review by the Cochrane Collaboration found no studies of sufficient quality to make any statement on the efficacy of the vaccine.[19]
Treatments
If diagnosed in time, the various forms of plague are usually highly responsive to antibiotic therapy. The antibiotics often used are streptomycin, chloramphenicol and tetracycline. Amongst the newer generation of antibiotics, gentamicin and doxycycline have proven effective in monotherapeutic treatment of plague.[20]
The plague bacterium could develop drug resistance and again become a major health threat. One case of a drug-resistant form of the bacterium was found in Madagascar in 1995.[21] Further outbreaks in Madagascar were reported in November 2014[22] and October 2017.[23]
Epidemiology
Globally about 600 cases are reported a year.[2] In 2017 the countries with the most cases include the Democratic Republic of the Congo, Madagascar and Peru.[2] It has historically occurred in large outbreaks, with the best known being the Black Death in the 14th century which resulted in greater than 50 million dead.[2]
Biological weapon
Plague has a long history as a biological weapon. Historical accounts from ancient China and medieval Europe detail the use of infected animal carcasses, such as cows or horses, and human carcasses, by the Xiongnu/Huns, Mongols, Turks and other groups, to contaminate enemy water supplies. Han Dynasty General Huo Qubing is recorded to have died of such a contamination while engaging in warfare against the Xiongnu. Plague victims were also reported to have been tossed by catapult into cities under siege.[24]
In 1347, the Genoese possession of Caffa, a great trade emporium on the Crimean peninsula, came under siege by an army of Mongol warriors of the Golden Horde under the command of Janibeg. After a protracted siege during which the Mongol army was reportedly withering from the disease, they decided to use the infected corpses as a biological weapon. The corpses were catapulted over the city walls, infecting the inhabitants. This event might have led to the transfer of the plague (Black Death) via their ships into the south of Europe, possibly explaining its rapid spread.[25]
During World War II, the Japanese Army developed weaponised plague, based on the breeding and release of large numbers of fleas. During the Japanese occupation of Manchuria, Unit 731 deliberately infected Chinese, Korean and Manchurian civilians and prisoners of war with the plague bacterium. These subjects, termed "maruta" or "logs", were then studied by dissection, others by vivisection while still conscious. Members of the unit such as Shiro Ishii were exonerated from the Tokyo tribunal by Douglas MacArthur but 12 of them were prosecuted in the Khabarovsk War Crime Trials in 1949 during which some admitted having spread bubonic plague within a 36-km radius around the city of Changde.[26]
Ishii innovated bombs containing live mice and fleas, with very small explosive loads, to deliver the weaponized microbes, overcoming the problem of the explosive killing the infected animal and insect by the use of a ceramic, rather than metal, casing for the warhead. While no records survive of the actual usage of the ceramic shells, prototypes exist and are believed to have been used in experiments during WWII.
After World War II, both the United States and the Soviet Union developed means of weaponising pneumonic plague. Experiments included various delivery methods, vacuum drying, sizing the bacterium, developing strains resistant to antibiotics, combining the bacterium with other diseases (such as diphtheria), and genetic engineering. Scientists who worked in USSR bio-weapons programs have stated that the Soviet effort was formidable and that large stocks of weaponised plague bacteria were produced. Information on many of the Soviet projects is largely unavailable. Aerosolized pneumonic plague remains the most significant threat.
The plague can be easily treated with antibiotics, which some countries, such as the United States, have large supplies on hand if such an attack should occur, thus making the threat less severe.[27]
See also
References
- "Symptoms Plague". CDC. September 2015. Retrieved 8 November 2017.
- "Plague". World Health Organization. October 2017. Retrieved 8 November 2017.
- "Resources for Clinicians Plague". CDC. October 2015. Retrieved 8 November 2017.
- "FAQ Plague". CDC. September 2015. Retrieved 8 November 2017.
- "Transmission Plague". CDC. September 2015. Retrieved 8 November 2017.
- Brown, SD; Montie, TC (1977). "Beta-adrenergic blocking activity of Yersinia pestis murine toxin". Infection and Immunity. 18 (1): 85–93. PMC 421197. PMID 198377.
- Sebbane, F; Jarret, C.O.; Gardner, D; Long, D; Hinnebusch, B.J. (2006). "Role of Yersinia pestis plasminogen activator in the incidence of distinct septicemic and bubonic forms of flea-borne plague". Proc Natl Acad Sci U S A. 103 (14): 5526–5530. doi:10.1073/pnas.0509544103. PMC 1414629. PMID 16567636.
- "Symptoms | Plague". Centers for Disease Control and Prevention. 14 September 2015. Retrieved 18 April 2017.
- Sebbane, F; Gardner, D; Long, D; Gowen, B.B.; Hinnebusch, B.J. (2005). "Kinetics of Disease Progression and Host Response in a Rat Model of Bubonic Plague". Am J Pathol. 166 (5): 1427–1439. doi:10.1016/S0002-9440(10)62360-7. PMC 1606397. PMID 15855643.
- "Plague". Centers for Disease Control and Prevention. Retrieved 2014-08-05.
- Wagle PM (1948). "Recent advances in the treatment of bubonic plague". Indian J Med Sci. 2: 489–94.
- Meyer KF (1950). "Modern therapy of plague". J Am Med Assoc. 144 (12): 982–85. doi:10.1001/jama.1950.02920120006003. PMID 14774219.
- Datt Gupta AK (1948). "A short note on plague cases treated at Campbell Hospital". Ind Med Gaz. 83: 150–51.
- Ryan, K. J.; Ray, C. G., eds. (2004). Sherris Medical Microbiology: An Introduction to Infectious Diseases (4th ed.). New York: McGraw-Hill. ISBN 978-0-8385-8529-0.
- Hoffman SL (1980). "Plague in the United States: the "Black Death" is still alive". Annals of Emergency Medicine. 9 (6): 319–22. doi:10.1016/S0196-0644(80)80068-0. PMID 7386958.
- Plague Manual: Epidemiology, Distribution, Surveillance and Control, pp. 9, 11. WHO/CDS/CSR/EDC/99.2
- Yersin, Alexandre (1894). "La peste bubonique à Hong-Kong". Annales de l'Institut Pasteur. 8: 662–67.
- "Plague Vaccine". CDC. June 11, 1982. Retrieved Apr 30, 2015.
- Jefferson T, Demicheli V, Pratt M; Demicheli; Pratt (2000). Jefferson, Tom (ed.). "Vaccines for preventing plague". Cochrane Database Syst Rev (2): CD000976. doi:10.1002/14651858.CD000976. PMC 6532692. PMID 10796565.CS1 maint: multiple names: authors list (link)
- Mwengee W; Butler, Thomas; Mgema, Samuel; Mhina, George; Almasi, Yusuf; Bradley, Charles; Formanik, James B.; Rochester, C. George (2006). "Treatment of Plague with Genamicin or Doxycycline in a Randomized Clinical Trial in Tanzania". Clin Infect Dis. 42 (5): 614–21. doi:10.1086/500137. PMID 16447105.
- Drug-resistant plague a 'major threat', say scientists, SciDev.Net.
- "Plague – Madagascar". World Health Organisation. 21 November 2014. Retrieved 26 November 2014.
- "WHO scales up response to plague in Madagascar". World Health Organization (WHO). 1 October 2017. Retrieved 5 October 2017.
- Schama, S. (2000). A History of Britain: At the Edge of the World? 3000BC–AD1603, First Edition, BBC Worldwide, London, p226.
- Wheelis M. (2002). "Biological warfare at the 1346 siege of Caffa". Emerg Infect Dis. 8 (9): 971–75. doi:10.3201/eid0809.010536. PMC 2732530. PMID 12194776.
- Daniel Barenblatt, A plague upon Humanity, HarperCollns, 2004, pp. 220–21
- Tamparo, Carol; Lewis, Marcia (2011). Diseases of the Human Body. Philadelphia, PA: F.A. Davis Company. p. 70. ISBN 9780803625051.
External links
| Wikimedia Commons has media related to Plague. |
- WHO Health topic
- CDC Plague map world distribution, publications, information on bioterrorism preparedness and response regarding plague
- Symptoms, causes, pictures of bubonic plague
| Classification | |
|---|---|
| External resources |
|