Sputum
Sputum is mucus and is the name used for the coughed-up material (phlegm) from the lower airways (trachea and bronchi). In medicine, sputum samples are usually used for naked eye exam, microbiological investigations of respiratory infections, and cytological investigations of respiratory systems. It is critical that the patient not give a specimen that includes any mucoid material from the interior of the nose. Naked eye exam of sputum can be done at home by a patient in order to note the various colors (see below). Any hint of yellow color suggests an airway infection (but does not indicate between the types of organisms causing it). Such color hints are best detected when the sputum is viewed on a very white background such as white paper, a white pot, or a white sink surface. The more intense the yellow color, the more likely it is a bacterial infection (bronchitis, bronchopneumonia, or pneumonia).
| Abnormal sputum | |
|---|---|
| Other names | Mucus |
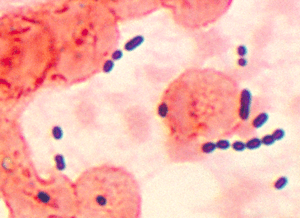 | |
| Cocci-shaped Enterococcus sp. bacteria taken from a pneumonia patient. | |
| Pronunciation |
|
| Specialty | Pulmonology |
Description
The best sputum samples contain very little saliva,[1] as saliva contaminates the sample with oral bacteria. This is especially true for samples for lab testing in cytology or microbiology. Specimen adequacy is assessed by the laboratory technologists by examining a Gram stain or cytology stain of the sputum. More than 25 squamous epithelial cells at low power magnification exam with the microscope strongly suggests salivary contamination.[2] Sputum samples have been used to quantify the degree of airway inflammation in human diseases such as asthma. Specifically, this work has demonstrated that sub group of severe asthma patients have airway inflammation that is resistant to treatment with corticosteroids.[3]
When a sputum specimen is plated out in microbiology, it is best to get the portion of the sample that most looks like yellow pus onto the swab. If there is any blood in the sputum, this should also be on the swab. Microbiological sputum samples are used to look for infections, such as Moraxella catarrhalis, Mycobacterium tuberculosis, Streptococcus pneumoniae, and Haemophilus influenzae. Other pathogens can also be found.
Purulent sputum[4] contains pus, composed of white blood cells, cellular debris, dead tissue, serous fluid, and viscous liquid (mucus). Purulent sputum is typically yellow or green. It is seen in cases of bronchiectasis, lung abscess, or an advanced stage of bronchitis.[5]
Interpretation
Sputum can be (when examined by the naked eye):
- Bloody[4] (hemoptysis)
- Blood-streaked sputum – inflammation of throat (larynx and/or trachea) or bronchi; lung cancer; other bleeding erosions, ulcers, or tumors of the lower airway.
- Pink sputum – sputum evenly mixed with blood from alveoli and/or small peripheral bronchi.
- Massive blood – cavitary tuberculosis or tumor such as lung cancer, or lung abscess; bronchiectasis; lung infarction; pulmonary embolism.
- Green or greenish colored - indicative of longstanding respiratory infection (green from degenerative changes in cell debris) as in pneumonia, ruptured lung abscess, chronic infectious bronchitis, and infected bronchiectasis or cystic fibrosis.
- Rust colored – usually caused by pneumococcal bacteria (in pneumonia), pulmonary embolism, lung cancer or pulmonary tuberculosis.
- Brownish – chronic bronchitis (greenish/yellowish/brown); chronic pneumonia (whitish-brown); tuberculosis; lung cancer.
- Yellow, yellowish purulent – containing pus. "The sputum color of patients with acute cough and no underlying chronic lung disease does not imply therapeutic consequences such as prescription of antibiotics."[6] The color can provide hints as to effective treatment in chronic bronchitis patients:[7]
- A yellow-greenish (mucopurulent) color suggests that treatment with antibiotics can reduce symptoms. The green color is caused by degenerating neutrophil verdoperoxidase.
- Whitish gray sputum color against a white color background (such as a white sink surface) tends to indicate either a specimen from someone who is dehydrated, and/or from an older person, and/or a specimen with a mixed, modest number of eosinophils and maybe some acute inflammatory neutrophil cells (this last choice tends to suggest a chronic allergic bronchitis).
- A white, milky, or opaque (mucoid) appearance means that antibiotics are less likely to be effective in treatment because the likelihood is greater of a viral infection or allergy (even asthma...thick sputum) than of antibiotic-responsive micro-organisms.
- Foamy white – may come from earlier-phase pulmonary edema.
- Frothy pink – may indicate more severe pulmonary edema. Antibiotics may not be necessary at this time.
- Clear – pulmonary embolism (clear to frothy); COPD chronic obstructive pulmonary disease (clear to gray); viral respiratory infection (clear to whitish & sometimes a hint of yellow); asthma (thick and white to yellowish).
See also
References
- Clinical Microbiology procedures handbook, American Society for Microbiology 2nd Ed. 2007 update
- Gershman, Neil H.; Liu, Hong; Wong, Hofer H.; Liu, Jane T.; Fahy, John V. (August 1999). "Fractional analysis of sequential induced sputum samples during sputum induction: Evidence that different lung compartments are sampled at different time points". Journal of Allergy and Clinical Immunology. 104 (2): 322–328. doi:10.1016/S0091-6749(99)70374-X. PMID 10452752.
- Peters, Michael C.; Kerr, Sheena; Dunican, Eleanor M.; Woodruff, Prescott G.; Fajt, Merritt L.; Levy, Bruce D.; Israel, Elliot; Phillips, Brenda R.; Mauger, David T.; Comhair, Suzy A.; Erzurum, Serpil C.; Johansson, Mats W.; Jarjour, Nizar N.; Coverstone, Andrea M.; Castro, Mario; Hastie, Annette T.; Bleecker, Eugene R.; Wenzel, Sally E.; Fahy, John V. (March 2018). "Refractory airway type 2 inflammation in a large subgroup of asthmatic patients treated with inhaled corticosteroids". Journal of Allergy and Clinical Immunology. 143 (1): 104–113.e14. doi:10.1016/j.jaci.2017.12.1009. PMC 6128784. PMID 29524537.
- Richard F. LeBlond; Richard L. DeGowin; Donald E. Brown (2004). DeGowin's diagnostic examination. New York: McGraw-Hill. ISBN 0-07-140923-8.
- https://www.medicalnewstoday.com/articles/318924.php
- Altiner A, Wilm S, Däubener W, Bormann C, Pentzek M, Abholz HH, Scherer M (2009). "Sputum color for diagnosis of a bacterial infection in patients with acute cough". Scand J Prim Health Care. 27 (2): 70–3. doi:10.1080/02813430902759663. PMC 3410464. PMID 19242860.
- Sputum Color is the Key to Treating Acute COPD Exacerbations