Typhoid fever
Typhoid fever, also known simply as typhoid, is a bacterial infection due to a specific type of Salmonella that causes symptoms.[3] Symptoms may vary from mild to severe, and usually begin 6 to 30 days after exposure.[1][2] Often there is a gradual onset of a high fever over several days.[1] This is commonly accompanied by weakness, abdominal pain, constipation, headaches, and mild vomiting.[2][6] Some people develop a skin rash with rose colored spots.[2] In severe cases, people may experience confusion.[6] Without treatment, symptoms may last weeks or months.[2] Diarrhea is uncommon.[6] Other people may carry the bacterium without being affected; however, they are still able to spread the disease to others.[4] Typhoid fever is a type of enteric fever, along with paratyphoid fever.[3]
| Typhoid fever | |
|---|---|
| Other names | Slow fever, typhoid |
 | |
| Rose spots on the chest of a person with typhoid fever | |
| Specialty | Infectious disease |
| Symptoms | Fever, abdominal pain, headache, rash[1] |
| Usual onset | 6–30 days after exposure[1][2] |
| Causes | Salmonella enterica subsp. enterica (spread by food or water contaminated with feces)[3][4] |
| Risk factors | Poor sanitation, poor hygiene.[3] |
| Diagnostic method | Bacterial culture, DNA detection[2][3][5] |
| Differential diagnosis | Other infectious diseases[6] |
| Prevention | Typhoid vaccine, handwashing[2][7] |
| Treatment | Antibiotics[3] |
| Frequency | 12.5 million (2015)[8] |
| Deaths | 149,000 (2015)[9] |
The cause is the bacterium Salmonella enterica subsp. enterica growing in the intestines and blood.[2][6] Typhoid is spread by eating or drinking food or water contaminated with the feces of an infected person.[4] Risk factors include poor sanitation and poor hygiene.[3] Those who travel in the developing world are also at risk.[6] Only humans can be infected.[4] Symptoms are similar to those of many other infectious diseases.[6] Diagnosis is by either culturing the bacteria or detecting their DNA in the blood, stool, or bone marrow.[2][3][5] Culturing the bacterium can be difficult.[10] Bone-marrow testing is the most accurate.[5]
A typhoid vaccine can prevent about 40 to 90% of cases during the first two years.[7] The vaccine may have some effect for up to seven years.[3] For those at high risk or people traveling to areas where the disease is common, vaccination is recommended.[4] Other efforts to prevent the disease include providing clean drinking water, good sanitation, and handwashing.[2][4] Until an individual's infection is confirmed as cleared, the individual should not prepare food for others.[2] The disease is treated with antibiotics such as azithromycin, fluoroquinolones, or third-generation cephalosporins.[3] Resistance to these antibiotics has been developing, which has made treatment of the disease more difficult.[3][11]
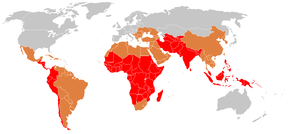
In 2015, 12.5 million new cases worldwide were reported.[8] The disease is most common in India.[3] Children are most commonly affected.[3][4] Rates of disease decreased in the developed world in the 1940s as a result of improved sanitation and use of antibiotics to treat the disease.[4] Each year in the United States, about 400 cases are reported and the disease occurs in an estimated 6,000 people.[6][12] In 2015, it resulted in about 149,000 deaths worldwide – down from 181,000 in 1990 (about 0.3% of the global total).[9][13] The risk of death may be as high as 20% without treatment.[4] With treatment, it is between 1 and 4%.[3][4] Typhus is a different disease.[14] However, the name typhoid means "resembling typhus" due to the similarity in symptoms.[15]
Signs and symptoms

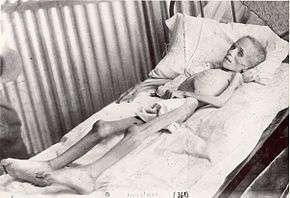
Classically, the progression of untreated typhoid fever is divided into four distinct stages, each lasting about a week. Over the course of these stages, the patient becomes exhausted and emaciated.[16]
- In the first week, the body temperature rises slowly, and fever fluctuations are seen with relative bradycardia (Faget sign), malaise, headache, and cough. A bloody nose (epistaxis) is seen in a quarter of cases, and abdominal pain is also possible. A decrease in the number of circulating white blood cells (leukopenia) occurs with eosinopenia and relative lymphocytosis; blood cultures are positive for Salmonella enterica subsp. enterica or S. paratyphi. The Widal test is usually negative in the first week.[17]
- In the second week, the person is often too tired to get up, with high fever in plateau around 40 °C (104 °F) and bradycardia (sphygmothermic dissociation or Faget sign), classically with a dicrotic pulse wave. Delirium can occur, where the patient is often calm, but sometimes becomes agitated. This delirium has led to typhoid receiving the nickname "nervous fever". Rose spots appear on the lower chest and abdomen in around a third of patients. Rhonchi (rattling breathing sounds) are heard in the base of the lungs. The abdomen is distended and painful in the right lower quadrant, where a rumbling sound can be heard. Diarrhea can occur in this stage, but constipation is also common. The spleen and liver are enlarged (hepatosplenomegaly) and tender, and liver transaminases are elevated. The Widal test is strongly positive, with antiO and antiH antibodies. Blood cultures are sometimes still positive at this stage. The major symptom of this fever is that it usually rises in the afternoon up to the first and second week.
- In the third week of typhoid fever, a number of complications can occur:
- Intestinal haemorrhage due to bleeding in congested Peyer's patches occurs; this can be very serious, but is usually not fatal.
- Intestinal perforation in the distal ileum is a very serious complication and is frequently fatal. It may occur without alarming symptoms until septicaemia or diffuse peritonitis sets in.
- Encephalitis
- Respiratory diseases such as pneumonia and acute bronchitis
- Neuropsychiatric symptoms (described as "muttering delirium" or "coma vigil"), with picking at bedclothes or imaginary objects
- Metastatic abscesses, cholecystitis, endocarditis, and osteitis
- The fever is still very high and oscillates very little over 24 hours. Dehydration ensues, and the patient is delirious (typhoid state). One-third of affected individuals develop a macular rash on the trunk.
- Platelet count goes down slowly and the risk of bleeding rises.
- By the end of third week, the fever starts subsiding.
Causes
Bacteria
The Gram-negative bacterium that causes typhoid fever is Salmonella enterica subsp. enterica.[18] The two main types of the subspecies enterica are ST1 and ST2, based on MLST subtyping scheme, which are currently widespread globally.[19]
Transmission
Unlike other strains of Salmonella, no animal carriers of typhoid are known.[20] Humans are the only known carriers of the bacteria.[20] S. e. subsp. enterica is spread through the fecal-oral route from individuals who are currently infected and from asymptomatic carriers of the bacteria.[20] An asymptomatic human carrier is an individual who is still excreting typhoid bacteria in their stool a year after the acute stage of the infection.[20]
Diagnosis
Diagnosis is made by any blood, bone marrow, or stool cultures and with the Widal test (demonstration of antibodies against Salmonella antigens O-somatic and H-flagellar). In epidemics and less wealthy countries, after excluding malaria, dysentery, or pneumonia, a therapeutic trial time with chloramphenicol is generally undertaken while awaiting the results of the Widal test and cultures of the blood and stool.[21]
Widal test

Widal test is used to identify specific antibodies in serum of people with typhoid by using antigen-antibody interactions.
In this test, the serum is mixed with a dead bacterial suspension of salmonella having specific antigens on it. If the patient's serum is carrying antibodies against those antigens then they get attached to them forming clumping which indicated the positivity of the test. If clumping does not occur then the test is negative. The Widal test is time-consuming and prone to significant false positive results. The test may also be falsely negative in the early course of illness. However, unlike the Typhidot test, the Widal test quantifies the specimen with titres.[22]
Typhidot
The test is based on the presence of specific IgM and IgG antibodies to a specific 50Kd OMP antigen.This test is carried out on a cellulose nitrate membrane where a specific S.typhi outer membrane protein is attached as fixed test lines.It separately identifies IgM and IgG antibodies. IgM shows recent infection whereas IgG signifies remote infection.
The sample pad of this kit contains colloidal gold-anti-human IgG or gold-anti-human IgM. If the sample contains IgG and IgM antibodies against those antigens then they will react and get turned into red color. This complex will continue to move forward and the IgG and IgM antibodies will get attached to the first test line where IgG and IgM antigens are present giving a pink-purplish colored band. This complex will continue to move further and reach the control line which consists of rabbit anti-mouse antibody which bends the mouse anti-human IgG or IgM antibodies. The main purpose of the control line is to indicate a proper migration and reagent color. The typhidot test becomes positive within 2–3 days of infection.
Two colored bands indicate a positive test. Single-band of control line indicates a negative test. Single-band of first fixed line or no bands at all indicates invalid tests. The most important limitation of this test is that it is not quantitative and the result is only positive or negative.[23]
Tubex test
Tubex test contains two types of particles brown magnetic particles coated with antigen and blue indicator particles coated with O9 antibody. During the test, if antibodies are present in the serum then they will get attached to the brown magnetic particles and settle down at the base and the blue indicator particles remain up in the solution giving a blue color that indicates positivity of the test.
If the serum does not have an antibody in it then the blue particle gets attached to the brown particles and settled down at the bottom giving no color to the solution which means the test is negative and they do not have typhoid.[24]
Prevention

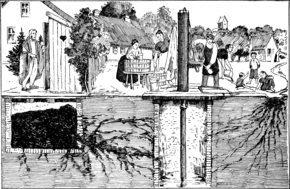
Sanitation and hygiene are important to prevent typhoid. It can only spread in environments where human feces are able to come into contact with food or drinking water. Careful food preparation and washing of hands are crucial to prevent typhoid. Industrialization, and in particular, the invention of the automobile, contributed greatly to the elimination of typhoid fever, as it eliminated the public-health hazards associated with having horse manure in public streets, which led to large number of flies,[25] which are known as vectors of many pathogens, including Salmonella spp.[26] According to statistics from the United States Centers for Disease Control and Prevention, the chlorination of drinking water has led to dramatic decreases in the transmission of typhoid fever in the United States.
Vaccination
Two typhoid vaccines are licensed for use for the prevention of typhoid:[7] the live, oral Ty21a vaccine (sold as Vivotif by Crucell Switzerland AG) and the injectable typhoid polysaccharide vaccine (sold as Typhim Vi by Sanofi Pasteur and Typherix by GlaxoSmithKline). Both are efficacious and recommended for travellers to areas where typhoid is endemic. Boosters are recommended every five years for the oral vaccine and every two years for the injectable form.[7] An older, killed whole-cell vaccine is still used in countries where the newer preparations are not available, but this vaccine is no longer recommended for use because it has a higher rate of side effects (mainly pain and inflammation at the site of the injection).[27]
To help decrease rates of typhoid fever in developing nations, the World Health Organization (WHO) endorsed the use of a vaccination program starting in 1999. Vaccinations have proven to be a great way at controlling outbreaks in high incidence areas. Just as important, it is also very cost-effective. Vaccination prices are normally low, less than US $1 per dose. Because the price is low, poverty-stricken communities are more willing to take advantage of the vaccinations.[28] Although vaccination programs for typhoid have proven to be effective, they alone cannot eliminate typhoid fever.[28] Combining the use of vaccines with increasing public health efforts is the only proven way to control this disease.[28]
Since the 1990s, two typhoid fever vaccines have been recommended by the WHO. The ViPS vaccine is given via injection, while the Ty21a is taken through capsules. Only people 2 years or older are recommended to be vaccinated with the ViPS vaccine, and it requires a revaccination after 2–3 years with a 55–72% vaccine efficacy. The alternative Ty21a vaccine is recommended for people 5 years or older, and has a 5-7-year duration with a 51–67% vaccine efficacy. The two different vaccines have been proven as a safe and effective treatment for epidemic disease control in multiple regions.[28]
A version combined with hepatitis A is also available.[29]
Treatment
Oral rehydration therapy
The rediscovery of oral rehydration therapy in the 1960s provided a simple way to prevent many of the deaths of diarrheal diseases in general.
Antibiotics
Where resistance is uncommon, the treatment of choice is a fluoroquinolone such as ciprofloxacin.[30][31] Otherwise, a third-generation cephalosporin such as ceftriaxone or cefotaxime is the first choice.[32][33][34][35] Cefixime is a suitable oral alternative.[36][37]
Typhoid fever, when properly treated, is not fatal in most cases. Antibiotics, such as ampicillin, chloramphenicol, trimethoprim-sulfamethoxazole, amoxicillin, and ciprofloxacin, have been commonly used to treat typhoid fever.[38] Treatment of the disease with antibiotics reduces the case-fatality rate to about 1%.[39]
Without treatment, some patients develop sustained fever, bradycardia, hepatosplenomegaly, abdominal symptoms, and occasionally, pneumonia. In white-skinned patients, pink spots, which fade on pressure, appear on the skin of the trunk in up to 20% of cases. In the third week, untreated cases may develop gastrointestinal and cerebral complications, which may prove fatal in up to 10–20% of cases. The highest case fatality rates are reported in children under 4 years. Around 2–5% of those who contract typhoid fever become chronic carriers, as bacteria persist in the biliary tract after symptoms have resolved.[40]
Surgery
Surgery is usually indicated if intestinal perforation occurs. One study found a 30-day mortality rate of 9% (8/88), and surgical site infections at 67% (59/88), with the disease burden borne predominantly by low-resource countries.[41]
For surgical treatment, most surgeons prefer simple closure of the perforation with drainage of the peritoneum. Small-bowel resection is indicated for patients with multiple perforations. If antibiotic treatment fails to eradicate the hepatobiliary carriage, the gallbladder should be resected. Cholecystectomy is not always successful in eradicating the carrier state because of persisting hepatic infection.
Resistance
As resistance to ampicillin, chloramphenicol, trimethoprim-sulfamethoxazole, and streptomycin is now common, these agents have not been used as first–line treatment of typhoid fever for almost 20 years. Typhoid resistant to these agents is known as multidrug-resistant typhoid.
Ciprofloxacin resistance is an increasing problem, especially in the Indian subcontinent and Southeast Asia. Many centres are shifting from using ciprofloxacin as the first line for treating suspected typhoid originating in South America, India, Pakistan, Bangladesh, Thailand, or Vietnam. For these people, the recommended first-line treatment is ceftriaxone. Also, azithromycin has been suggested to be better at treating resistant typhoid in populations than both fluoroquinolone drugs and ceftriaxone.[31] Azithromycin significantly reduces relapse rates compared with ceftriaxone.
A separate problem exists with laboratory testing for reduced susceptibility to ciprofloxacin; current recommendations are that isolates should be tested simultaneously against ciprofloxacin (CIP) and against nalidixic acid (NAL), and that isolates that are sensitive to both CIP and NAL should be reported as "sensitive to ciprofloxacin", but that isolates testing sensitive to CIP but not to NAL should be reported as "reduced sensitivity to ciprofloxacin". However, an analysis of 271 isolates showed that around 18% of isolates with a reduced susceptibility to ciprofloxacin (MIC 0.125–1.0 mg/l) would not be picked up by this method.[42] How this problem can be solved is not certain, because most laboratories around the world (including the West) are dependent on disk testing and cannot test for MICs.
Epidemiology
In 2000, typhoid fever caused an estimated 21.7 million illnesses and 217,000 deaths.[5] It occurs most often in children and young adults between 5 and 19 years old.[43] In 2013, it resulted in about 161,000 deaths – down from 181,000 in 1990.[13] Infants, children, and adolescents in south-central and Southeast Asia experience the greatest burden of illness.[44] Outbreaks of typhoid fever are also frequently reported from sub-Saharan Africa and countries in Southeast Asia.[45][46][47] In the United States, about 400 cases occur each year, and 75% of these are acquired while traveling internationally.[48][49]
Historically, before the antibiotic era, the case fatality rate of typhoid fever was 10–20%. Today, with prompt treatment, it is less than 1%.[50] However, about 3–5% of individuals who are infected develop a chronic infection in the gall bladder.[51] Since S. e. subsp. enterica is human-restricted, these chronic carriers become the crucial reservoir, which can persist for decades for further spread of the disease, further complicating the identification and treatment of the disease.[52] Lately, the study of S. e. subsp. enterica associated with a large outbreak and a carrier at the genome level provides new insights into the pathogenesis of the pathogen.[53][54]
In industrialized nations, water sanitation and food handling improvements have reduced the number of cases.[55] Developing nations, such as those found in parts of Asia and Africa, have the highest rates of typhoid fever. These areas have a lack of access to clean water, proper sanitation systems, and proper health-care facilities. For these areas, such access to basic public-health needs is not in the near future.[56]
Twenty-first century
In 2004–05 an outbreak in the Democratic Republic of Congo resulted in more than 42,000 cases and 214 deaths.[43] Since November 2016, Pakistan has had an outbreak of extensively drug-resistant (XDR) typhoid fever.[57]
Twentieth century

In 1902, guests at mayoral banquets in Southampton and Winchester, England, became ill and four died, including the Dean of Winchester, after consuming oysters. The infection was due to oysters sourced from Emsworth, where the oyster beds had been contaminated with raw sewage.[58][59]
The most notorious carrier of typhoid fever, but by no means the most destructive, was Mary Mallon, also known as Typhoid Mary. In 1907, she became the first carrier in the United States to be identified and traced. She was a cook in New York, who was closely associated with 53 cases and three deaths.[60]
History
Spread
During the course of treatment of a typhoid outbreak in a local village in 1838, English country doctor William Budd realised the "poisons" involved in infectious diseases multiplied in the intestines of the sick, were present in their excretions, and could be transmitted to the healthy through their consumption of contaminated water.[61] He proposed strict isolation or quarantine as a method for containing such outbreaks in the future.[62] The medical and scientific communities did not identify the role of microorganisms in infectious disease until the work of Robert Koch and Louis Pasteur.
Organism involved
In 1880, Karl Joseph Eberth described a bacillus that he suspected was the cause of typhoid.[63][64][65] In 1884, pathologist Georg Theodor August Gaffky (1850–1918) confirmed Eberth's findings,[66] and the organism was given names such as Eberth's bacillus, Eberthella Typhi, and Gaffky-Eberth bacillus. Today, the bacillus that causes typhoid fever goes by the scientific name Salmonella enterica enterica, serovar Typhi.
Vaccine
British bacteriologist Almroth Edward Wright first developed an effective typhoid vaccine at the Army Medical School in Netley, Hampshire. It was introduced in 1896 and used successfully by the British during the Boer War in South Africa.[67] At that time, typhoid often killed more soldiers at war than were lost due to enemy combat. Wright further developed his vaccine at a newly opened research department at St Mary's Hospital Medical School in London from 1902, where he established a method for measuring protective substances (opsonin) in human blood.
Citing the example of the Second Boer War, during which many soldiers died from easily preventable diseases, Wright convinced the British Army that 10 million vaccine doses should be produced for the troops being sent to the Western Front, thereby saving up to half a million lives during World War I.[68] The British Army was the only combatant at the outbreak of the war to have its troops fully immunized against the bacterium. For the first time, their casualties due to combat exceeded those from disease.[69]
In 1909, Frederick F. Russell, a U.S. Army physician, adopted Wright's typhoid vaccine for use with the Army, and two years later, his vaccination program became the first in which an entire army was immunized. It eliminated typhoid as a significant cause of morbidity and mortality in the U.S. military.[70]
Chlorination of water
Most developed countries had declining rates of typhoid fever throughout the first half of the 20th century due to vaccinations and advances in public sanitation and hygiene. In 1893 attempts were made to chlorinate the water supply in Hamburg, Germany and in 1897 Maidstone, England was the first town to have its entire water supply chlorinated.[71] In 1905, following an outbreak of typhoid fever, the City of Lincoln, England instituted permanent water chlorination.[72] The first permanent disinfection of drinking water in the US was made in 1908 to the Jersey City, New Jersey, water supply. Credit for the decision to build the chlorination system has been given to John L. Leal.[73] The chlorination facility was designed by George W. Fuller.[74]
Antibiotics
In 1942, doctors introduced antibiotics in clinical practice, greatly reducing mortality.
Terminology
The disease has been referred to by various names, often associated with symptoms, such as gastric fever, enteric fever, abdominal typhus, infantile remittant fever, slow fever, nervous fever, and pythogenic fever.[75]
Notable cases
- William Henry Harrison, the 9th President of the United States of America, died 32 days into his term, in 1841. This is the shortest term served by a United States President.
- Stephen A. Douglas, political opponent of Abraham Lincoln in 1858 and 1860, died of typhoid on June 3, 1861.
- William Wallace Lincoln, the son of US president Abraham and Mary Todd Lincoln, died of typhoid in 1862.[76]
- Edward VII of the UK, while still Prince of Wales, had a near fatal case of typhoid fever in 1871.[77] It was thought at the time that his father, the Prince Consort Albert, had also died of typhoid fever (in 1861)[78] but this is disputed.
- Leland Stanford Jr., son of American tycoon and politician A. Leland Stanford and eponym of Leland Stanford Junior University, died of typhoid fever in 1884 at the age of 15.[79]
- Gerard Manley Hopkins, English poet, died of typhoid fever in 1889.[80]
- Lizzie van Zyl, South African child inmate of the Bloemfontein concentration camp during the Second Boer War, died of typhoid fever in 1901.
- Dr HJH 'Tup' Scott, captain of the 1886 Australian cricket team that toured England, died of typhoid in 1910.[81]
- Arnold Bennett, English novelist, died in 1932 of typhoid, two months after drinking a glass of water in a Paris hotel to prove it was safe.[82]
- Hakaru Hashimoto, Japanese medical scientist, died of typhoid fever in 1934.[83]
- Lourdes Van-Dúnem, Angolan singer, died of typhoid in 2006.[84]
- Heath Bell, a relief pitcher for the San Diego Padres, acquired typhoid on a 2010 trip to Fiji, and survived.[85]
References
- Anna E. Newton (2014). "3 Infectious Diseases Related To Travel". CDC health information for international travel 2014 : the yellow book. ISBN 9780199948499. Archived from the original on 2015-07-02.
- "Typhoid Fever". cdc.gov. May 14, 2013. Archived from the original on 6 June 2016. Retrieved 28 March 2015.
- Wain J, Hendriksen RS, Mikoleit ML, Keddy KH, Ochiai RL (March 2015). "Typhoid fever". Lancet. 385 (9973): 1136–45. doi:10.1016/s0140-6736(13)62708-7. PMID 25458731.
- "Typhoid vaccines: WHO position paper" (PDF). Releve Epidemiologique Hebdomadaire. 83 (6): 49–59. February 2008. PMID 18260212. Archived (PDF) from the original on April 2, 2015.
- Crump JA, Mintz ED (January 2010). "Global trends in typhoid and paratyphoid Fever". Clinical Infectious Diseases. 50 (2): 241–6. doi:10.1086/649541. PMC 2798017. PMID 20014951.
- "Typhoid Fever". cdc.gov. May 14, 2013. Archived from the original on 2 April 2015. Retrieved 28 March 2015.
- Milligan R, Paul M, Richardson M, Neuberger A (May 2018). "Vaccines for preventing typhoid fever". The Cochrane Database of Systematic Reviews. 5: CD001261. doi:10.1002/14651858.CD001261.pub4. PMC 6494485. PMID 29851031.
- Vos, Theo; Allen, Christine; Arora, Megha; Barber, Ryan M.; Bhutta, Zulfiqar A.; Brown, Alexandria; Carter, Austin; Casey, Daniel C.; Charlson, Fiona J.; Chen, Alan Z.; Coggeshall, Megan; Cornaby, Leslie; Dandona, Lalit; Dicker, Daniel J.; Dilegge, Tina; Erskine, Holly E.; Ferrari, Alize J.; Fitzmaurice, Christina; Fleming, Tom; Forouzanfar, Mohammad H.; Fullman, Nancy; Gething, Peter W.; Goldberg, Ellen M.; Graetz, Nicholas; Haagsma, Juanita A.; Hay, Simon I.; Johnson, Catherine O.; Kassebaum, Nicholas J.; Kawashima, Toana; et al. (October 2016). "Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1545–1602. doi:10.1016/S0140-6736(16)31678-6. PMC 5055577. PMID 27733282.
- Wang, Haidong; Naghavi, Mohsen; Allen, Christine; Barber, Ryan M.; Bhutta, Zulfiqar A.; Carter, Austin; Casey, Daniel C.; Charlson, Fiona J.; Chen, Alan Zian; Coates, Matthew M.; Coggeshall, Megan; Dandona, Lalit; Dicker, Daniel J.; Erskine, Holly E.; Ferrari, Alize J.; Fitzmaurice, Christina; Foreman, Kyle; Forouzanfar, Mohammad H.; Fraser, Maya S.; Fullman, Nancy; Gething, Peter W.; Goldberg, Ellen M.; Graetz, Nicholas; Haagsma, Juanita A.; Hay, Simon I.; Huynh, Chantal; Johnson, Catherine O.; Kassebaum, Nicholas J.; Kinfu, Yohannes; et al. (October 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1459–1544. doi:10.1016/s0140-6736(16)31012-1. PMC 5388903. PMID 27733281.
- Alan J. Magill (2013). Hunter's tropical medicine and emerging infectious diseases (9th ed.). London: Saunders/Elsevier. pp. 568–572. ISBN 9781455740437. Archived from the original on 2017-02-28.
- Chatham-Stephens K, Medalla F, Hughes M, Appiah GD, Aubert RD, Caidi H, et al. (January 2019). "Emergence of Extensively Drug-Resistant Salmonella Typhi Infections Among Travelers to or from Pakistan - United States, 2016-2018". MMWR. Morbidity and Mortality Weekly Report. 68 (1): 11–13. doi:10.15585/mmwr.mm6801a3. PMC 6342547. PMID 30629573.
- Jackson BR, Iqbal S, Mahon B (March 2015). "Updated recommendations for the use of typhoid vaccine--Advisory Committee on Immunization Practices, United States, 2015". MMWR. Morbidity and Mortality Weekly Report. 64 (11): 305–8. PMC 4584884. PMID 25811680.
- GBD 2013 Mortality Causes of Death Collaborators (January 2015). "Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013". Lancet. 385 (9963): 117–71. doi:10.1016/S0140-6736(14)61682-2. PMC 4340604. PMID 25530442.
- Cunha BA (March 2004). "Osler on typhoid fever: differentiating typhoid from typhus and malaria". Infectious Disease Clinics of North America. 18 (1): 111–25. doi:10.1016/S0891-5520(03)00094-1. PMID 15081508.
- "Oxford English Dictionary (Online)". p. typhoid, adj. and n. Archived from the original on 11 January 2008. Retrieved 28 March 2015.
Resembling or characteristic of typhus
- "Typhoid". Merriam Webster Dictionary. Archived from the original on 2013-07-02. Retrieved 2013-06-24.
- Kumar P, Kumar R (March 2017). "Enteric Fever". Indian Journal of Pediatrics. 84 (3): 227–230. doi:10.1007/s12098-016-2246-4. PMID 27796818.
- "Typhoid Fever Information for Health Professionals". CDC. May 14, 2013. Archived from the original on 20 August 2016. Retrieved 20 August 2016.
- Yap KP, Ho WS, Gan HM, Chai LC, Thong KL (2016). "Global MLST of Salmonella Typhi Revisited in Post-genomic Era: Genetic Conservation, Population Structure, and Comparative Genomics of Rare Sequence Types". Frontiers in Microbiology. 7: 270. doi:10.3389/fmicb.2016.00270. PMC 4774407. PMID 26973639.
- Eng SK, Pusparajah P, Ab Mutalib NS, Ser HL, Chan KG, Lee LH (June 2015). "Salmonella:A review on pathogenesis, epidemiology and antibiotic resistance". Frontiers in Life Science. 8 (3): 284–293. doi:10.1080/21553769.2015.1051243.
- Ryan KJ, Ray CG, eds. (2004). Sherris Medical Microbiology (4th ed.). McGraw Hill. ISBN 978-0-8385-8529-0.
- "Widal Test - an overview | ScienceDirect Topics". www.sciencedirect.com. Retrieved 2019-11-14.
- Lim, Pak-Leong; Tam, Frankie C. H.; Cheong, Yuet-Meng; Jegathesan, M. (August 1998). "One-Step 2-Minute Test To Detect Typhoid-Specific Antibodies Based on Particle Separation in Tubes". Journal of Clinical Microbiology. 36 (8): 2271–2278. ISSN 0095-1137. PMC 105030. PMID 9666004.
- "TYPHIDOT Rapid IgG/IgM (Combo)" (PDF). Reszon Diagnostics International. Retrieved 14 November 2019.
- "The Great Horse Manure Crisis of 1894". Archived from the original on 2015-05-25.
- Cirillo VJ (2006). ""Winged sponges": houseflies as carriers of typhoid fever in 19th- and early 20th-century military camps". Perspectives in Biology and Medicine. 49 (1): 52–63. doi:10.1353/pbm.2006.0005. PMID 16489276.
- Marathe SA, Lahiri A, Negi VD, Chakravortty D (2012). "Typhoid fever & vaccine development: a partially answered question". The Indian Journal of Medical Research. 135 (2): 161–9. PMC 3336846. PMID 22446857.
- Date KA, Bentsi-Enchill A, Marks F, Fox K (June 2015). "Typhoid fever vaccination strategies". Vaccine. 33 Suppl 3: C55–61. doi:10.1016/j.vaccine.2015.04.028. PMID 25902360.
- health, NPS: Better choices, Better. "Vivaxim Solution for injection". NPS MedicineWise. Archived from the original on 1 October 2015. Retrieved 10 April 2017.
- Parry CM, Beeching NJ (June 2009). "Treatment of enteric fever". BMJ. 338: b1159. doi:10.1136/bmj.b1159. PMID 19493937.
- Effa EE, Lassi ZS, Critchley JA, Garner P, Sinclair D, Olliaro PL, Bhutta ZA (October 2011). "Fluoroquinolones for treating typhoid and paratyphoid fever (enteric fever)". The Cochrane Database of Systematic Reviews (10): CD004530. doi:10.1002/14651858.CD004530.pub4. PMC 6532575. PMID 21975746.
- Soe GB, Overturf GD (1987). "Treatment of typhoid fever and other systemic salmonelloses with cefotaxime, ceftriaxone, cefoperazone, and other newer cephalosporins". Reviews of Infectious Diseases. 9 (4): 719–36. doi:10.1093/clinids/9.4.719. JSTOR 4454162. PMID 3125577.
- Wallace MR, Yousif AA, Mahroos GA, Mapes T, Threlfall EJ, Rowe B, Hyams KC (December 1993). "Ciprofloxacin versus ceftriaxone in the treatment of multiresistant typhoid fever". European Journal of Clinical Microbiology & Infectious Diseases. 12 (12): 907–10. doi:10.1007/BF01992163. PMID 8187784.
- Dutta P, Mitra U, Dutta S, De A, Chatterjee MK, Bhattacharya SK (June 2001). "Ceftriaxone therapy in ciprofloxacin treatment failure typhoid fever in children". The Indian Journal of Medical Research. 113: 210–3. PMID 11816954.
- Коваленко А.Н.; et al. (2011). "Особенности клиники, диагностики и лечения брюшного тифа у лиц молодого возраста". Voen.-meditsinskii Zhurnal. 332 (1): 33–39.
- Bhutta ZA, Khan IA, Molla AM (November 1994). "Therapy of multidrug-resistant typhoid fever with oral cefixime vs. intravenous ceftriaxone". The Pediatric Infectious Disease Journal. 13 (11): 990–4. doi:10.1097/00006454-199411000-00010. PMID 7845753.
- Cao XT, Kneen R, Nguyen TA, Truong DL, White NJ, Parry CM (March 1999). "A comparative study of ofloxacin and cefixime for treatment of typhoid fever in children. The Dong Nai Pediatric Center Typhoid Study Group". The Pediatric Infectious Disease Journal. 18 (3): 245–8. doi:10.1097/00006454-199903000-00007. PMID 10093945.
- Baron S et al.
- "Diarrhoeal Diseases (Updated February 2009)". Archived from the original on November 2, 2011. Retrieved 2013-04-25.. World Health Organization
- "WHO | Typhoid fever". www.who.int. Archived from the original on 2017-07-27. Retrieved 2017-08-10.
- GlobalSurg Collaborative (October 2018). "Management and Outcomes Following Surgery for Gastrointestinal Typhoid: An International, Prospective, Multicentre Cohort Study". World Journal of Surgery. 42 (10): 3179–3188. doi:10.1007/s00268-018-4624-8. PMC 6132852. PMID 29725797.
- Cooke FJ, Wain J, Threlfall EJ (August 2006). "Fluoroquinolone resistance in Salmonella Typhi". BMJ. 333 (7563): 353–4. doi:10.1136/bmj.333.7563.353-b. PMC 1539082. PMID 16902221.
- "Typhoid Fever". World Health Organization. Archived from the original on 2011-11-02. Retrieved 2007-08-28.
- Crump JA, Luby SP, Mintz ED (2004). "The global burden of typhoid fever". Bull World Health Organ. 82 (5): 346–353. PMC 2622843. PMID 15298225.
- Muyembe-Tamfum JJ, Veyi J, Kaswa M, Lunguya O, Verhaegen J, Boelaert M (January 2009). "An outbreak of peritonitis caused by multidrug-resistant Salmonella Typhi in Kinshasa, Democratic Republic of Congo". Travel Medicine and Infectious Disease. 7 (1): 40–3. doi:10.1016/j.tmaid.2008.12.006. PMID 19174300.
- Baddam R, Kumar N, Thong KL, Ngoi ST, Teh CS, Yap KP, et al. (July 2012). "Genetic fine structure of a Salmonella enterica serovar Typhi strain associated with the 2005 outbreak of typhoid fever in Kelantan, Malaysia". Journal of Bacteriology. 194 (13): 3565–6. doi:10.1128/jb.00581-12. PMC 3434757. PMID 22689247.
- Yap KP, Teh CS, Baddam R, Chai LC, Kumar N, Avasthi TS, et al. (September 2012). "Insights from the genome sequence of a Salmonella enterica serovar Typhi strain associated with a sporadic case of typhoid fever in Malaysia". Journal of Bacteriology. 194 (18): 5124–5. doi:10.1128/jb.01062-12. PMC 3430317. PMID 22933756.
- Matano, Leigh M.; Morris, Heidi G.; Wood, B. McKay; Meredith, Timothy C.; Walker, Suzanne (12 15, 2016). "Accelerating the discovery of antibacterial compounds using pathway-directed whole cell screening". Bioorganic & Medicinal Chemistry. 24 (24): 6307–6314. doi:10.1016/j.bmc.2016.08.003. ISSN 1464-3391. PMC 5180449. PMID 27594549. Check date values in:
|date=(help) - http://www.floridahealth.gov/diseases-and-conditions/disease-reporting-and-management/disease-reporting-and-surveillance/_documents/gsi-typhoid-fever.pdf
- Heymann, David L., ed. (2008), Control of Communicable Diseases Manual, Washington, D.C.: American Public Health Association, pg 665. ISBN 978-0-87553-189-2.
- Levine MM, Black RE, Lanata C (December 1982). "Precise estimation of the numbers of chronic carriers of Salmonella typhi in Santiago, Chile, an endemic area". The Journal of Infectious Diseases. 146 (6): 724–6. doi:10.1093/infdis/146.6.724. PMID 7142746.
- Gonzalez-Escobedo G, Marshall JM, Gunn JS (January 2011). "Chronic and acute infection of the gall bladder by Salmonella Typhi: understanding the carrier state". Nature Reviews. Microbiology. 9 (1): 9–14. doi:10.1038/nrmicro2490. PMC 3255095. PMID 21113180.
- Yap KP, Gan HM, Teh CS, Baddam R, Chai LC, Kumar N, et al. (November 2012). "Genome sequence and comparative pathogenomics analysis of a Salmonella enterica Serovar Typhi strain associated with a typhoid carrier in Malaysia". Journal of Bacteriology. 194 (21): 5970–1. doi:10.1128/jb.01416-12. PMC 3486090. PMID 23045488.
- Yap KP, Gan HM, Teh CS, Chai LC, Thong KL (November 2014). "Comparative genomics of closely related Salmonella enterica serovar Typhi strains reveals genome dynamics and the acquisition of novel pathogenic elements". BMC Genomics. 15 (1): 1007. doi:10.1186/1471-2164-15-1007. PMC 4289253. PMID 25412680.
- Crump JA, Sjölund-Karlsson M, Gordon MA, Parry CM (October 2015). "Epidemiology, Clinical Presentation, Laboratory Diagnosis, Antimicrobial Resistance, and Antimicrobial Management of Invasive Salmonella Infections". Clinical Microbiology Reviews. 28 (4): 901–37. doi:10.1128/CMR.00002-15. PMC 4503790. PMID 26180063.
- Khan MI, Pach A, Khan GM, Bajracharya D, Sahastrabuddhe S, Bhutta W, et al. (June 2015). "Typhoid vaccine introduction: An evidence-based pilot implementation project in Nepal and Pakistan". Vaccine. 33 Suppl 3: C62–7. doi:10.1016/j.vaccine.2015.03.087. PMID 25937612.
- "Extensively Drug-Resistant Typhoid Fever in Pakistan". Centers for Disease Control and Prevention. 30 September 2019.
- "Emsworth Oysters". Emsworth Business Association. 10 February 2019. Archived from the original on 3 February 2016.
- Bulstrode, H. Timbrell (1903). "Dr. H. Timbrell Bulstrode's report to the Local Government Board upon alleged oyster-borne enteric fever and other illness following the mayoral banquets at Winchester and Southampton, and upon enteric fever occurring simultaneously elsewhere and also ascribed to oysters". London: HMSO: 1. Archived from the original on 7 July 2019. Cite journal requires
|journal=(help) - "Nova: The Most Dangerous Woman in America". Archived from the original on 2010-04-26.
- Asimov, Asimov's Biographical Encyclopedia of Science and Technology 2nd Revised edition
- Aronson SM (November 1995). "William Budd and typhoid fever". Rhode Island Medicine. 78 (11): 310. PMID 8547718.
- C. J. Eberth (1880) "Die Organismen in den Organen bei Typhus abdominalis" (Organisms in the [internal] organs in cases of Typhus abdominalis), Archiv für pathologische Anatomie und Physiologie, 81 : 58–74.
- C. J. Eberth (1881) "Neue Untersuchungen über den Bacillus des Abdominaltyphus" (New investigations into the bacilli of abdominal typhoid), Archiv für pathologische Anatomie und Physiologie, 83 : 486–501.
- Eberth's findings were verified by Robert Koch: Koch, Robert (1881) "Zur Untersuchung von pathogenen Organismen" Archived 2017-04-23 at the Wayback Machine (On the investigation of pathogenic organisms), Mitteilungen aus dem Kaiserlichen Gesundheitsamte, 1 : 1–49; see p. 45. Archived 2017-04-23 at the Wayback Machine
- Gaffky (1884) "Zur Aetiology des Abdominaltyphus" Archived 2017-04-23 at the Wayback Machine (On the etiology of abdominal typhus), Mittheilungen aus dem Kaiserlichen Gesundheitsamte, 2 : 372–420.
- "Sir Almroth Edward Wright". Encyclopædia Britannica. Archived from the original on 2013-11-11.
- "Library and Archive Catalogue". Royal Society. Retrieved 1 November 2010.
- "Medical lessons from World War I underscore need to keep developing antimicrobial drugs". MinnPost. 2014-11-11. Archived from the original on 30 January 2016. Retrieved 8 September 2017.
- USAMRMC: 50 Years of Dedication to the Warfighter 1958–2008 (PDF). U.S. Army Medical Research & Material Command (2008). 2008. p. 5. ASIN B003WYKJNY. Archived (PDF) from the original on 2013-02-14.
- "Typhoid Epidemic at Maidstone". Journal of the Sanitary Institute. 18: 388. October 1897.
- "A miracle for public health?". Retrieved 2012-12-17.
- Leal, John L. (1909). "The Sterilization Plant of the Jersey City Water Supply Company at Boonton, N.J." Proceedings American Water Works Association. pp. 100–9.
- Fuller, George W. (1909). "Description of the Process and Plant of the Jersey City Water Supply Company for the Sterilization of the Water of the Boonton Reservoir." Proceedings American Water Works Association. 110-34.
- "Typhoid Fever | Center for Emerging and Re-emerging Infectious Diseases | University of Washington". cerid.uw.edu. Retrieved 2019-12-08.
- Dennis, Brady; Dennis, Brady (2011-09-29). "Willie Lincoln's death: A private agony for a president facing a nation of pain". The Washington Post. ISSN 0190-8286. Archived from the original on 2017-04-01. Retrieved 2017-03-12.
- Matthew, H. C. G. (September 2004; online edition May 2006) "Edward VII (1841–1910)" Archived 2016-03-02 at the Wayback Machine, Oxford Dictionary of National Biography, Oxford University Press, doi:10.1093/ref:odnb/32975, retrieved 24 June 2009 (subscription or UK public library membership required)
- Paulley JW (December 1993). "The death of Albert Prince Consort: the case against typhoid fever". The Quarterly Journal of Medicine. 86 (12): 837–41. doi:10.1093/oxfordjournals.qjmed.a068768. PMID 8108541. Archived from the original on 2015-12-08.
- "A History of Stanford". Stanford University. Retrieved 4 July 2018.
- Ruggles, Eleanor (1944) Gerard Manley Hopkins: A Life. Norton.
- Scott, Belinda F.. (1910-09-23) Biography – Henry James Herbert Scott – Australian Dictionary of Biography Archived 2011-02-21 at the Wayback Machine. Adbonline.anu.edu.au. Retrieved on 2014-05-12.
- "Straw for Silence". The Spectator. Vol. 203. F.C. Westley. 1959. ISSN 0038-6952. OCLC 1766325. Retrieved March 16, 2011.
- Hakaru Hashimoto#Biography
- "Angolan singer Lourdes Van-Dunem dies of typhoid". 2006. Archived from the original on 4 March 2016. Retrieved 23 October 2015.
- "Heath Bell Recovering After Bout With Typhoid Fever on Vacation". AOL News. 2011. Archived from the original on 2 March 2013. Retrieved 17 October 2011.
Further reading
- Easmon C (2005-04-01). "Typhoid fever and paratyphoid fever". Travel Health. Retrieved 2008-10-05.
- Harrison NG. "Walter Reed and Typhoid Fever, 1897–1911". Univ. of Virginia. Archived from the original on 2009-09-08. Retrieved 2008-10-05.
- Nicolson, Stuart (2008-06-26). "Typhoid left city (Aberdeen) 'under siege'". BBC News. Retrieved 2008-10-05.
- O'Hara C (2006-01-26). "Typhoid Fever Led To The Fall Of Athens". Elsevier. Retrieved 2008-10-05.
External links
| Wikimedia Commons has media related to: |
| Classification | |
|---|---|
| External resources |