Peritoneal mesothelioma
Peritoneal mesothelioma is the name given to the cancer that attacks the lining of the abdomen. This type of cancer affects the lining that protects the contents of the abdomen and which also provides a lubricating fluid to enable the organs to move and work properly.
| Peritoneal mesothelioma | |
|---|---|
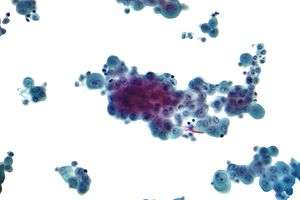 | |
| Micrograph of a cytopathology specimen showing mesothelioma. The cytopathologic appearance of mesothelioma in the pleural cavity and peritoneal cavity is not distinguishable. | |
| Specialty | Oncology |
The peritoneum is made of two parts, the visceral and parietal peritoneum. The visceral peritoneum covers the internal organs and makes up most of the outer layer of the intestinal tract. Covering the abdominal cavity is the parietal peritoneum.
Symptoms
Symptoms of peritoneal mesothelioma include weight loss and abdominal pain and swelling due to a buildup of fluid in the abdomen. Other symptoms of peritoneal mesothelioma may include bowel obstruction, blood clotting abnormalities, anemia, and fever. If the cancer has spread beyond the mesothelium to other parts of the body, symptoms may include pain, trouble swallowing, or swelling of the neck or face.
Causes
Asbestos is a known cause of peritoneal mesothelioma in humans.[1][2][3][4][5][6][7]
A 1975 study of three small villages in central Cappadocia, Turkey—Tuzköy, Karain and Sarıhıdır—found that peritoneal mesothelioma was causing 50% of all deaths. Initially, this was attributed to erionite, a zeolite mineral with similar properties to asbestos, but detailed epidemiological investigation demonstrated that the substance causes the disease mostly in families with a genetic predisposition to mineral fiber carcinogenesis. The studies are being extended to other parts of the region.[8][9]
Diagnosis
Peritoneal mesothelioma has two clinical types which can be differentiated with the help of CT findings, the "dry" type and the "wet". It is classified as "dry" when there are multiple tiny masses or one dominant localized mass and generally little or no ascites. The "wet" type has widespread small nodules, no dominant mass and a presence of ascites. If fluid is found, the process of eliminating it is through paracentesis; however the analysis of this fluid has limited diagnostic significance. Normally, a definitive diagnosis may be obtained through tissue biopsy.
Treatment
Given its rarity, there are no established guidelines for the treatment of peritoneal mesothelioma. The modern approach to malignant peritoneal mesothelioma includes cytoreductive surgery,[10] hyperthermic intraperitoneal chemotherapy (HIPEC), intraperitoneal chemotherapy, and intravenous chemotherapy.[11] These are often used in conjunction and in a complementary fashion, and this multifaceted approach has significantly improved outcomes when compared to intravenous chemotherapy alone. For instance, the reported median survival time for patients with stage IV mesothelioma as reported by the American Cancer Society is 12 months;[12] however, with adequate cytoreduction, intraperitoneal, and intravenous chemotherapy combined, some authors report 10-year survival rates projected at nearly 75%.[13]
Multiple factors have been shown to be significant in predicting the outcome and overall survival. Age greater than 60 at surgery, more overall disease burden (defined as a PCI greater than 15), complete cytoreduction (no visible disease), and epitheliod subtype pathology have all been shown to be predictors of both mortality and disease progression.[11] These known predictors notwithstanding, many patients with advanced peritoneal mesothelioma are still surgical candidates, and even patients with the highest possible score on the peritoneal carcinomatosis index (39) can be completely reduced to a PCI of 0 with adequate surgery.[14]
References
- ATSDR reference page on asbestos
- U.S. National Institutes of Health - National Cancer Institute Fact Sheet Archived 2010-09-06 at the Wayback Machine
- Consensus Report (August 1997). "Asbestos, asbestosis, and cancer: the Helsinki criteria for diagnosis and attribution". Scand J Work Environ Health. 23 (4): 311–6. PMID 9322824.
- Cai SX, Zhang CH, Zhang X, Morinaga K (April 2001). "Epidemiology of occupational asbestos-related diseases in China". Ind Health. 39 (2): 75–83. doi:10.2486/indhealth.39.75. PMID 11341561.
- Boffetta P (June 2007). "Epidemiology of peritoneal mesothelioma: a review". Ann. Oncol. 18 (6): 985–90. doi:10.1093/annonc/mdl345. PMID 17030547.
- Scripcariu V, Dajbog E, Lefter L, et al. (2006). "[Malignant peritoneal mesothelioma]". Chirurgia (Bucur) (in Romanian). 101 (6): 641–6. PMID 17283842.
- Burdorf A, Järvholm B, Siesling S (December 2007). "Asbestos Exposure and differences in occurrence of peritoneal mesothelioma between men and women across countries". Occup Environ Med. 64 (12): 839–842. doi:10.1136/oem.2006.031724. PMC 2095382. PMID 17567726.
- Dogan, Umran (2003). "Mesothelioma in Cappadocian villages". Indoor and Built Environment. Ankara: Sage. 12 (6): 367–375. doi:10.1177/1420326X03039065. ISSN 1420-326X.
- Carbone, Michelle; et al. (2007). "A mesothelioma epidemic in Cappadocia: scientific developments and unexpected social outcomes". Nature Reviews Cancer. 7 (2): 147–54. doi:10.1038/nrc2068. ISSN 1474-175X. PMID 17251920.
- "gpm cyto". www.surgicaloncology.com. Retrieved 2016-08-16.
- Magge, Deepa; Zenati, Mazen S.; Austin, Frances; Mavanur, Arun; Sathaiah, Magesh; Ramalingam, Lekshmi; Jones, Heather; Zureikat, Amer H.; Holtzman, Matthew (2014-04-01). "Malignant peritoneal mesothelioma: prognostic factors and oncologic outcome analysis". Annals of Surgical Oncology. 21 (4): 1159–1165. doi:10.1245/s10434-013-3358-y. ISSN 1534-4681. PMC 4100549. PMID 24322529.
- "Survival statistics for mesothelioma". www.cancer.org. Retrieved 2016-08-16.
- "Effect of long-term intraperitoneal chemotherapy for patients with malignant peritoneal mesothelioma on survival". Journal of Clinical Oncology. ISSN 0732-183X.
- "Current Indications". www.surgicaloncology.com. Retrieved 2016-08-16.
This article includes text from the U.S. National Cancer Institute's public domain Dictionary of Cancer Terms.
Further reading
- Bridda A, Padoan I, Mencarelli R, Frego M (2007). "Peritoneal Mesothelioma: A Review". MedGenMed. 9 (2): 32. PMC 1994863. PMID 17955087.
- Malignant mesothelioma entry in the public domain NCI Dictionary of Cancer Terms