We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
Vertebrobasilar insufficiency
From WikEM
Contents
Background
- Characterized by diminished bloodflow through the vertebral or basilar arteries. The two vertebral arteries originally branch proximally from the subcalvian artery and travel through the vertebrae and distally join to become the basilar artery. Symptoms result from diminished circulation to the posterior brain, brainstem and cerebellum. Head-turning can cause ipsilateral vertebral artery to temporarily occlude; if the contralateral vertebral artery is stenotic, this may lead to syncope. This is also known as Bow hunter's Syndrome[1]
- Head extension may also provoke symptoms. Neurologic symptoms tend to not present when one vertebral artery remains patent[2]
- Symptoms may result secondary to arterial plaques, arterial dissection, compressive lesions, or subclavian steal (see below). Posterior strokes encompass 20-30% of all strokes[3]
- Cervical ostephytes can also directly compress vertebral arteries and cause VBI symptoms[4].
Bow hunter's syndrome (Rotational vertebral artery compression)
- Head turning causes temporary occlusion of the ipsilateral vertebral artery. VBI results if the contralateral vertebral artery has a fixed occlusion[5]. Improvement of symptoms in neutral position is considered pathognomonic[6]
Subclavian steal phenomenon
A stenotic lesion in the subclavian, located proximal to the vertebral artery, results in reversing the flow of blood in the vertebral artery when superimposed with increased arm activity(4).
Clinical Features
Symptoms
- Numbness/tingling
- Vertigo/dizziness
- Changes in vision
- Nausea/vomiting
- Weakness
- Dysphagia
- Dysarthria
- Syncope
Differential Diagnosis
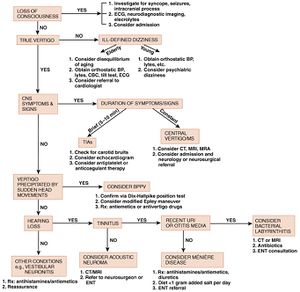
Vertigo
- Vestibular/otologic
- Benign Paroxysmal Positional Vertigo (BPPV)
- Traumatic (following head injury)
- Infection
- Meniere's disease
- Ear foreign body
- Otic barotrauma
- Neurologic
- Cerebellar stroke
- Vertebrobasilar insufficiency
- Lateral Wallenberg syndrome
- Anterior inferior cerebellar artery syndrome
- Neoplastic: cerebellopontine angle tumors
- Basal ganglion diseases
- Vertebral Artery Disssection
- Multiple sclerosis
- Infections: neurosyphilis, tuberculosis
- Epilepsy
- Migraine (basilar)
- Other
- Hematologic: anemia, polycythemia, hyperviscosity syndrome
- Toxic
- Chronic renal failure
- Metabolic
Evaluation
Work-up
- Glucose check
- Full neuro exam
- TM exam
- CTA or MRA (diagnostic study of choice) of the neck/brain if symptoms consistent with central cause
| Test | Sensitivity |
| HINTS | 100% |
| MRI (24hrs) | 68.40%[7] |
| MRI (48hrs) | 81%[7] |
| CT non con | 26%[8] |
HINTS Exam
Proposed as method of distinguishing peripheral cause from cerebellar/brain stem CVA in the Emergency Department population [9][10][11]
The 3 components of the HINTS exam include:
- Head impulse test of vestibulo-ocular reflex function
- Observation for nystagmus in primary, right, and left gaze
- Alternate cover test for skew deviation.
Head Impulse Test:
- Normally, a functional vestibular system will identify any movement of the head position and rapidly correct eye movement accordingly so that the center of the vision remains on a target. This reflex fails in peripheral causes of vertigo effective the vestibulocochlear nerve
- Have patient fix their eyes on your nose
- Move their head in the horizontal plane to the left and righ
- When the head is turned towards the normal side the vestibular ocular reflex remains intact and eyes continue to fixate on the visual target
- When the head is turned towards the affected side, the vestibular ocular reflex fails and the eyes make a corrective saccade to re-fixate on the visual target [12][13]
- It is reassuring if the reflex is abnormal (due to dysfunction of the peripheral nerve)
Test of Skew
- Skew deviation is a fairly specific predictor of brainstem involvement in patients with acute vestibular syndrome. The presence of skew may help identify stroke when a positive head impulse test falsely suggests a peripheral lesion.
- Skew is also known vertical dysconjugate gaze and is a sign of a central lesion
- Have pt look at your nose with their eyes and then cover one eye
- Then rapidly uncover the eye and quickly look to see if the eye moves to re-align.
- Repeat with on each eye
- A positive HINTS exam: 100% sensitive and 96% specific for the presence of a central lesion.
- The HINTS exam was more sensitive than general neurological signs: 100% versus 51%.
- The sensitivity of early MRI with DWI for lateral medullary or pontine stroke was lower than that of the HINTS examination (72% versus 100%, P=0.004) with comparable specificity (100% versus 96%, P=1.0).
- If any of the above 3 tests are consistent with CVA obtain full work-up (including MRI)
Management
Medical management
- Lower cholesterol
- Control hypertension
- Smoking cessation
- Antiplatelets
Surgical management
- Endarterectomy
- Bypass grafting
- Stenting
Disposition
- Admit
See Also
External Links
References
- ↑ #Go G, Hwang S-H, Park IS, Park H. Rotational Vertebral Artery Compression : Bow Hunter’s Syndrome. Journal of Korean Neurosurgical Society. 2013;54(3):243-245. doi:10.3340/jkns.2013.54.3.243.
- ↑ Ibrahim Alnaami, Muzaffer Siddiqui, and Maher Saqqur, “The Diagnosis of Vertebrobasilar Insufficiency Using Transcranial Doppler Ultrasound,” Case Reports in Medicine, vol. 2012, Article ID 894913, 3 pages, 2012. doi:10.1155/2012/894913.
- ↑ Ibrahim Alnaami, Muzaffer Siddiqui, and Maher Saqqur, “The Diagnosis of Vertebrobasilar Insufficiency Using Transcranial Doppler Ultrasound,” Case Reports in Medicine, vol. 2012, Article ID 894913, 3 pages, 2012. doi:10.1155/2012/894913.
- ↑ Tintinalli
- ↑ #Go G, Hwang S-H, Park IS, Park H. Rotational Vertebral Artery Compression : Bow Hunter’s Syndrome. Journal of Korean Neurosurgical Society. 2013;54(3):243-245. doi:10.3340/jkns.2013.54.3.243.
- ↑ #Go G, Hwang S-H, Park IS, Park H. Rotational Vertebral Artery Compression : Bow Hunter’s Syndrome. Journal of Korean Neurosurgical Society. 2013;54(3):243-245. doi:10.3340/jkns.2013.54.3.243.
- ↑ 7.0 7.1 ../docss/CNS-EBN_cat-document_2010-07-JUL-30_a-negative-dwi-mri-within-48-hours-of-stroke-symptoms-ruled-out-anterior-circulation-stroke_4494E.pdf
- ↑ Chalela JA, Kidwell CS, Nentwich LM, et al. Magnetic resonance imaging and computed tomography in emergency assessment of patients with suspected acute stroke: a prospective comparison. Lancet. 2007;369:293–8.
- ↑ ../docss/hints-exam.pdf?d13a76d516d9dec20c3d276ce028ed5089ab1ce3dae902ea1d01c0873ed8cc5fe910&c_id=2502227
- ↑ http://www.ncbi.nlm.nih.gov/pubmed/18541870
- ↑ ../docss/diff-of-vertigo.pdf?c_id=2502226&expiration=1380995436&hwt=0a8bc67ea910e018a1543ebea192f668
- ↑ Barraclough K, Bronstein A. Vertigo. BMJ. 2009;339:b3493
- ↑ Kuo CH, Pang L, Chang R. Vertigo - part 1 - assessment in general practice. Aust Fam Physician. 2008;37(5):341-7