We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
Seizure
From WikEM
(Redirected from Epilepsy)
This page covers seizures in general; refer to Status epilepticus for persistently seizing patients and seizure (peds) for pediatric patients.
Contents
Background
- Caused by a pathologic pattern of brain cortex activity → involuntary movement or change in level of consciousness[1]
- 11% of people will have at least one seizure in their lifetime
- 3% will have epilepsy (at least 2 unprovoked seizures)
- In pregnancy >20 WGA or <4wks postpartum, need to consider eclampsia
- Most seizures in pregnancy are not first-time seizures, but rather are due to medication noncompliance or pharmacokinetic drug changes as result of pregnancy
Seizure Types
Classification is based on the international classification from 1981[2]; More recent terms suggested by the ILAE (International League Against Epilepsy) task Force.[3]
Focal seizures
(Older term: partial seizures)
- Without impairment in consciousness– (AKA Simple partial seizures)
- With motor signs
- With sensory symptoms
- With autonomic symptoms or signs
- With psychic symptoms (including aura)
- With impairment in consciousness - (AKA Complex Partial Seizures--Older terms: temporal lobe or psychomotor seizures)
- Simple partial onset, followed by impairment of consciousness
- With impairment of consciousness at onset
- Focal seizures evolving to secondarily generalized seizures
- Simple partial seizures evolving to generalized seizures
- Complex partial seizures evolving to generalized seizures
- Simple partial seizures evolving to complex partial seizures evolving to generalized seizures
Generalized seizures
- Absence seizures (Older term: petit mal)
- Typical absence seizures
- Atypical absence seizures
- Myoclonic seizure
- Clonic seizures
- Tonic seizures
- Tonic–clonic seizures (Older term: grand mal)
- Atonic seizures
Clinical Features
- Abrupt onset, may be unprovoked
- Brief duration (typically <2min)
- AMS
- Jerking of limbs
- Postictal drowsiness/confusion
Seizure vs. Syncope[4]
- Factors that strongly favor seizure from most specific to least:
- Waking with cut tongue
- Abnormal behavior noted by bystanders
- LOC with emotional stress
- Postictal confusion
- Head turning to one side during LOC
- Prodromal deja vu or jamais vu
- Factors that predict against seizure
- Presyncopal spells
- Prodromal vertigo
- LOC with prolonged standing, sitting
- Diaphoresis, vertigo, nausea, chest pain, feeling of warmth, palpitations, dyspnea before spell
Differential Diagnosis
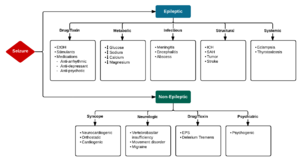
Seizure
- Epileptic seizure
- Non-epileptic seizure
- Intracranial mass
- Syncope
- Hyperventilation syndrome
- Migraine headache
- Movement disorders
- Narcolepsy/cataplexy
Evaluation
Physical
- Check for:
- Head / C-spine injuries
- Tongue/mouth lacs
- Sides of tongue (true seizure) more often bitten than tip of tongue (Psychogenic nonepileptiform seizures, formerly "pseudoseizure.")
- Tongue biting has sensitivity of ~25% and approaches 100% specificity in lateral tongue biting[5]
- Posterior shoulder dislocation
- Focal deficit (Todd paralysis vs CVA)
Work-Up
Known Epileptic with NO Change in Baseline Seizures
- Anticonvulsant drug concentration
- Fingerstick glucose
- Close out-patient follow-up
- Check for signs of trauma, cervical spine tenderness
- Consider head CT scan if suspicious of change in pattern, prolonged postictal period or trauma
New Seizure or Change in Baseline Seizures
- Consider: Pregnancy test, glucose, Electrolytes (Na, Ca, BUN, Crt), RPR, HIV, UA, EEG, lumbar puncture
- Always perform ECG as prolong QT and torsades can cause shaking after intermitent runs
- Non-contrast CT in ED or advanced imaging arranged as outpatient
- Neurology follow up or consult
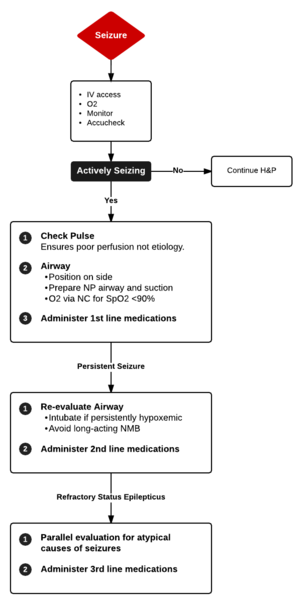
Management
- Protect patient from injury
- If possible, place patient in left lateral position to reduce risk of aspiration
- Do not place bite block!
- Benzodiazepine (Initial treatment of choice)[6]
- Secondary medications
- Fosphenytoin IV 20-30mg/kg at 150mg/min (may also be given IM)
- Contraindicated in pts w/ 2nd or 3rd degree AV block
- Valproic acid IV 20-40mg/kg at 5mg/kg/min
- Levetiracetam IV 60mg/kg, max 4500mg/dose
- Phenobarbital IV 20mg/kg at 50-75mg/min (be prepared to intubate)
- Fosphenytoin IV 20-30mg/kg at 150mg/min (may also be given IM)
- Refractory medications
- Consider
- Secondary causes of seizure (e.g. hyponatremia, hypoglycemia, INH toxicity, ecclampsia)
- Nonconvulsive seizures or status epilepticus - get EEG
Disposition
First Time Seizures
- Those with single generalized seizure and otherwise normal history and physical can be discharged home with close follow-up
- Observation is not unreasonable for those that look ill or have a complicating history/physical
- 24-hr recurrence of seizures in this group is about 9% when alcohol-related events are excluded[10]
- Instructions not to drive, swim, or participate in other potentially dangerous activities is important
See Also
- Anticonvulsants
- Anticonvulsant levels and reloading
- Seizure (peds)
- Febrile seizure
- Status epilepticus
External Links
References
- ↑ Martindale JL, Goldstein JN, Pallin DJ. Emergency department seizure epidemiology. Emerg Med Clin North Am. 2011 Feb;29(1):15-27.
- ↑ Proposal for revised clinical and electroencephalographic classification of epileptic seizures. From the Commission on Classification and Terminology of the International League Against Epilepsy. Epilepsia 1981; 22:489.
- ↑ Epilepsia 2015; 56:1515-1523.
- ↑ Sheldon R et al. Historical criteria that distinguish syncope from seizures. J Am Coll Cardiol. 2002 Jul 3;40(1):142-8.
- ↑ Benbadis SR et al. Value of tongue biting in the diagnosis of seizures. Arch Intern Med. 1995 Nov 27;155(21):2346-9.
- ↑ Glauser T, et al. Evidence-based guideline: treatment of convulsive status epilepticus in children and adults: report of the guideline committee of the American Epilepsy Society. Epilepsy Curr. 2016; 16(1):48-61.
- ↑ McMullan J, Sasson C, Pancioli A, Silbergleit R: Midazolam versus diazepam for the treatment of status epilepticus in children and young adults: A meta-analysis. Acad Emerg Med 2010; 17:575-582
- ↑ Legriel S, Oddo M, and Brophy GM. What’s new in refractory status epilepticus? Intensive Care Medicine. 2016:1-4.
- ↑ Mirsattari SM et al. Treatment of refractory status epilepticus with inhalational anesthetic agents isoflurane and desflurane. Arch Neurol. 2004 Aug;61(8):1254-9.
- ↑ Krumholz A, Wiebe S, Gronseth G, et al. Practice Parameter: evaluating an apparent unprovoked first seizure in adults (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Epilepsy Society. Neurology. 2007; 69(21):1996-2007.