We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
Nontraumatic thoracic aortic dissection
From WikEM
(Redirected from Aortic dissection)
Not to be confused with traumatic aortic transection
Contents
Background
- Most commonly seen in men 60-80 yrs old
- Intimal tear with blood leaking into media
- Mortality increases 1% per hour of symptoms when untreated
- Diagnosis delayed > 24hr in 50% of cases
- Bimodal age distribution
- Young with risk factors
- Connective tissue disease (e.g. Marfan syndrome, Ehler's-Danlos, collagen vascular disease)
- Pregnancy, especially 3rd trimester
- Chest trauma
- Recent cardiac catheterization
- Bicuspid aortic valve
- Aortic coarctation
- Elderly males with chronic hypertension
- Atherosclerotic risk factors (smoking, hypertension, HLD, DM)
- Young with risk factors
Classification (Stanford)
- Type A - Involves any portion of ascending aorta
- Requires surgery
- Type B - Isolated to descending aorta
- Primarily medical management with surgery consultation

|

|

| |
| Percentage | 60% | 10–15% | 25–30% |
| Type | DeBakey I | DeBakey II | DeBakey III |
| Stanford A (Proximal) | Stanford B (Distal) | ||
Clinical Features
General
- Symptoms
- Tearing/ripping pain (10.8x increased disease probability)
- Migrating pain (7.6x)
- Sudden chest pain (2.6x)
- History of hypertension (1.5x)
- Signs
- Focal neurologic deficit (33x)
- Diastolic heart murmur (acute aortic regurg) (4.9x)
- Pulse deficit (2.7x)
- Hypertension at time of presentation (49% of all cases[1])
- Studies
- Enlarged aorta or widened mediastinum (3.4x)
- LVH on admission ECG (3.2x)
Specific
- Ascending Aorta
- Acute aortic regurgitation, leading to a diastolic decrescendo murmur, hypotension, or heart failure, in 50%-66%
- MI/Ischemia on ECG, usually inferior
- Cardiac Tamponade
- Hemothorax - if adventitia disruption
- Horners, partial - sympathetic ganglion
- Voice hoarseness - recurrent laryngeal n. compression
- CVA/Syncope - if carotid extension
- Neurological deficits
- SBP>20mmhg difference between arms
- Hypertension at time of presentation (35.7% of all cases[1])
- Descending Aorta
- Chest pain, back pain, abdominal pain
- Chest Pain - Abrupt, severe (90% of patients) radiating to back
- Hypertension at time of presentation (70.1% of all cases[1])
- Hemiplegia, neuropathy (15%)
- Renal failure
- Distal Pulse deficits/ limb ischemia
- Mesenteric ischemia
- Chest pain, back pain, abdominal pain
Differential Diagnosis
Chest pain
Critical
- Acute Coronary Syndromes
- Aortic Dissection
- Cardiac Tamponade
- Pulmonary Embolism
- Tension Pneumothorax
- Boerhhaave's Syndrome
- Coronary Artery Dissection
Emergent
- Pericarditis
- Myocarditis
- Pneumothorax
- Mediastinitis
- Cholecystitis
- Pancreatitis
- Cocaine-associated chest pain
Nonemergent
- Stable angina
- Asthma exacerbation
- Valvular Heart Disease
- Aortic Stenosis
- Mitral valve prolapse
- Hypertrophic cardiomyopathy
- Pneumonia
- Pleuritis
- Tumor
- Pneumomediastinum
- Esophageal Spasm
- Gastroesophageal Reflux Disease (GERD)
- Peptic Ulcer Disease
- Biliary Colic
- Muscle sprain
- Rib Fracture
- Arthritis
- Chostochondirits
- Spinal Root Compression
- Thoracic outlet syndrome
- Herpes Zoster / Postherpetic Neuralgia
- Psychologic / Somatic Chest Pain
- Hyperventilation
- Panic attack
Hypertension
- Asymptomatic hypertension
- Hypertensive urgency
- Hypertensive emergency
- ACS
- Hypertensive encephalopathy
- Acute renal failure
- Nontraumatic thoracic aortic dissection
- PRES
- Preeclampsia/Eclampsia
- Autonomic dysreflexia
- Drug use or overdose (e.g stimulants or Synthroid)
- Tyramine reaction
- Pheochromocytoma
- Hyperthyroidism
- Anxiety
Evaluation
Acute Aortic Dissection (AAD) Risk Score
A score 1 should be awarded for each of the 3 categories that contain at least one of the listed features
| Predisposing conditions | Pain features | Physical findings |
|
Chest, back, or abdominal pain described as:
AND
|
|
| Score | Category | Prevalence |
| 0 | Low | 6% |
| 1 | Intermediate | 27% |
| >1 | High | 39% |
No Risk Factor Screening
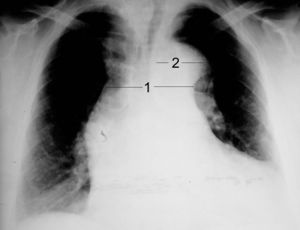
- CXR
- Abnormal in 90%
- Mediastinal widening (seen in 56-63%)
- Left sided pleural effusion (seen in 19%)
- Widening of aortic contour (seen in 48%), displaced calcification (6mm), aortic kinking, double density sign
Low AAD risk Rule-Out[2]
High Risk/Definitive
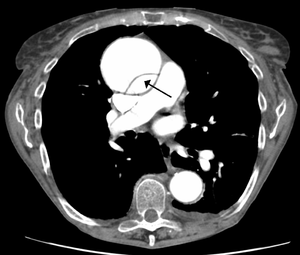
- CT aortogram chest
- Study of choice
- Similar sensitivity/specificity to TEE and MRA
Other Findings
- ECG
- Ischemia (esp inferior) - 15%
- Nonspec ST-T changes - 40%
- Bedside US
- Can help in ruling in patients when AOFT is >4cm
- Rule out pericardial effusion and tamponade
- TEE has a sensitivity of 98% and 95% specific[5]
Management
Lower wall tension by lowering BP (La Place T = P × r)
- Control heart rate before blood pressure (Goal to keep HR 60-80 and SBP 100-120)
- Important considerations
- Right radial arterial line or right arm blood pressure will be the most accurate
- Beta blockers are good first-line options, since they reduce heart rate and aortic wall tension
- However, avoid beta blockers in aortic regurgitation murmurs or on bedside echo
- Do not start nitroprusside until tachycardia resolves to avoid reflexive tachycardia
- Heart rate control (beta-blockers are first line)
- Esmolol
- Advantage of short half life, easily titratable
- Bolus 0.1-0.5mg/kg over 1min; infuse 0.025-0.2mg/kg/min
- Esmolol Drip Sheet
- Labetalol - has both alpha and beta effects
- Push dose - 10-20mg with repeat doses of 20-40mg q10min up to 300mg
- Drip - Load 15-20mg IV, followed by 5mg/hr
- Metoprolol
- 5mg IV x 3; infuse at 2-5mg/hr
- Diltiazem - Use if contraindications to beta-blockers
- Loading 0.25mg/kg over 2–5 min, followed by a drip of 5mg/h
- Esmolol
- Blood pressure control (vasodialators)
- Only use if beta-blocker is ineffective
- Do not use without a beta-blocker (must suppress reflex tachycardia - shear forces from increased HR)
- Nicardipine/Clevidipine - consider following regimen for nicardipine:
- 5mg/hr start, then titrate up by 2.5mg/hr every 10 min until goal
- Once at goal, drop to 3mg/hr and re-titrate from there
- May initially bolus 2mg IV[6]
- Nitroprusside 0.3-0.5mcg/kg/min - Risk of cerebral blood vessel vasodilation and CN/Thiocynate toxicity
- Fenoldopam
- Enalapril
- Analgesia
Disposition
- Admission to OR or ICU
Complications
- AV Regurgitation/Insufficiency
- CHF with diastolic murmur
- Rupture
- Pericardium: tamponade
- Mediastinum: hemothorax
- Vascular obstruction
- Coronary: ACS
- Carotid: CVA
- Lumbar: Paraplegia
See Also
External Links
- NNT Aortic Dissection LRs
- AHA Full Guidelines
- AHA Quick Summary
- ALiEM Paucis Verbis: International Registry on Aortic Dissection (IRAD)
References
- ↑ 1.0 1.1 1.2 Hagan PG, Nienaber CA, Isselbacher EM, et al. The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA. 2000; 283(7):897-903.
- ↑ Asha SE et al. "A systematic review and meta-analysis of D-dimer as a rule out test for suspected acute aortic dissection." Annals of EM. 66;4;368-377Ocotber 2015.
- ↑ Shimony A, et al. Meta-analysis of usefulness of d-dimer to diagnose acute aortic dissection. Am J Cardiol. 2011; 107(8):1227-1234.
- ↑ Diercks DB, et al. Clinical policy: Critical issues in the evaluation and management of adult patients with suspected acute nontraumatic thoracic aortic dissection. Ann Emerg Med. 2015; 65(1):32-42e12.
- ↑ Shiga T, Wajima Z, Apfel CC, Inoue T, Ohe Y. Diagnostic accuracy of transesophageal echocardiography, helical computed tomography, and magnetic resonance imaging for suspected thoracic aortic dissection: systematic review and meta-analysis. Arch Intern Med. 2006 Jul 10;166(13):1350-6.
- ↑ Curran MP et al. Intravenous Nicardipine. Drugs 2006; 66(13): 1755-1782. ../docss/bolus-dose-nicardipine.pdf