Chart 1: Acute, Generalized Vesicular or Pustular Rash Illness Protocol
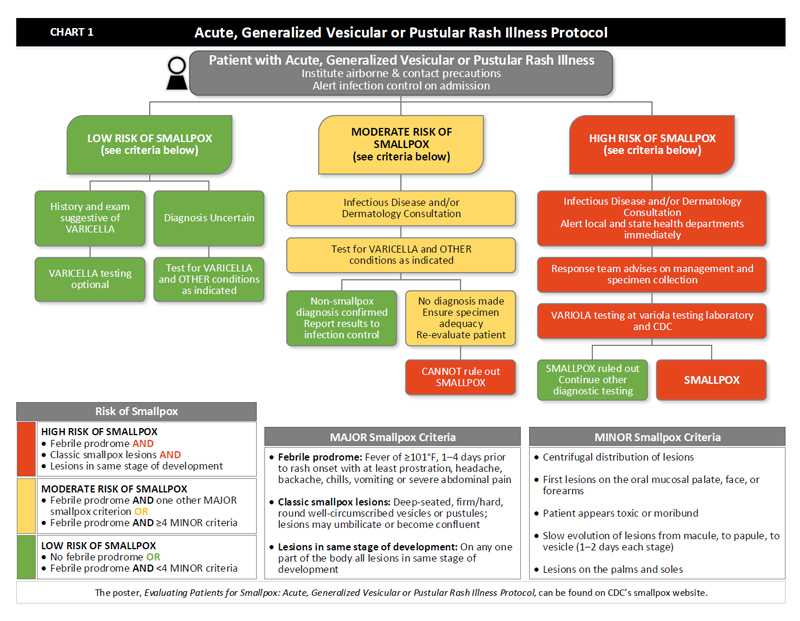
- When a patient presents with an acute, generalized vesicular or pustular rash illness, institute airborne and contact precautions. Alert infection control on admission.
- Determine the patient’s risk of smallpox using the MAJOR and MINOR criteria.
- There are three MAJOR criteria:
- Febrile prodrome: Fever of ≥101°F, 1–4 days prior to rash onset with at least prostration, headache, backache, chills, vomiting or severe abdominal pain
- Classic smallpox lesions: Deep-seated, firm/hard, round well-circumscribed vesicles or pustules; lesions may umbilicate or become confluent
- Lesions in same stage of development: On any one part of the body all lesions in same stage of development
- There are five MINOR criteria:
- Centrifugal distribution of lesions
- First lesions on the oral mucosalpalate, face, or forearms
- Patient appears toxic or moribund
- Slow evolution of lesions from macule, to papule, to vesicle (1-2 days each stage)
- Lesions on the palms and soles
- If the patient has no febrile prodrome OR has febrile prodrome AND <4 MINOR criteria, the patient’s risk of smallpox is low.
- If the patient has a history and exam suggestive of varicella, varicella testing is optional, and risk of smallpox is low.
- If the diagnosis is uncertain, test for varicella and other conditions as indicated. Risk of smallpox is low.
- If the patient has a febrile prodrome AND one other MAJOR smallpox criterion OR if the patient has a febrile prodrome AND ≥ 4 MINOR criteria, the patient’s risk of smallpox is moderate.
- Obtain Infectious Disease and/or Dermatology consultation.
- Test for Varicella and other conditions as indicated.
- If tests confirm a non-smallpox diagnosis, report results to infection control. The patient’s risk of smallpox is low.
- If no diagnosis is made after tests are completed, ensure specimen adequacy and re‑evaluate the patient. At this point, the patient’s risk of smallpox is moderate.
- If re‑evaluation does not reveal a diagnosis, you CANNOT rule out smallpox. Patient’s risk of smallpox is HIGH.
- If the patient has a febrile prodrome AND classic smallpox lesions AND lesions in the same stage of development, the patient’s risk of smallpox is HIGH.
- Obtain Infectious Disease and/or Dermatology consultation and alert local and state public health departments immediately.
- The Response team from the local and/or state public health department will advise on management and specimen collection.
- Perform variola testing at variola testing laboratory and at CDC
- If variola testing rules out smallpox, continue other diagnostic testing. Patient’s risk of smallpox is low.
- If variola is positive, then smallpox is confirmed.
- There are three MAJOR criteria:
- Page last reviewed: December 1, 2016
- Page last updated: December 1, 2016
- Content source:


 ShareCompartir
ShareCompartir