Whole Genome Sequencing (WGS)
Whole genome sequencing (WGS) provides detailed genetic information about germs that make people sick. CDC’s Division of Foodborne, Waterborne, and Environmental Diseases uses this information to improve efforts to find, investigate, and prevent illnesses caused by bacteria, fungi and parasites. These capabilities are especially important when looking for the source of an outbreak or trying to predict antibiotic resistance in bacteria. WGS provides highly detailed and timely information that helps CDC and other government agencies protect the public’s health.
What It Does
Making the Match
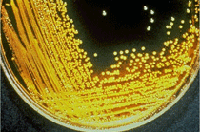
Like people, germs have DNA. WGS allows scientists to study these germs by looking at their DNA fingerprints. It also lets them compare different fingerprints of germs to one another. By comparing the whole genome sequences of these germs, scientists can determine if they are closely related to one another (or are very similar), which indicates those germs likely came from the same source.

Since 2013, WGS has allowed scientists to detect more Listeria outbreaks, solve them while they are still small, and identify new food sources of Listeria, such as caramel apples and ice cream.
Read more about how WGS helped make the match in a Listeria outbreak.
Imagine someone giving you two books to compare, using different methods. With the first method, you can see whether both books have the same number of chapters. With the second method, you can tell whether almost every letter of every word in both books is the same. Whole genome sequencing is like the second method and provides much more detail about germs compared with traditional laboratory methods.
WGS provides a nearly complete reading of the millions of units that make up a germ’s DNA. By knowing what order these units are in, scientists can identify the type of germ and learn more about its genes, including, in bacteria, the genes that cause antibiotic resistance. This detailed information also allows outbreak investigators to link cases of illness in an outbreak and find sources of infection with greater confidence than with other DNA fingerprinting methods. Before WGS, scientists still used DNA fingerprints from germs to link illnesses, but those fingerprints contained less information.
Foodborne Outbreak Investigations
The results from WGS help CDC precisely identify the germ responsible for foodborne disease outbreaks. Outbreak investigators combine WGS data with information from sick people about what they ate to:
- Link cases: By comparing the DNA fingerprints of bacteria taken from sick people, scientists can determine if they are closely related to one another or are very similar. If so, this close genetic relationship provides more evidence that people got sick from the same source.
- Find the source: Scientists from CDC, the U.S. Food and Drug Administration, the U.S. Department of Agriculture’s Food Safety and Inspection Service, and state health departments analyze bacteria taken from potential sources. If bacteria found in a food or food production environment have genome sequences similar to bacteria from sick people, investigators are more confident that people got sick from that food.
These data also help shape government food safety policies and food industry practices, which help to make food safer and save lives. Federal agencies use whole genome sequencing to detect and investigate foodborne disease outbreaks through two networks:
- PulseNet, a laboratory network managed by CDC, focuses on bacteria from sick people.
- GenomeTrakr, a database of foodborne germs managed by FDA, focuses on germs from contaminated food products and the environment.
Beyond Foodborne Outbreaks
Scientists regularly analyze samples of germs collected from sick people to better understand how diseases are spread around the world, to discover trends in disease transmission and to uncover new or unknown sources of infections. Some sequencing activities are:
- Tracking U.S. Candida auris cases, helping investigators determine how this multidrug-resistant fungus is being spread in U.S. healthcare facilities and around the world.
- Investigating the expanding geographic range of Valley fever, which helped researchers detect where the fungus was present in a new part of the country.
- Using CryptoNet to identify and compare whole-genome profiles of the parasite Cryptosporidium (“Crypto”) to support investigations of Crypto outbreaks, increase understanding of Crypto transmission, and improve prevention strategies.
Success Stories

Learn how CDC is using WGS to transform illness detection, investigation, and prevention.
The information from WGS helped CDC scientists create CryptoNet, a new DNA fingerprinting system for Cryptosporidium, a waterborne parasite that can get into our drinking water and swimming pools.
More information about CryptoNet
In 2010, a cholera outbreak sickened more than 250,000 and caused 4,000 deaths in Haiti 9 months after a massive earthquake. WGS linked all of the tested cholera and indicated that United Nations peacekeepers brought the disease into the country.
Antibiotic Resistance
WGS can tell us if bacteria have genes that may predict whether they are resistant to antibiotics. When bacteria are resistant to certain antibiotics, those drugs can no longer be used to fight infections. Using WGS, researchers can better understand how bacteria become resistant to antibiotics and how resistance spreads. This information helps scientists find ways to stop the spread of antibiotic-resistant infections. Learn more about how CDC’s National Antimicrobial Resistance Monitoring System is using WGS to study antibiotic resistance.
The Future of WGS
State public health laboratories are quickly expanding their use of WGS. CDC’s PulseNet laboratory is moving toward using WGS as the sole DNA fingerprinting technology for foodborne bacteria, making the continued collection and submission of specimens very important. PulseNet is supporting a nationwide switch to WGS that includes training public health microbiologists to perform sequencing, purchasing sequencing supplies, and updating systems for data analysis. These efforts ensure CDC and its public health partners can continue to successfully detect, respond, and stop infectious diseases.
- Page last reviewed: September 27, 2017
- Page last updated: September 27, 2017
- Content source:


 ShareCompartir
ShareCompartir