Division Accomplishments
The Division of Foodborne, Waterborne, and Environmental Diseases protects public health nationally and internationally through the prevention and control of disease, disability, and death caused by foodborne, waterborne, and environmentally transmitted infections.
Food
Detecting, investigating, and monitoring foodborne and diarrheal disease outbreaks

CDC staff collect samples while investigating an E. coli O157 outbreak linked to a Connecticut dairy goat farm in 2016.
- In 2016, CDC investigated more than 200 multistate clusters of foodborne illness. CDC worked with FDA, USDA, and state health and regulatory partners to identify the source of these outbreaks.
- In addition to foodborne outbreaks, CDC investigated several multistate outbreaks caused by bacteria that were spread by direct or indirect contact with animals.
- Expanded state health department capacity to interview ill people to determine what they ate that made them sick, resulting in better, faster data and improving our nation’s ability to solve foodborne disease outbreaks.
- Created a sixth Integrated Food Safety Center of Excellence to provide assistance and training to other state and local health departments to build their capacity to track and investigate foodborne disease.
Understanding and tracking foodborne pathogens and infections
- Developed a method to estimate how many antibiotic- resistant Salmonella infections occur in people every year. These estimates help track progress to combat antibiotic-resistant bacteria and provide information to shape prevention efforts.
- Responded to the emergence in the United States of strains carrying mcr-1, a gene that can make bacteria resistant to colistin, a last-resort antibiotic for some multidrug-resistant infections.
- Enhanced public access to surveillance data through new online public databases, FoodNet Fast and NARMS Now.
- Fully integrated the System for Enteric Disease Response, Investigation, and Coordination (SEDRIC) as a routine tool for foodborne and animal-related outbreak surveillance and response across the country. SEDRIC is a web-based tool that helps outbreak investigators at the local, state, and federal levels share data in real time to solve outbreaks faster and prevent illnesses and deaths.
- Published new information about listeriosis in scientific journals that explained the role of whole genome sequencing (WGS) in outbreak investigation, demonstrated the ability of WGS paired with epidemiologic data to link one case to lettuce, and determined the incubation period of the disease.
Water
Making water safer, in the United States and around the world, through water, sanitation and hygiene (WASH) expertise
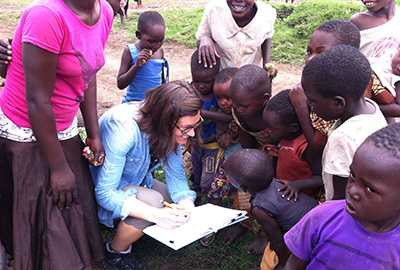
Epidemic Intelligence Service Officer Karlyn Beer greets children in a northern Tanzania village during a cholera outbreak rapid response.
- Assisted clinicians and tested more than 150 clinical samples from around the country for free-living amebas, such as Naegleria fowleri.
- Launched One Health Harmful Algal Bloom System, a national tracking system for harmful algal blooms and related illnesses in humans and animals. These blooms occur when certain types of microscopic algae grow quickly in water and may harm the health of people and animals, and the environment.
- Assembled a new team to attack multidrug-resistant shigellosis.
- Supported efforts to track, control and prevent epidemic cholera in East and West Africa. Before it was controlled, a cholera epidemic in Tanzania had caused 25,139 illness and 390 deaths.
Fungal
Preventing and controlling fungal infections in the United States and around the globe

Strain of Candida auris cultured in a petri dish.
- Identified, investigated, and developed prevention recommendations for infections with Candida auris, a globally emerging drug-resistant fungus.
- Provided epidemiologic, environmental, and laboratory assistance for fungal disease outbreak investigations, including Exophiala bloodstream infections, Malassezia infections, and histoplasmosis.
- Supported cryptococcal disease prevention activities, including evaluating screening programs, building laboratory capacity, and promoting access to laboratory testing and antifungal medicines. This included scaling up a new, cost-effective Cryptococcus screen-and-treat program in South Africa that can save the lives of over 400,000 HIV/AIDS patients.
- Tracked trends in antifungal resistance in Candida and the epidemiology of candidemia, one of the most common healthcare-associated bloodstream infections in the United States. Data and isolates have been collected for over 6,500 people since 2008.
Laboratory
Building capacity for whole genome sequencing and addressing the challenges of rapid diagnostic tests.

In Dubai, CDC trained public health laboratory staff on methods used for foodborne outbreak detection in PulseNet International.
- Expanded whole genome sequencing for public health surveillance in states across the country, making the detailed DNA fingerprinting technology part of daily food safety microbiology for public health. At the close of 2016, labs in 30 states were certified to use whole genome sequencing and report to CDC.
- Worked to develop short- and long-term solutions to preserve the samples of patients’ bacteria (bacterial cultures, or isolates) needed to obtain the DNA fingerprints needed to detect foodborne disease outbreaks and monitor antibiotic resistance trends.
- Promoted performing a bacterial culture at clinical and state public health laboratories to confirm positive results from rapid tests that do not rely on bacterial cultures (culture-independent diagnostic test).
- Identified bacterial genetic targets that could be used for routine surveillance that would test directly from primary samples such as stool and blood.
- Worked with culture-independent diagnostic test manufacturers to encourage test designs that will allow culturing bacteria from positive samples.
- Applied new laboratory tools to detect Coccidioides in the environment and used whole genome sequencing to understand the emergence of this fungus that causes Valley Fever in new geographic areas.
- Performed laboratory surveillance for azole-resistant Aspergillus fumigatus and initiated a pilot program for surveillance of invasive mold infections.
- Analyzed DNA profiles of over 200 Cryptosporidium samples to develop a new DNA fingerprinting and classification system to identify different Cryptosporidium species.
- Developed the first whole genome sequence-based method of bacterial identification to receive approval for CLIA-certified reporting at the CDC.
Global
Building capacity in partner countries to support their efforts in preventing, detecting, and responding to foodborne, waterborne, and mycotic disease outbreaks.

CDC arranged a cholera laboratory methods training for the Centre Pasteur Cameroon at Laquintinie Regional Hospital in Cameroon. Trainers included CDC’s MaryAnn Turnsek, second from right, first row.
- Developed a training toolkit to build and sustain public health capacity to prevent, detect, and respond to outbreaks caused by contaminated food and water.
- Designated as a WHO Collaborating Centre for Antimicrobial Resistance for surveillance for foodborne infections and fungi.
- Provided laboratory and epidemiological trainings in Cameroon, Georgia, Indonesia, Kenya, Mexico, and Uganda. These capacity building activities help CDC protect and control outbreaks at their source, saving lives and reducing costs.
- Continued efforts to limit and control cholera around the world, from Haiti to Tanzania, including new guidance for a cholera vaccine for travelers accepted by the Advisory Committee on Immunization Practices.
Communications and Partnerships

Download infographic [PDF – 1 page], which explains key tools and tips to help prevent food poisoning.
- Awarded $30 million to states and cities through the Epidemiology and Laboratory Capacity Cooperative Agreement to support foodborne disease prevention and tracking.
- Promoted food safety education through CDC features, FoodSafety.gov, partnerships with consumer food safety education groups, and media and social media outreach.
- Increased targeted outreach to food and animal industries through infographics, fact sheets, and presentations providing insight on how outbreaks are investigated.
Related Links
-
Learn about 2016 accomplishments from CDC’s National Center for Emerging and Zoonotic Infectious Diseases.
- Page last reviewed: April 28, 2017
- Page last updated: April 28, 2017
- Content source:


 ShareCompartir
ShareCompartir