This page is a historical archive and is no longer maintained.
For current information, please visit http://www.cdc.gov/media/
Fact Sheet
For Immediate Release: April 7, 2011
Contact: CDC Online Newsroom
(404) 639-3286
World Health Day: Media Fact Sheet
Antimicrobial resistance: no action today, no cure tomorrow
On this Page
- Antimicrobial resistance in U.S. healthcare and community settings
- Antiviral Resistance and HIV
- Antiviral Resistance and Influenza
- Antimicrobial resistance and Malaria
- Antimicrobial resistance and Neisseria gonorrhoeae
- Antimicrobial resistance and Tuberculosis (TB)
Download a PDF version of this fact sheet ( 448 KB)
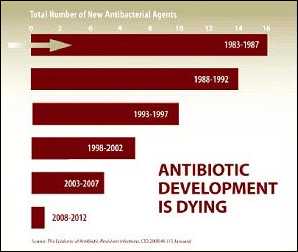
Antimicrobial resistance—when germs change in a way that reduces or eliminates the effectiveness of drugs to treat them—is a growing global problem. Antimicrobial treatments, which include antibiotics, antivirals, antifungals, and other medications, are some of the most important tools we have to combat life‐threatening diseases.
Inappropriate antimicrobial use drives resistance – harms patients
All use of antimicrobials in inpatient and outpatient settings drives antibiotic resistance and increases one's chance of acquiring an antimicrobial-resistant infection. Therefore, it is important to use antibiotics only when needed. Antimicrobial or drug resistance is compromising the effectiveness of these important treatments and increases the patient's risk of complications or death. Patients, healthcare providers, hospital administrators, industry, and policy makers must work together to employ effective strategies for improving antimicrobial use – ultimately saving lives.
Antimicrobial resistance in U.S. healthcare and community settings
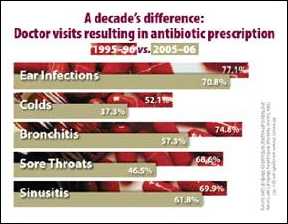
Scope of the problem: It is estimated that approximately 50% of antimicrobials, particularly antibiotics, are unnecessarily or inappropriately prescribed in U.S. hospitals and doctors' offices. Reducing unnecessary antibiotic use can decrease resistance, Clostridium difficile infections, costs, and improve patient outcomes. Drug resistance found in healthcare facilities can include organisms like methicillin-resistant Staphylcoccus aureus and Gram-negative infections such as carbapenem-resistant Enterobacteriaceae (CRE) such as Klebsiella pneumoniae carbapenemase (KPCs). In the community, resistant bacteria that cause pneumococcal disease (ranging from ear and sinus infections to pneumonia and meningitis) can pose serious challenges. In 2009, an estimated 34% of cases of invasive pneumococcal disease in the United States were not susceptible to at least one antibiotic, and 16% were not susceptible to at least 3 antibiotics. When treatment options are not available for pneumococcal disease, illnesses can last longer or even be fatal.
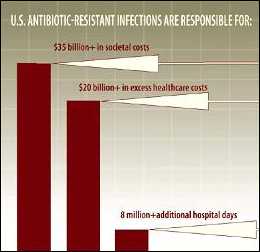
Impact of the problem: Antibiotic resistance increases the economic burden on the entire healthcare system since resistant infections cost more to treat and can prolong healthcare use. More than $1.1 billion is spent annually in the U.S. on unnecessary antibiotic prescriptions for respiratory infections in adults. In children, antibiotics are the most common cause of emergency department visits for adverse drug events. U.S. antibiotic-resistant infections are responsible for $20 billion in excess healthcare costs, $35 billion in societal costs, and 8 million additional hospital days.
How to prevent resistance: The presence of antibiotic-resistant bacteria is greatest during the month following a patient's antibiotic use and may persist for up to 12 months. Patients can help prevent antibiotic resistance by practicing appropriate antibiotic use and preventing infections – through good hygiene and receiving recommended vaccines. In addition to programs that prevent infections, healthcare providers can improve antimicrobial use by putting stewardship interventions into practice in their facilities. These interventions can be implemented in any healthcare setting and have been shown to improve patient outcomes, reduce antimicrobial resistance, and save money.
What CDC is doing about it: Promoting appropriate antibiotic use in community and healthcare settings is one strategy to combat antibiotic resistance. CDC's Get Smart: Know When Antibiotics Work and Get Smart for Healthcare programs address this strategy through a variety of tactics. CDC will continue to support World Health Organization policy through promotion of standard treatment guidelines, adherence to treatment, and treatment health literacy. CDC works with state health departments, professional organizations, and other partners to tackle the spread of drug-resistant infections in healthcare facilities through the prevention of healthcare-associated infections. [More information…]
 Antiviral Resistance and HIV
Antiviral Resistance and HIV
Scope of the problem: Antiretroviral therapy (ART) has substantially slowed disease progression and improved the quality of the lives of persons infected with HIV. Published studies estimate that 4 to 20% of persons newly diagnosed with HIV infection have transmitted drug resistance, with the highest prevalence occurring in countries with long-established ART. In the United States, HIV drug-resistance surveillance at 11 HIV surveillance sites in 2007 found that one of every six newly diagnosed HIV infections in 2007 was drug-resistant. Of these, 2.2% were resistant to two or more classes of drugs used to treat HIV.
Impact of the problem: The emergence of drug-resistant HIV strains hinders ART response and limits treatment options in affected individuals. Widespread ART use has resulted in the development of drug-resistant HIV strains that can be transmitted and can compromise the effectiveness of first-line treatment regimens among drug-naïve individuals. Alternate regimens can be more costly and make adherence more difficult. Drug resistance continues to be an important limitation to successful HIV therapy and prevention.
How to prevent resistance: Because of the high genetic variability and rapid mutation rate of HIV, the development of some drug-resistant HIV strains is inevitable. Nonetheless, healthcare providers can help minimize drug resistance by testing for drug resistance at diagnosis, before treatment initiation, and upon treatment failure and by considering drug resistance when determining ART regimens for their patients. Individuals who are on ART can also prevent drug resistance by taking their medications as prescribed and by engaging in practices and behaviors that reduce transmission to others.
What CDC is doing about it: At 11 state and local health departments, CDC maintains the Variant, Atypical, and Resistant HIV Surveillance System (VARHS) as a part of the national HIV surveillance system. The purpose of VARHS is to estimate the prevalence of transmitted drug resistance mutations in individuals newly diagnosed with HIV and to monitor the distribution of HIV subtypes in the United States. Data obtained and analyzed from VARHS are used to assist local HIV prevention and treatment program planning and evaluation. In addition, CDC funds programs to assist persons living with HIV to implement HIV prevention strategies, maintain healthy lifestyles, and to improve adherence to treatment regimens.
Antiviral Resistance and Influenza
Scope of the problem: Of the four licensed prescription influenza antiviral agents (amantadine, rimantadine, oseltamivir, zanamivir) that are available in the United States, high levels of resistance to the adamantanes (amandatine, rimantadine) persist among 2009 influenza A (H1N1) and influenza A (H3N2) viruses circulating globally.
Impact of the problem: Resistance of influenza A viruses to antiviral drugs can occur spontaneously or emerge rapidly during the course of antiviral treatment. During the past five years, the emergence of resistance to one or more of the four licensed influenza antiviral agents among some circulating influenza virus strains has complicated influenza treatment and chemoprophylaxis recommendations.
How to prevent resistance: Annual influenza vaccination is the best way to prevent influenza. Antiviral medications should be used as adjuncts to vaccination, not as a substitute for vaccination when vaccine is available. Indiscriminate use of influenza antiviral chemoprophylaxis might promote drug resistance. Infection control measures are especially important for patients who are immunocompromised to reduce the risk of transmission of antiviral drug-resistant influenza virus.
What CDC is doing about it: CDC conducts ongoing surveillance and testing of influenza viruses to monitor for antiviral resistance in collaboration with state public health departments and the World Health Organization. The information collected is used to make informed public health policy recommendations about the use of influenza antiviral medications. CDC continually improves the ability to detect rapidly and to monitor antiviral resistance through improvements in laboratory methods and by increasing the number of surveillance sites domestically and globally.
 Antimicrobial resistance and Malaria
Antimicrobial resistance and Malaria
Scope of the problem: Plasmodium falciparum, the most dangerous of the malaria parasites, is able to develop resistance to drugs more rapidly than other forms of malaria and began to develop resistance to chloroquine in the late 1950s. Chloroquine resistance has spread to nearly all areas of the world where falciparum malaria is transmitted. In some areas, this form of malaria can only be treated with artemisinin-based combination treatments, because resistance has developed to all of the other currently available antimalarial drugs. Most recently, artemisinin resistance appears to be emerging in parts of Southeast Asia.
Impact of the problem: Worldwide, malaria caused 780,000 deaths in 2009, and there were an estimated 225 million cases. Most (90%) of the deaths are in children in Africa. Important advances in malaria control have been made in the past 10 years. However, the development of resistance to antimalarial drugs poses one of the greatest threats to malaria control and results in increased malaria morbidity and mortality.
How to prevent resistance: Discourage the use of single drug artemisinin therapies, limit use of artemisinin combination treatments to confirmed malaria cases, and reduce malaria transmission by ensuring that people in malaria-endemic areas sleep under insecticide-treated bed nets and/or have their houses sprayed with insecticide.
What CDC is doing about it: CDC jointly implements the President's Malaria Initiative (PMI) in 17 countries in sub-Saharan Africa and in the Mekong Subregion, leading PMI's monitoring and evaluation efforts and providing technical assistance in other areas as well. It also provides technical assistance to the Amazon Malaria Initiative. CDC conducts ongoing investigations into the genetic complexity of malaria parasites and how this complexity affects drug resistance, immunity, and disease. [More information…]
Antimicrobial resistance and Neisseria gonorrhoeae
Scope of the problem: Gonorrhea, caused by a bacterium called Neisseria gonorrhoeae, is the second most common, reportable, communicable disease in the U.S. with 301,174 cases reported to CDC in 2009. However, CDC estimates that more than 700,000 persons in the U.S. become infected with gonorrhea each year. Gonorrhea has acquired resistance to the antibiotics used for the treatment of the disease, with 23.5% of strains in 2009 showing resistance to penicillin, tetracycline, fluoroquinolones, or a combination of these antibiotics. Preliminary 2010 data indicate that the potential for cephalosporin-resistant gonorrhea is now increasing.
Impact of the problem: Cephalosporins are the only class of antibiotics left as the recommended treatment of gonorrhea in the U.S. If cephalosporin-resistant gonorrhea emerges in the U.S., our ability to treat this common infection will be significantly compromised and result in costly complications.
How to prevent resistance: With the possible emergence of cephalosporin-resistant gonorrhea in the U.S., all antibiotic treatment options have been exhausted; thus dual therapy (with cephalosporins and either azithromycin or doxycycline) is one theoretical approach to prevent emerging resistance to cephalosporins. In addition, decreasing the burden of gonorrhea overall through health promotion, condom use, screening, and timely treatment of patients and their partners is important.
What CDC is doing about it: CDC's Gonococcal Isolate Surveillance Project (a collaborative project between CDC, select STD clinics, and five regional laboratories) monitors potential resistance of gonorrhea to antibiotics. A multi-drug resistant gonococcal outbreak response plan was developed to identify additional resistant gonorrhea cases through enhanced surveillance and partner services to ensure timely and appropriate treatment of resistant cases. CDC is working with the National Institutes of Health to identify other drugs which can be used to treat gonorrhea cost-effectively if cephalopsorins are no longer an option. Globally, CDC is working with the World Health Organization to address multi-drug resistant gonorrhea infections. [More information…]
 Antimicrobial resistance and Tuberculosis (TB)
Antimicrobial resistance and Tuberculosis (TB)
Scope of the problem: Tuberculosis (or TB) is caused by a bacterium called Mycobacterium tuberculosis. Globally, in 2008, there were an estimated 440,000 cases of multidrug-resistant TB (MDR TB), mostly in China, India, the Russian Federation, and South Africa. By July 2010, a total of 58 countries and territories had reported at least one case of extensively drug-resistant TB (XDR TB). In the U.S., approximately 1.3% of all TB cases reported in 2009 were MDR TB (113 total cases). One case of extensively drug-resistant TB (XDR TB) has been reported to-date.
Impact of the problem: Drug resistance poses a serious threat to our ability to treat and to control TB, both in the U.S. and abroad. Persons with drug-resistant TB are more likely to progress to—and die of—TB disease than persons with drug-susceptible TB. Drug-resistant TB is extremely difficult and costly to treat. It is estimated that preventing a single case of MDR TB could save the U.S. healthcare system more than $250,000, and the cost of hospitalization for one XDR TB patient is estimated to average $483,000.
How to prevent resistance: Healthcare providers can help prevent drug-resistant TB by quickly diagnosing cases, following recommended treatment guidelines, monitoring patients' response to treatment, and making sure therapy is completed. The most important thing people can do to prevent the spread of drug-resistant TB is to take all of their medications exactly as prescribed by their healthcare provider.
What CDC is doing about it: CDC collaborates with state, federal, and international partners to raise awareness and enhance strategies for TB prevention worldwide by strengthening TB services for people living with HIV/AIDS; assembling outbreak response teams; improving access to TB drugs; developing international TB testing standards; building capacity of healthcare providers to diagnose and to treat TB; convening the Federal TB Task Force; providing technical assistance to expand TB program capacity; promoting effective infection control measures; and supporting TB communication and education efforts. [More information…]
###
U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES
- Historical Document: April 7, 2011
- Content source: Office of the Associate Director for Communication, Division of News and Electronic Media
- Notice: Links to non-governmental sites do not necessarily represent the views of the CDC.
View Press Releases in
Contact Us:
- Centers for Disease Control and Prevention
1600 Clifton Rd
Atlanta, GA 30333 - 800-CDC-INFO
(800-232-4636)
TTY: (888) 232-6348 - Contact CDC-INFO

