Medical Screening of U.S.-Bound Refugees
Central American Refugee Health Profile
Overseas Medical Examination
An overseas medical examination is mandatory for all refugees identified for resettlement to the United States and must be performed in accordance with CDC’s Technical Instructions. The overseas medical examination is performed by panel physicians selected by the U.S. Department of State. CDC provides the regulatory and technical oversight and training for all panel physicians. The purpose of the medical examination is to identify applicants with inadmissible health-related conditions.
Central American refugees and parolees admitted through the CAM program receive medical assessments from panel physicians before arrival in the United States (Figure 3). As this program is relatively new, additional components of the medical screening may be added as more individuals are approved for resettlement. Those entering under different mechanisms do not receive medical assessments by panel physicians before entry.
Information collected during the overseas medical examination is reported to the Electronic Disease Notification system (EDN) and is available to state refugee health programs in the states where the refugees are resettled. Refugees are not required to receive any vaccines before they are admitted into the United States.
Figure 3: Medical Assessment of United States-bound Central American Refugees
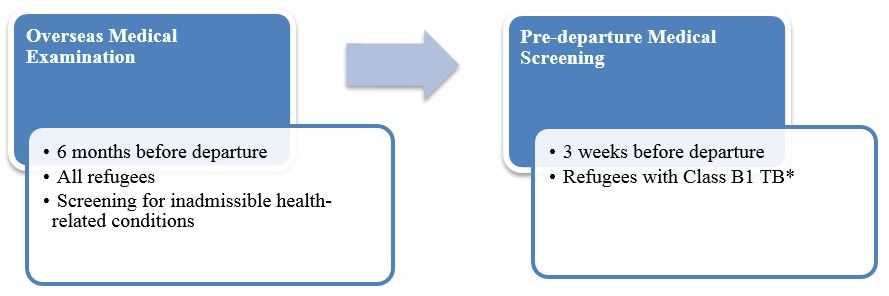
* Class B1 TB refers to tuberculosis fully treated by directly observed therapy, or abnormal chest x-ray with negative sputum smears and cultures, or extrapulmonary TB.
Pre-departure Medical Screening
If previously diagnosed with Class B1 TB (tuberculosis fully treated using directly observed therapy, or abnormal chest x-ray with negative sputum smears and cultures, or extrapulmonary TB), Central American refugees receive a pre-departure medical screening approximately 3 weeks before leaving for the United States.
Post-Arrival Medical Screening
CDC recommends that refugees receive a post-arrival medical screening (domestic medical examination) within 30 days of arrival in the United States. The Department of Health and Human Services’ Office of Refugee Resettlement (ORR) supports medical screening for those who have been granted refugee status. The purpose of these comprehensive examinations is to identify conditions for which refugees may not have been screened during their overseas medical examinations and to introduce refugees to the U.S. healthcare system. CDC provides guidelines and recommendations for the domestic medical examination of newly arrived refugees, which state health departments oversee and administer. State refugee health programs determine who conducts the examinations within their jurisdictions; these may be performed by health department personnel, private physicians, or federally qualified health centers (FQHCs). Most state health departments collect data from the screenings.
References
-
Cultural Orientation Resource Exchange, Backgrounder: Central American Minors. 2015.
-
Central Intelligence Agency. Guatemala. The World Factbook [cited 2015 March];
Available from: https://www.cia.gov/library/publications/the-world-factbook/geos/gt.html. -
Central Intelligence Agency. El Salvador. The World Factbook [cited 2015 March];
Available from: https://www.cia.gov/library/publications/the-world-factbook/geos/es.html. -
Central Intelligence Agency. Honduras. The World Factbook [cited 2015 March];
Available from: https://www.cia.gov/library/publications/the-world-factbook/geos/ho.html. -
United States Department of State, Guatemala, in International Religious Freedom Report for 2012. 2012.
-
Stansifer, C.L., Guatemala, in Encyclopaedia Britannica. 2015.
-
Moncada R, J., W. Clegern, and R. Woodward, Honduras, in Encyclopaedia Britannica. 2014.
-
Zimmerman, L., Women in Latin America. Roger Thayer Stone Ceter for Latin American Studies, Tulane University.
-
U.S. Customs and Border Protection. Southwest Border Unaccompanied Alien Children Statistics FY 2015. 2015 [cited 2015 November];
Available from: http://www.cbp.gov/newsroom/stats/southwest-border-unaccompanied-children/fy-2015. -
Centers for Disease Control and Prevention, Unaccompanied Children: Health Information for Public Health Partners.
-
Langlois, J., Written testimony of USCIS Refugee, Asylum and International Operations Associate Director Joseph Langlois for a Senate Committee on the Judiciary, Subcommittee on Immigration and The National Interest hearing titled “Eroding the Law and Diverting Taxpayer Resources: An Examination of the Administration's Central American Minors Refugee/Parole Program”. 2015.
-
Article 1, Convention Relating to the Status of Refugees, Editor. 1951.
-
U.S. Citizenship and Immigration Services. Humanitarian Parole. 2015 [cited 2015 November];
Available from: http://www.uscis.gov/humanitarian/humanitarian-parole. -
Central Intelligence Agency. Physicians density. [cited 2016 March 17];
Available from: https://www.cia.gov/library/publications/the-world-factbook/fields/2226.html. -
World Health Organization, Health workforce, infrastructure, essential medicines. 2009.
-
World Bank, Universal Healthcare on the rise in Latin America. 2013.
-
Pan American Health Organization, Health Systems Profile: Honduras, in Monitoring and Analyzing Health Systems Change/Reform. 2009.
-
Brown, S. Considering Curanderismo: the place of traditional Hispanic folk healing in modern medicine. 2008 [cited 2016 September];
Available from: http://www.bc.edu/clubs/mendel/ethos/archives/2008/brown.shtml. -
UNICEF, Country statistics 2015.
-
The World Bank, HealthStats 2016.
-
UNICEF. At a glance: Guatemala. 2013 [cited 2015 November]; Available from: http://www.unicef.org/infobycountry/guatemala_statistics.html.
-
Geneva Declaration Secretariat, Global Burden of Armed Violence 2011: Lethal Encounters. 2011, Cambridge University Press: Cambridge.
-
United Nations High Commissioner for Refugees, Women on the Run: First-hand accounts of refugees fleeing El Salvador, Guatemala, Honduras, and Mexico. 2015.
-
Manjoo, R., Special Rapporteur on violence against women finalizes country mission to Honduras and calls for urgent action to address the culture of impunity for crimes against women and girls. 2014, United Nations Human Rights, Office of the High Commissioner.
-
Marilena Adams, T., Chronic violence and non-conventional armed actors: a systematic approach. 2014.
-
Bakrania, S., Organised violence and its impacts in Central America's northern triangle. 2013, GSDRC Applied Knowledge Services.
-
American Academy of Pediatrics. Immigrant Toolkit. [cited 2015 December]; Available from: https://www.aap.org/en-us/about-the-aap/Committees-Councils-Sections/Council-on-Community-Pediatrics/Pages/Section-1-Clinical-Care.aspx.
-
Pan American Health Organization and World Health Organization, Chikungunya and dengue fever in the Americas, in Epidemiological Alert. 29 August 2014.
-
Centers for Disease Control and Prevention. Chikungunya Virus. 2016 [cited 2016 March 11]; Available from: http://www.cdc.gov/chikungunya/index.html.
-
Centers for Disease Control and Prevention. All Countries & Territories with Active Zika Virus Transmission. 2016 [cited 2016 December];
Available from: https://www.cdc.gov/zika/geo/active-countries.html. -
Gatherer, D. and A. Kohl, Zika virus: a previously slow pandemic spreads rapidly through the Americas. J Gen Virol, 2016. 97(2): p. 269-73.
-
European Centre for Disease Prevention and Control, Rapid risk assessment: Zika virus epidemic in the Americas: potential association with microcephaly and Guillain-Barré syndrome. 2015, ECDC: Stockholm.
-
World Health Organization. Tuberculosis profile: El Salvador. 2015 [cited 2015 November];
Available from: https://extranet.who.int/sree/Reports?op=Replet&name=%2FWHO_HQ_Reports%2FG2%2FPROD%2FEXT%2FTBCountryProfile&ISO2=SV&LAN=EN&outtype=html. -
World Health Organization. Tuberculosis profile: Guatemala. 2015 [cited 2015 November];
Available from: https://extranet.who.int/sree/Reports?op=Replet&name=%2FWHO_HQ_Reports%2FG2%2FPROD%2FEXT%2FTBCountryProfile&ISO2=GT&LAN=EN&outtype=html. -
World Health Organization. Tuberculosis profile: Honduras. 2015 [cited 2015 November];
Available from: https://extranet.who.int/sree/Reports?op=Replet&name=%2FWHO_HQ_Reports%2FG2%2FPROD%2FEXT%2FTBCountryProfile&ISO2=HN&LAN=EN&outtype=html. -
Calvo, F.N., et al, Reunión de la Comisión Intergubernamental de la Iniciativa de los Países de Centroamérica (IPCA) para la Interrupción de la Transmisión Vectorial, Transfusional y Atención Médica de la Enfermedad de Chagas.
-
Bern, C., et al., Trypanosoma cruzi and Chagas' Disease in the United States. Clin Microbiol Rev, 2011. 24(4): p. 655-81.
-
Bern, C., Chagas' Disease. N Engl J Med, 2015. 373(19): p. 1882.
-
Hotez, P.J., L. Woc-Colburn, and M.E. Bottazzi, Neglected tropical diseases in Central America and Panama: review of their prevalence, populations at risk and impact on regional development. Int J Parasitol, 2014. 44(9): p. 597-603.
-
Hotez, P.J., et al., The neglected tropical diseases of Latin America and the Caribbean: a review of disease burden and distribution and a roadmap for control and elimination. PLoS Negl Trop Dis, 2008. 2(9): p. e300.
-
World Health Organization. PCT Databank. 2014 [cited December 2015];
Available from: http://www.who.int/neglected_diseases/preventive_chemotherapy/databank/en/. -
Schneider, M.C., et al., Elimination of neglected diseases in latin america and the Caribbean: a mapping of selected diseases. PLoS Negl Trop Dis, 2011. 5(2): p. e964.
-
Schar, F., et al., Strongyloides stercoralis: Global Distribution and Risk Factors. PLoS Negl Trop Dis, 2013. 7(7): p. e2288.
-
Bhattarai, R., et al., Estimating the non-monetary burden of neurocysticercosis in Mexico. PLoS Negl Trop Dis, 2012. 6(2): p. e1521.
-
Botero, D., et al., Taeniasis and cysticercosis. Infect Dis Clin North Am, 1993. 7(3): p. 683-97.
-
Medina, M.T., et al., Reduction in rate of epilepsy from neurocysticercosis by community interventions: the Salama, Honduras study. Epilepsia, 2011. 52(6): p. 1177-85.
-
Cook, D.M., et al., A retrospective analysis of prevalence of gastrointestinal parasites among school children in the Palajunoj Valley of Guatemala. J Health Popul Nutr, 2009. 27(1): p. 31-40.
-
Chero, J.C., et al., Hymenolepis nana infection: symptoms and response to nitazoxanide in field conditions. Trans R Soc Trop Med Hyg, 2007. 101(2): p. 203-5.
-
Drugs for Parasitic Infections. 3rd ed. 2013, New Rochelle, NY: The Medical Letter.
-
World Health Organization. Guatemala. Noncommunicable Disease Country Profiles 2014 [cited 2015 December];
Available from: http://www.who.int/nmh/countries/gtm_en.pdf [PDF - 1 page]. -
World Health Organization. Country Cooperation Strategy, Guatemala. [cited 2015 December];
Available from: http://apps.who.int/iris/bitstream/10665/136864/1/ccsbrief_gtm_en.pdf [PDF - 1 page]. -
World Health Organization. El Salvador. Noncommunicable Disease Country Profiles 2014 [cited 2015 December];
Available from: http://www.who.int/nmh/countries/slv_en.pdf [PDF - 1 page]. -
World Health Organization. Country Cooperation Strategy, Honduras. 2013 [cited 2015 December];
Available from: http://apps.who.int/iris/bitstream/10665/136893/1/ccsbrief_hnd_en.pdf [PDF - 2 pages]. -
The World Bank. Nutrition at a Glance, El Salvador. [cited 2015 December];
Available from: http://siteresources.worldbank.org/NUTRITION/Resources/281846-1271963823772/ElSalvador91311web.pdf [PDF - 2 pages]. -
The World Bank. Nutrition at a Glance, Guatemala. [cited 2015 December];
Available from: http://siteresources.worldbank.org/NUTRITION/Resources/281846-1271963823772/Guatemala.pdf [PDF - 2 pages]. -
The World Bank. Nutrition at a Glance, Honduras. [cited 2015 December];
Available from: http://www-wds.worldbank.org/external/default/WDSContentServer/WDSP/IB/2013/05/10/000333037_20130510152029/Rendered/PDF/771720BRI0Box000honduras0April02011.pdf [PDF - 2 pages]. -
The World Bank. Data by country. [cited 2015 December]; Available from: http://data.worldbank.org/indicator/SP.DYN.IMRT.IN/countries.
-
World Health Organization. The worldwide prevalence of anaemia, 1993-2005. [cited 2015 December];
Available from: http://apps.who.int/iris/bitstream/10665/43894/1/9789241596657_eng.pdf [PDF - 51 pages]. -
American Academy of Pediatrics. State Medicaid Payment for Caries Prevention Services by Non-Dental Professionals. 2013;
Available from: http://www2.aap.org/oralhealth/docs/OHReimbursementChart.pdf [PDF - 12 pages]. -
US Preventive Services Task Force. Dental caries in children from birth through age 5 years: screening. May 2014;
Available from: http://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/dental-caries-in-children-from-birth-through-age-5-years-screening. -
Central Intelligence Agency. The World Factbook. [cited 2015 December]; Available from: https://www.cia.gov/library/publications/resources/the-world-factbook/index.html.
-
Martin-Herz, S.P., et al. Developmental screening with recent immigrant and refugee children: a preliminary report. 2012;
Available from: http://ethnomed.org/clinical/pediatrics/developmental-screening-with-recent-immigrant-and-refugee-children. -
Centers for Disease Control and Prevention. Developmental monitoring for health professionals. [cited 2015 December];
Available from: http://www.cdc.gov/ncbddd/childdevelopment/screening-hcp.html. -
American Academy of Pediatrics. Recommendations for preventative pediatric health care. [cited 2015 December];
Available from: https://www.aap.org/en-us/Documents/periodicity_schedule_oral_health.pdf [PDF - 2 pages]. -
National Newborn Screening & Global Resource Center. [cited 2015 December]; Available from: http://genes-r-us.uthscsa.edu/%3Cfront%3E.
-
World Health Organization. Lead: assessing the environmental burden of disease at national and local levels. [cited 2015 December];
Available from: http://www.who.int/quantifying_ehimpacts/publications/en/leadebd2.pdf?ua=1 [PDF - 73 pages]. -
Rivera, M.F., Prevalence of lead intoxication in public schools in Tegucigalpa. Revista Medica Hondureña, 1997. 65(3).
-
De Burgos, H., The site of lead: social poisoning in El Salvador. Anthropoligica, 2015. 57(1): p. 185-198.
-
Vigeh, M., H. Saito, and S. Sawada, Lead exposure in female workers who are pregnant or of childbearing age. Ind Health, 2011. 49(2): p. 255-61.
-
United Nations High Commissioner for Refugees, Children on the Run: Unaccompanied children leaving Central America and Mexico and the need for international protection.
-
Pan American Health Organization, Guatemala, in Health in the Americas, 2012 Edition: Country Volume. 2012.
-
Working with Immigrant-Origin Clients: An Update for Mental Health Professionals. 2013, American Psychological Association.
-
World Food Programme. El Salvador. 2016 [cited 2016 March 15]; Available from: https://www.wfp.org/countries/el-salvador/overview.
-
Lutter, C. and C. Chaarro, Malnutrition in infants and young children in Latin America and the Caribbean: Achieving the Millennium Development Goals. 2008, PAHO: Washington DC.
-
UNICEF, Stunting prevalence among children under five. June 2015.
-
World Food Programme. Guatemala. 2016 [cited 2016 March 15]; Available from: https://www.wfp.org/countries/guatemala.
-
World Health Organization, Global prevalence of vitamin A deficiency in populations at risk 1995-2005. WHO Global Database on Vitamin A Deficiency. . 2009, World Health Organization: Geneva.
-
World Food Programme. Honduras. 2016 [cited 2016 March 15]; Available from: https://www.wfp.org/countries/honduras.
-
FAO, The state of food insecurity in the world: economic crises-impacts and lessons learned. 2009.
-
Rivera, J.A., et al., Childhood and adolscent overweight and obesity in Latin America: a systematic review. Lancet Diabetes Endocrinol, 2014. 2: p. 321-32.
-
UNICEF, W.H.O. and World Bank, Joint Child Malnutrition Estimates: Levels and Trends. 2015.
-
Webber, L., et al., High rates of obesity and non-communicable diseases predicted across Latin America. PLoS One, 2012. 7(8): p. e39589.
-
World Health Organization, Global Infobase. 2016.
-
World Health Organization, Global Database on BMI. 2005.
-
Popkin, B.M., M.K. Richards, and C.A. Montiero, Stunting is associated with overweight in children of four nations that are undergoing the nutrition transition. J Nutr, 1996. 126(12): p. 3009-16.
-
Centers for Disease Control and Prevention. Defining childhood obesity. [cited 2015 December]; Available from: http://www.cdc.gov/obesity/childhood/defining.html.
-
American Academy of Pediatrics. Blood Pressure Tables for Children and Adolescents. [cited 2015 December];
Available from: http://www.nhlbi.nih.gov/health-pro/guidelines/current/hypertension-pediatric-jnc-4/blood-pressure-tables.
- Page last reviewed: January 25, 2017
- Page last updated: January 25, 2017
- Content source:


 ShareCompartir
ShareCompartir