HIV Transmission
Myths persist about how HIV is transmitted. This section provides the facts about HIV risk from different types of sex, injection drug use, and other activities.
How is HIV passed from one person to another?
You can get or transmit HIV only through specific activities. Most commonly, people get or transmit HIV through sexual behaviors and needle or syringe use.
Only certain body fluids—blood, semen (cum), pre-seminal fluid (pre-cum), rectal fluids, vaginal fluids, and breast milk—from a person who has HIV can transmit HIV. These fluids must come in contact with a mucous membrane or damaged tissue or be directly injected into the bloodstream (from a needle or syringe) for transmission to occur. Mucous membranes are found inside the rectum, vagina, penis, and mouth.
In the United States, HIV is spread mainly by
- Having anal or vaginal sex with someone who has HIV without using a condom or taking medicines to prevent or treat HIV.
- For the HIV-negative partner, receptive anal sex (bottoming) is the highest-risk sexual behavior, but you can also get HIV from insertive anal sex (topping).
- Either partner can get HIV through vaginal sex, though it is less risky for getting HIV than receptive anal sex.
- Sharing needles or syringes, rinse water, or other equipment (works) used to prepare drugs for injection with someone who has HIV. HIV can live in a used needle up to 42 days depending on temperature and other factors.
Less commonly, HIV may be spread
- From mother to child during pregnancy, birth, or breastfeeding. Although the risk can be high if a mother is living with HIV and not taking medicine, recommendations to test all pregnant women for HIV and start HIV treatment immediately have lowered the number of babies who are born with HIV.
- By being stuck with an HIV-contaminated needle or other sharp object. This is a risk mainly for health care workers.
In extremely rare cases, HIV has been transmitted by
- Oral sex—putting the mouth on the penis (fellatio), vagina (cunnilingus), or anus (rimming). In general, there’s little to no risk of getting HIV from oral sex. But transmission of HIV, though extremely rare, is theoretically possible if an HIV-positive man ejaculates in his partner’s mouth during oral sex. To learn more about how to lower your risk, see Oral Sex and HIV Risk.
- Receiving blood transfusions, blood products, or organ/tissue transplants that are contaminated with HIV. This was more common in the early years of HIV, but now the risk is extremely small because of rigorous testing of the US blood supply and donated organs and tissues.
- Eating food that has been pre-chewed by an HIV-infected person. The contamination occurs when infected blood from a caregiver’s mouth mixes with food while chewing. The only known cases are among infants.
- Being bitten by a person with HIV. Each of the very small number of documented cases has involved severe trauma with extensive tissue damage and the presence of blood. There is no risk of transmission if the skin is not broken.
- Contact between broken skin, wounds, or mucous membranes and HIV-infected blood or blood-contaminated body fluids.
- Deep, open-mouth kissing if both partners have sores or bleeding gums and blood from the HIV-positive partner gets into the bloodstream of the HIV-negative partner. HIV is not spread through saliva.
Learn more about how to protect yourself and get information tailored to meet your needs from CDC’s HIV Risk Reduction Tool (BETA).
How well does HIV survive outside the body?
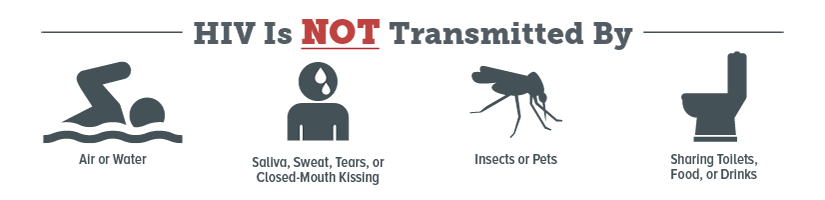
HIV does not survive long outside the human body (such as on surfaces), and it cannot reproduce outside a human host. It is not spread by
- Mosquitoes, ticks, or other insects.
- Saliva, tears, or sweat that is not mixed with the blood of an HIV-positive person.
- Hugging, shaking hands, sharing toilets, sharing dishes, or closed-mouth or “social” kissing with someone who is HIV-positive.
- Other sexual activities that don’t involve the exchange of body fluids (for example, touching).
Learn more about how to protect yourself and get information tailored to meet your needs from CDC’s HIV Risk Reduction Tool (BETA).
Can I get HIV from anal sex?
Yes. In fact, anal sex is the riskiest type of sex for getting or transmitting HIV.
HIV can be found in certain body fluids—blood, semen (cum), pre-seminal fluid (pre-cum), or rectal fluids—of a person who has HIV. Although receptive anal sex (bottoming) is much riskier for getting HIV than insertive anal sex (topping), it’s possible for either partner—the top or the bottom—to get HIV. The bottom’s risk is very high because the lining of the rectum is thin and may allow HIV to enter the body during anal sex. The top is also at risk because HIV can enter the body through the opening at the tip of the penis (or urethra); the foreskin if the penis isn’t circumcised; or small cuts, scratches, or open sores anywhere on the penis. See the Prevention Q&As for information on how to lower your risk of getting HIV from anal sex.
Learn more about how to protect yourself and get information tailored to meet your needs from CDC’s HIV Risk Reduction Tool (BETA).
Can I get HIV from vaginal sex?
Yes. Either partner can get HIV through vaginal sex, though it is less risky for getting HIV than receptive anal sex.
When a woman has vaginal sex with a partner who’s HIV-positive, HIV can enter her body through the mucous membranes that line the vagina and cervix. Most women who get HIV get it from vaginal sex.
Men can also get HIV from having vaginal sex with a woman who’s HIV-positive. This is because vaginal fluid and blood can carry HIV. Men get HIV through the opening at the tip of the penis (or urethra); the foreskin if they’re not circumcised; or small cuts, scratches, or open sores anywhere on the penis. See the Prevention Q&As for information on how to lower your risk of getting HIV from vaginal sex.
Learn more about how to protect yourself and get information tailored to meet your needs from CDC’s HIV Risk Reduction Tool (BETA).
Can I get HIV from oral sex?
The chance that an HIV-negative person will get HIV from oral sex with an HIV-positive partner is extremely low.
Oral sex involves putting the mouth on the penis (fellatio), vagina (cunnilingus), or anus (anilingus). In general, there’s little to no risk of getting or transmitting HIV through oral sex.
Factors that may increase the risk of transmitting HIV through oral sex are ejaculation in the mouth with oral ulcers, bleeding gums, genital sores, and the presence of other sexually transmitted diseases (STDs), which may or may not be visible.
You can get other STDs from oral sex. And, if you get feces in your mouth during anilingus, you can get hepatitis A and B, parasites like Giardia, and bacteria like Shigella, Salmonella, Campylobacter, and E. coli.
For information on how to lower your risk of getting HIV or other STDs from oral sex, see Oral Sex and HIV Risk.
Learn more about how to protect yourself and get information tailored to meet your needs from CDC’s HIV Risk Reduction Tool (BETA).
Is there a connection between HIV and other sexually transmitted infections?
Yes. Having another sexually transmitted disease (STD) can increase the risk of getting or transmitting HIV.
If you have another STD, you’re more likely to get or transmit HIV to others. Some of the most common STDs include gonorrhea, chlamydia, syphilis, trichomoniasis, human papillomavirus (HPV), genital herpes, and hepatitis. The only way to know for sure if you have an STD is to get tested. If you’re sexually active, you and your partners should get tested for STDs (including HIV if you’re HIV-negative) regularly, even if you don’t have symptoms.
If you are HIV-negative but have an STD, you are about 3 times as likely to get HIV if you have unprotected sex with someone who has HIV. There are two ways that having an STD can increase the likelihood of getting HIV. If the STD causes irritation of the skin (for example, from syphilis, herpes, or human papillomavirus), breaks or sores may make it easier for HIV to enter the body during sexual contact. Even STDs that cause no breaks or open sores (for example, chlamydia, gonorrhea, trichomoniasis) can increase your risk by causing inflammation that increases the number of cells that can serve as targets for HIV.
If you are HIV-positive and also infected with another STD, you are about 3 times as likely as other HIV-infected people to spread HIV through sexual contact. This appears to happen because there is an increased concentration of HIV in the semen and genital fluids of HIV-positive people who also are infected with another STD.
For more information about the connection between HIV and other STDs, see STDs and HIV. To get tested for HIV or other STDs, find a testing site near you.
Learn more about how to protect yourself and get information tailored to meet your needs from CDC’s HIV Risk Reduction Tool (BETA).
Does my HIV-positive partner’s viral load affect my risk of getting HIV?
Yes, as an HIV-positive person’s viral load goes down, the chance of transmitting HIV goes down.
Viral load is the amount of HIV in the blood of someone who is HIV-positive. When the viral load is very low, it is called viral suppression. Undetectable viral load is when the amount of HIV in the blood is so low that it can’t be measured.
In general, the higher someone’s viral load, the more likely that person is to transmit HIV. People who have HIV but are in care, taking HIV medicines, and have a very low or undetectable viral load are much less likely to transmit HIV than people who have HIV and do not have a low viral load.
However, a person with HIV can still potentially transmit HIV to a partner even if they have an undetectable viral load, because
- HIV may still be found in genital fluids (semen, vaginal fluids). The viral load test only measures virus in blood.
- A person’s viral load may go up between tests. When this happens, they may be more likely to transmit HIV to partners.
- Sexually transmitted diseases increase viral load in genital fluids.
If you’re HIV-positive, getting into care and taking HIV medicines (called antiretroviral therapy or ART) the right way, every day will give you the greatest chance to get and stay virally suppressed, live a longer, healthier life, and reduce the chance of transmitting HIV to your partners.
If you’re HIV-negative and have an HIV-positive partner, encourage your partner to get into care and take HIV treatment medicines.
Taking other actions, like using a condom the right way every time you have sex or taking daily medicine to prevent HIV (called pre-exposure prophylaxis or PrEP) if you’re HIV-negative, can lower your chances of transmitting or getting HIV even more.
Learn more about how to protect yourself and get information tailored to meet your needs from CDC’s HIV Risk Reduction Tool (BETA).
Can I get HIV from injecting drugs?
Yes. Your risk for getting HIV is very high if you use needles or works (such as cookers, cotton, or water) after someone with HIV has used them.
People who inject drugs, hormones, steroids, or silicone can get HIV by sharing needles or syringes and other injection equipment. The needles and equipment may have someone else’s blood in them, and blood can transmit HIV. Likewise, you’re at risk for getting hepatitis B and C if you share needles and works because these infections are also transmitted through blood.
Another reason people who inject drugs can get HIV (and other sexually transmitted diseases) is that when people are high, they’re more likely to have risky sex.
Stopping injection and other drug use can lower your chances of getting HIV a lot. You may need help to stop or cut down using drugs, but many resources are available. To find a substance abuse treatment center near you, check out the locator tools on SAMHSA.gov or HIV.gov, or call 1-800-662-HELP (4357).
If you keep injecting drugs, you can lower your risk for getting HIV by using only new, sterile needles and works each time you inject. Never share needles or works. For more information on how to lower your risk, see How can I prevent getting HIV from drug use?
Learn more about how to protect yourself, and get information tailored to meet your needs from CDC’s HIV Risk Reduction Tool (BETA).
Can I get HIV from using other kinds of drugs?
When you’re drunk or high, you’re more likely to make decisions that put you at risk for HIV, such as having sex without a condom.
Drinking alcohol, particularly binge drinking, and using “club drugs” like Ecstasy, ketamine, GHB, and poppers can alter your judgment, lower your inhibitions, and impair your decisions about sex or other drug use. You may be more likely to have unplanned and unprotected sex, have a harder time using a condom the right way every time you have sex, have more sexual partners, or use other drugs, including injection drugs or meth. Those behaviors can increase your risk of exposure to HIV. If you have HIV, they can also increase your risk of spreading HIV to others. Being drunk or high affects your ability to make safe choices.
If you’re going to a party or another place where you know you’ll be drinking or using drugs, you can bring a condom so that you can reduce your risk if you have vaginal or anal sex.
Therapy, medicines, and other methods are available to help you stop or cut down on drinking or using drugs. Talk with a counselor, doctor, or other health care provider about options that might be right for you. To find a substance abuse treatment center near you, check out the locator tools on SAMHSA.gov or HIV.gov, or call 1-800-662-HELP (4357).
Learn more about how to protect yourself, and get information tailored to meet your needs from CDC’s HIV Risk Reduction Tool (BETA).
If I already have HIV, can I get another kind of HIV?
Yes. This is called HIV superinfection.
HIV superinfection is when a person with HIV gets infected with another strain of the virus. The new strain of HIV can replace the original strain or remain along with the original strain.
The effects of superinfection differ from person to person. Superinfection may cause some people to get sicker faster because they become infected with a new strain of the virus that is resistant to the medicine (antiretroviral therapy or ART) they’re taking to treat their original infection.
Research suggests that a hard-to-treat superinfection is rare. Taking medicine to treat HIV (ART) may reduce someone’s chance of getting a superinfection.
Learn more about how to protect yourself, and get information tailored to meet your needs from CDC’s HIV Risk Reduction Tool (BETA).
Are health care workers at risk of getting HIV on the job?
The risk of health care workers being exposed to HIV on the job (occupational exposure) is very low, especially if they use protective practices and personal protective equipment to prevent HIV and other blood-borne infections. For health care workers on the job, the main risk of HIV transmission is from being stuck with an HIV-contaminated needle or other sharp object. However, even this risk is small. Scientists estimate that the risk of HIV infection from being stuck with a needle used on an HIV-infected person is less than 1%.
For more information on preventing occupational exposure to HIV, see Occupational HIV Transmission and Prevention Among Health Care Workers.
Learn more about how to protect yourself, and get information tailored to meet your needs from CDC’s HIV Risk Reduction Tool (BETA).
Can I get HIV from receiving medical care?
Although HIV transmission is possible in health care settings, it is extremely rare.
Careful practice of infection control, including universal precautions (using protective practices and personal protective equipment to prevent HIV and other blood-borne infections), protects patients as well as health care providers from possible HIV transmission in medical and dental offices and hospitals.
The risk of getting HIV from receiving blood transfusions, blood products, or organ/tissue transplants that are contaminated with HIV is extremely small because of rigorous testing of the US blood supply and donated organs and tissues.
It is important to know that you cannot get HIV from donating blood. Blood collection procedures are highly regulated and safe.
For more information on preventing occupational exposure to HIV, see Occupational HIV Transmission and Prevention Among Health Care Workers.
Learn more about how to protect yourself, and get information tailored to meet your needs from CDC’s HIV Risk Reduction Tool (BETA).
Can I get HIV from casual contact (“social kissing,” shaking hands, hugging, using a toilet, drinking from the same glass, or the sneezing and coughing of an infected person)?
No. HIV isn’t transmitted
- By hugging, shaking hands, sharing toilets, sharing dishes, or closed-mouth or “social” kissing with someone who is HIV-positive.
- Through saliva, tears, or sweat that is not mixed with the blood of an HIV-positive person.
- By mosquitoes, ticks or other blood-sucking insects.
- Through the air.
Only certain body fluids—blood, semen (cum), pre-seminal fluid (pre-cum), rectal fluids, vaginal fluids, and breast milk—from an HIV-infected person can transmit HIV. Most commonly, people get or transmit HIV through sexual behaviors and needle or syringe use. Babies can also get HIV from an HIV-positive mother during pregnancy, birth, or breastfeeding. See How is HIV passed from one person to another?
Learn more about how to protect yourself, and get information tailored to meet your needs from CDC’s HIV Risk Reduction Tool (BETA).
Can I get HIV from a tattoo or a body piercing?
There are no known cases in the United States of anyone getting HIV this way. However, it is possible to get HIV from a reused or not properly sterilized tattoo or piercing needle or other equipment, or from contaminated ink.
It’s possible to get HIV from tattooing or body piercing if the equipment used for these procedures has someone else’s blood in it or if the ink is shared. The risk of getting HIV this way is very low, but the risk increases when the person doing the procedure is unlicensed, because of the potential for unsanitary practices such as sharing needles or ink. If you get a tattoo or a body piercing, be sure that the person doing the procedure is properly licensed and that they use only new or sterilized needles, ink, and other supplies.
Learn more about how to protect yourself, and get information tailored to meet your needs from CDC’s HIV Risk Reduction Tool (BETA).
Can I get HIV from being spit on or scratched by an HIV-infected person?
No. HIV isn’t spread through saliva, and there is no risk of transmission from scratching because no body fluids are transferred between people.
Learn more about how to protect yourself, and get information tailored to meet your needs from CDC’s HIV Risk Reduction Tool (BETA).
Can I get HIV from mosquitoes?
No. HIV is not transmitted by mosquitoes, ticks, or any other insects.
Learn more about how to protect yourself, and get information tailored to meet your needs from CDC’s HIV Risk Reduction Tool (BETA).
Can I get HIV from food?
You can’t get HIV from consuming food handled by an HIV-infected person. Even if the food contained small amounts of HIV-infected blood or semen, exposure to the air, heat from cooking, and stomach acid would destroy the virus.
Though it is very rare, HIV can be spread by eating food that has been pre-chewed by an HIV-infected person. The contamination occurs when infected blood from a caregiver’s mouth mixes with food while chewing. The only known cases are among infants.
Learn more about how to protect yourself, and get information tailored to meet your needs from CDC’s HIV Risk Reduction Tool (BETA).
Are lesbians or other women who have sex with women at risk for HIV?
Case reports of female-to-female transmission of HIV are rare. The well-documented risk of female-to-male transmission shows that vaginal fluids and menstrual blood may contain the virus and that exposure to these fluids through mucous membranes (in the vagina or mouth) could potentially lead to HIV infection.
Learn more about how to protect yourself, and get information tailored to meet your needs from CDC’s HIV Risk Reduction Tool (BETA).
Is the risk of HIV different for different people?
Some groups of people in the United States are more likely to get HIV than others because of many factors, including the status of their sex partners, their risk behaviors, and where they live.
When you live in a community where many people have HIV infection, the chances of having sex or sharing needles or other injection equipment with someone who has HIV are higher. You can use CDC’s HIV, STD, hepatitis, and tuberculosis atlas to see the percentage of people with HIV (“prevalence”) in different US communities. Within any community, the prevalence of HIV can vary among different populations.
Gay and bisexual men have the largest number of new diagnoses in the United States. Blacks/African Americans and Hispanics/Latinos are disproportionately affected by HIV compared to other racial and ethnic groups. Also, transgender women who have sex with men are among the groups at highest risk for HIV infection, and injection drug users remain at significant risk for getting HIV.
Risky behaviors, like having anal or vaginal sex without using a condom or taking medicines to prevent or treat HIV, and sharing needles or syringes play a big role in HIV transmission. Anal sex is the highest-risk sexual behavior. If you don’t have HIV, being a receptive partner (or bottom) for anal sex is the highest-risk sexual activity for getting HIV. If you do have HIV, being the insertive partner (or top) for anal sex is the highest-risk sexual activity for transmitting HIV.
But there are more tools available today to prevent HIV than ever before. Choosing less risky sexual behaviors, taking medicines to prevent and treat HIV, and using condoms with lubricants are all highly effective ways to reduce the risk of getting or transmitting HIV. Learn more about these and other strategies to prevent HIV.
For more information about the risk for different groups of people, see HIV in the United States and HIV by Geographical Distribution.
Learn more about how to protect yourself, and get information tailored to meet your needs from CDC’s HIV Risk Reduction Tool (BETA).
Content provided and maintained by the US Centers for Disease Control and Prevention (CDC). Please see our system usage guidelines and disclaimer.
- Page last reviewed: May 30, 2017
- Page last updated: May 30, 2017
- Content source:


 ShareCompartir
ShareCompartir