Diphallia
Diphallia, penile duplication (PD), diphallic terata, or diphallasparatus, is an extremely rare developmental abnormality in which a male is born with two penises.[1][2] The first reported case was by Johannes Jacob Wecker in 1609.[3][4] Its occurrence is 1 in 5.5 million boys in the United States.[5]
| Diphallia | |
|---|---|
 | |
| Diphallia |
When diphallia is present, it is usually accompanied by renal, vertebral, hindgut, anorectal or other congenital anomalies. There is also a higher risk of spina bifida.[4] Infants born with PD and its related conditions have a higher death rate from various infections associated with their more complex renal or colorectal systems.
It is thought diphallia occurs in the fetus between the 23rd and 25th days of gestation when an injury, chemical stress, or malfunctioning homeobox genes hamper proper function of the caudal cell mass of the fetal mesoderm as the urogenital sinus separates from the genital tubercle and rectum to form the penis.
The occurrence is rare, at once in every five to six million live births,[6] with 1 in 5.5 million boys in the United States.[5]
The first case was reported by Wecker in Bologna, Italy in 1609, and since then, about one hundred cases have been reported until today.[1][6] This condition has existed in humans since ancient times.[7] The two external genitalia may vary in size and shape,[8] either lying beside each other in a sagittal plane or one above the other in a frontal plane.[9]
According to Schneider classification in 1928, double penis is classified into three groups: (a) glans diphallia, (b) bifid diphallia and (c) complete diphallia or double penis.[10] According to Vilanora and Raventos, in 1954, a fourth group called pseudodiphallia is added.[11]
The current widely accepted classification, introduced by Aleem in 1972, classifies double penis into two groups: true diphallia and bifid phallus.[8] True diphallia is caused by cleavage of pubic tubercle; bifid phallus is caused by separation of pubic tubercle.[8][12] Each of these two groups is further subdivided into partial or complete.[8] True diphallia is where each phallus has two corpora cavernosa and a single corpus spongiosum containing a urethra.[8][12] True diphallia can be either complete with both penises similar in size, or partial when one of the phallia is smaller in size or immature, though structurally same as the larger phallus.[8] In bifid phallus, each phallus has only one corpus cavernosum and one corpus spongiosum containing a urethra.[8][12] When the separation of penises is way down to base of penile shaft, is complete bifid; whereas to glans is partial bifid.[8] For complete bifid phallus associated with anomalies, the anterior urethra is absent from each penis and the prostatic urethra is situated in the skin between the two penises.[13] In partial bifid phallus, the duplication of urethra, corpora cavernous and corpus spongiosum in one penis is incomplete, and there is only a corpus cavernosum and a spongiosum surrounding the functioning urethra in the other penis.[14]
Notable Clinical Cases
Diphallia is usually accompanied by systemic anomalies, their extent varies, ranging from no associated anomaly to multiple anomalies including urogenital, gastrointestinal and musculoskeletal systems.[1][8] Penile duplication also varies from a single penis with double glans to complete double penises.[6] The meatus may be normal at tip of glans, hypospadiac, or epispadiac; the scrotum may be normal or bifid.[14] True diphallia is more likely accompanied with associated anomalies and malformations compared with bifid phallus.[1] Infants born with diphallia have higher death rate due to infections associated with anomalies.[13]
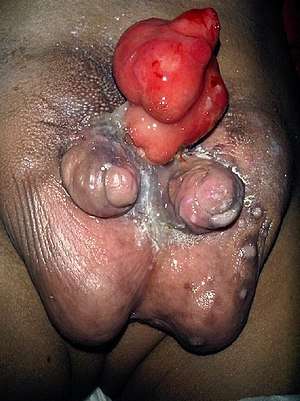
(A) Complete true diphallia with associated anomalies
A 2-day old male newborn,[6] associated with complex genitourinary and ano-rectal malformation. He had imperforated anus, hypospadias, bifid scrotum, meatuses on both glandes, two bladders and two colons, and had normal testes, kidneys and urethers. (Refer Figure 3.)
(B) Partial true diphallia or pseudodiphallia, without associated anomalies
Partial true diphallia corresponds to pseudodiphallia.[1] Pseudodiphallia is formed from erectile tissue only, undifferentiated and non-functional.[13] It is independent of the normal penis [10] and can be removed surgically without problem.[13] This rare case was reported,[13] based on the age of the 83-year-old man when diphallia was only detected then when he was hospitalised, and also because of the absence of other anatomical malformations. The small, immature and nonfunctional penis protruded on one side of the large, normal penis. The secondary penis had glans but without urinary meatus. (Refer Figure 1.)
(C) Complete bifid diphallia with associated anomalies
A 12-year-old boy,[1] associated with bifid scrotum, epispadia and pubic symphysis diastasis. He had two separate penises, similar in size and shape, each penis had an epispadia urethral meatus. He had bifid scrotum, one testicle on each side of the scrotum. A bowel loop-like structure was over the pubis region. This structure had no communication with any other structures. He had a single normal bladder and ureter. (Refer Figure 2.)
(D) Partial bifid diphallia without associated anomalies
A 15-year-old boy,[14] apart from having two penises, had normal external genitalia. His two testicles were within normal scrotum and normally positioned. He had two unequal sized glandes at tip of a thick penile shaft, and only urinated through the larger glans. He had a patent anus, one bladder, one normal urethra, normal gastrointestinal and genitourinary systems. (Refer Figure 4.)
Male sex determination
A male inherits an X chromosome from mother and a Y chromosome from father. The presence of the sex-determining-region of the Y chromosome, or SRY gene, determines the embryo being a male. Internal and external male genitalia development from bipotential gonad in embryo. SRY gene encodes testis-determining SRY factor (TDF) protein that promotes expression of several other genes such as SRY-box 9 (SOX-9) gene and steroidogenic factor-1 (SF1) gene, causing differentiation of the medulla of bipotential gonad into testis by week six.[15]
Internal genitalia development
Sertoli cells of testes secrete anti-Müllerian hormone (AMH) causing Müllerian ducts to generate, and Leydig cells of testes secrete testosterone and its derivative dihydrotestosterone (DHT) which is converted from testosterone by 5α-reductase, causing the Wolffian ducts to convert into seminal vesicles, vas deferens and epididymis by week ten.
External genitalia development
Initial development of external genital is independent of androgens before indifferent gonads differentiate into testes.[12] It occurs by week eight of gestation, as directed by a number of genes. External genitalia develop from mesenchymal cells underlying coelomic epithelium lining urogenital ridges on posterior wall of abdomen.[16] Primordial germ cells (PGCs), precursors of gametes,[17] migrate from egg sac into urogenital ridges, the site of gonad development in early embryonic development, by week six.[18] Genital ridges secrete a chemoattractant causing PGCs migration.[16] Around week three, the mesenchyme cells migrate around the cloacal membrane forming a pair of cloacal folds laterally around the cloacal membrane.[10][12] From week six, the anterior cloacal folds fuse to form genital tubercle, the posterior cloacal folds divide into anterior urogenital folds and posterior anal folds.[10][19] The cloacal membrane, divides into urogenital and anal membranes,[20] breaks to form anterior urogenital opening and posterior anal opening respectively.[20][21] Also from week six, labioscrotal swellings develop laterally of urogenital folds,[10][19] and labioscrotal swellings later form scrotal swellings.[10][19][12]
Hormone–dependent development of external genitalia begins at about week eight.[12] External genitalia differentiates under the action of testosterone and DHT. DHT causes development of other male sex characteristics, such as prostate development, differentiation of external genitalia including genital tubercle elongation forming glans penis, urogenital folds forming penile shaft and labioscrotal swellings forming scrotum by week ten.[15] Without DHT, male external genitalia will not develop during embryo growth.[15][18] Cells of urogenital ridges and underlying mesenchyme proliferate and form primary sex cords, which then undergo a series of mitotic division, under influence of TDF, develop into male gonad.[18][16] Elongation of genital tubercle forms developing glans penis.[15] As phallus elongates, it pulls forward urethral folds that surrounds urogenital sinus together.[20] Fusion of urogenital folds forms urogenital groove on ventral (under) side of phallus, and the groove gradually closes towards the glans forming the penile urethra.[20][22] The urogenital sinus differentiates into bladder and prostatic and posterior urethra.[23] Erectile mesenchymal tissue develops into corpus spongiosum around the urethra and forms the glans penis, and into corpora cavenosa in the penile shaft.[20]
Cause
Cause of diphallia is unknown,[13] and also because its associated anomalies vary largely, it is impossible to give a simple, single explanation of its cause.[12] But it is thought to have started from duplication of cloacal membrane in early embryonic development stages in the fetus, between third and sixth week of gestation,[13][7] because normal development of cloacal folds in the fetus is complete between this time.[10][22]
Normal development of penis occurs with the fusion of cloacal tubercles at anterior end of urogenital sinus.[1][13] Mesenchyme migrate around cloacal membrane, proliferate and expand around cloacal plate, forming a pair of cloacal folds that fuse to form genital tubercle which develops into penis.[13][1][12] If cloacal membrane is doubled, mesenchyme will migrate and surround both cloacal membranes, leading to the formation of two pairs of cloacal folds around two cloacal membranes, resulting in formation of two genital tubercles and thus two penises.[1][12] The concept of caudal duplication syndrome is used to explain the symptoms of diphallia with associated complex anomalies in lower abdomen and urinary tract.[22][12] Further, as mesenchyme migrate from more than one area, failure in migration and in the fusion of mesoderm results in formation of two genital tubercles [1] and double penises, as well as producing associated anomalies such as double bladders, double urethra, double colons and imperforated anus.[13][12] Failure in proper fusion of urethral folds results in hypospadias.[24] Failure in mesoderm cell migration results in epispadia.[23]
Diphallia is a rare abnormal external genitalia. The cause is uncertain, but most scientists agree that diphallia is a defect of genital tubercle, and occurs at about week three of gestation, when caudal cell mass of mesoderm is affected by various external environmental factors including drugs, infections and malfunctioning homeobox genes.[11][2]
Treatment
Treatment is a case-by-case analysis taking into account of many considerations including medical and ethical, and involves surgical excision of the non-functioning penis.[1]
References
- Tirtayasa, Pande (2013). "Diphallia with Associated Anomalies: A Case Report and Literature Review". Case Reports in Urology: 1–4. PMC 3870645. Archived from the original on 2019-08-09. Retrieved 2018-06-07 – via ProQuest.
- Aparicio-Rodríguez, J (2010). "Disorders of sexual development in genetic pediatrics: Three different ambiguous genitalia cases report from hospital para el Nino Poblano, Mexico". International Journal of Genetics and Molecular Biology. 2 (10): 207–216.
- Sharma KK, Jain R, Jain SK, Purohit A (2000). "Concealed diphallus :a Case report and review of the literature". Journal of Indian Association of Pediatric Surgeons. 5 (1): 18–21. Archived from the original on 2000.
- Mirshemirani, AR; Sadeghyian, N; Mohajerzadeh, L; Molayee, H; Ghaffari, P (2010). "Diphallus: Report on six cases and review of the literature". Iranian Journal of Pediatrics. 20 (3): 353–7. PMC 3446048. PMID 23056729.
- "Indian man wants op to remove extra organ". Reuters. 19 August 2006. Archived from the original on 22 January 2007. Retrieved 2006-08-18.
- Mirshemirani, Ali-Reza (2010). "Diphallus: Report on Six Cases and Review of the Literature". Iranian Journal of Pediatrics. 20 (3): 353–357.
- Karabagli, Murat (2017). "Bifid phallus with complete duplication and a separate scrotum in a German shepherd dog: a case report". Veterinarni Medicina. 62 (4): 226–230. doi:10.17221/16/2017-VETMED.
- Gyftopoulos, Kostis (2002). "Clinical and embryologic aspects of penile duplication and associated anomalies". Urology. 60 (4): 675–679. doi:10.1016/S0090-4295(02)01874-5.
- Wojewski, A (1964). "Total diphallia: A case of plastic repair". Plastic and Reconstructive Surgery. 34 (1): 106. doi:10.1097/00006534-196407000-00032.
- Aboodi, M.d M (2005). "Accessory Pseudophallus With Accessory Pseudoscrotum Detected During Antenatal Sonographic Scanning". Journal of Ultrasound in Medicine. 24 (8): 1163–1166. doi:10.7863/jum.2005.24.8.1163.
- Kundal, Vijay (2013). "A rare case of isolated complete diphallia and review of the literature". BMJ Case Reports. 2013. PMC 3603707. Archived from the original on 2019-08-09. Retrieved 2018-06-07 – via ProQuest.
- deVries, Catherine (2013). "Congenital anomalies in children" (PDF). Retrieved 18 April 2018.
- Rossete-Cervantes, H (2016). "Diphallia: a case report". Revista Médica del Instituto Mexicano del Seguro Social. 54 (3): 401 – via PubMed.
- Karagöz, Yeşim (2014). "Isolated penile duplication: case report and literature review" (PDF). Causapedia. 3: 762.
- Silverthorn, Dee (2016). Human physiology: an integrated approach. London: Pearson. pp. 827–829. ISBN 9781292094939.
- Silverman, Ann. "Gonadal Development" (PDF). Department of Anatomy & Cell Biology. Retrieved 16 April 2018.
- Magnúsdóttir, Erna (2014). "How to make a primordial germ cell". Development. 141 (2): 245–252. doi:10.1242/dev.098269. PMID 24381195.
- Ross, Michael (2015). Histology: a text and atlas : with correlated cell and molecular biology. Wolters Kluwer/Lippincott Williams & Wilkins Health. pp. 791–792. ISBN 9781451187427.
- Wein, Alan (2016). Campbell-Walsh urology. Philadelphia: Elsevier. ISBN 9780323341486.
- Pansky, Ben (2015). "Development of The Male External Genital Organs". LifeMap Discovery. Retrieved 13 April 2018.
- Van Der Werff, J (2000). "Normal development of the male anterior urethra" (PDF). Teratology. 61 (3): 172–83. doi:10.1002/(SICI)1096-9926(200003)61:3<172::AID-TERA4>3.0.CO;2-B. PMID 10661906.
- Elumalai, Ganesh (2017). ""PENILE DUPLICATION" Embryological basis and its clinical importance". Elixir Embryology. Retrieved 14 April 2018.
- Levin, Terry (2007). "Congenital anomalies of the male urethra". Pediatric Radiology. 37 (9): 851–862. doi:10.1007/s00247-007-0495-0. PMC 1950215. PMID 17572890.
- Elumalai, Ganesh (2017). ""HYPOSPADIAS" ITS EMBRYOLOGICAL BASIS AND CLINICAL IMPORTANCE". Elixir Embryology: 44481–44487.
Notes
- A scientific paper of triphallia (3 penises) in a marine snail was reported.[1]
See also
Further reading
- Chadha R, Bagga D, Gupta S, Mahajan JK. (July 2001). "Complete diphallia associated with features of covered exstrophy." 36 (7): E12, W.B. Saunders Company. National Center for Biotechnology Information, US National Library of Medicine, National Institutes of Health
- Fleishman, Cooper (May 15, 2012). "Man With 2 Penises, Woman With 2 Vaginas Were the Sexiest Couple of the 19th Century". HyperVocal.
External links
| Classification | |
|---|---|
| External resources |
|
- Castillo, Viviana M; Brown, Donald I (2012). "One Case of Triphallia in the Marine Snail Echinolittorina peruviana (Caenogastropoda: Littorinidae)". International Journal of Morphology. 30 (3): 791. doi:10.4067/S0717-95022012000300003.