Ureter
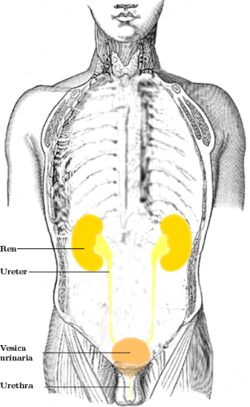
The ureters are tubes made of smooth muscle fibers that propel urine from the kidneys to the urinary bladder. In the adult, the ureters are usually 25–30 cm (10–12 in) long and around 3–4 mm (0.12–0.16 in) in diameter. The ureter is lined by urothelial cells, a type of transitional epithelium, and has an additional smooth muscle layer in the more distal one-third to assist with peristalsis.
| Ureter | |
|---|---|
 | |
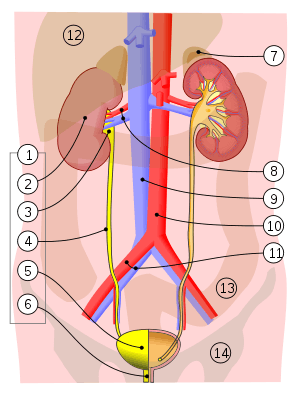 1. Human urinary system: 2. Kidney, 3. Renal pelvis, 4. Ureter, 5. Urinary bladder, 6. Urethra. (Left side with frontal section), 7. Adrenal gland Vessels: 8. Renal artery and vein, 9. Inferior vena cava, 10. Abdominal aorta, 11. Common iliac artery and vein With transparency: 12. Liver, 13. Large intestine, 14. Pelvis | |
| Details | |
| Precursor | Ureteric bud |
| System | Urinary system |
| Artery | Superior vesical artery, Vaginal artery, Ureteral branches of renal artery |
| Nerve | Ureteric plexus |
| Identifiers | |
| Latin | Ureter |
| MeSH | D014513 |
| TA | A08.2.01.001 |
| FMA | 9704 |
| Anatomical terminology | |
Structure
The ureters are tubular structures, approximately 3 mm (0.12 in) in adults, that pass from the pelvis of each kidney into the bladder. From the renal pelvis, they descend on top of the psoas major muscle to reach the brim of the pelvis. Here, they cross in front of the common iliac arteries. They then pass down along the sides of the pelvis, and finally curve forwards and enter the bladder from its left and right sides at the back of the bladder.[1][2]
The ureters enter the bladder from its back surface, traveling 1.5 - 2 cm before opening into the bladder on its outer back surface at the slit-like ureteric orifices.[1][3] In the contracted bladder they are about 25 mm (1 in) apart and about the same distance from the internal urethral orifice; in the distended bladder these measurements may be increased to about 50 mm (2 in).[1]
The junction between the pelvis of the kidney and the ureters is known as the ureteropelvic junction or ureteral pelvic junction, and the junction between the ureter and the bladder is known as the ureterovesical (ureter-bladder) junction. At the entrance to the bladder, the ureters are surrounded by valves known as ureterovesical valves, which prevent vesicoureteral reflux (backflow of urine).
A number of structures pass by, above, and around the ureters on their path down from the kidneys to the pelvis.[1] In females, the ureters pass through the mesometrium and under the uterine arteries on the way to the urinary bladder.
Blood and lymphatic supply
The ureter has an arterial supply which varies along its course.
- The upper part of the ureter closest to the kidney is supplied by the renal arteries.[1]
- The middle part of the ureter is supplied by the common iliac arteries, direct branches from the abdominal aorta, and gonadal arteries (the testicular artery in men or ovarian artery in women).[1]
- The lower part of the ureter closest to the bladder is supplied by branches from the internal iliac arteries, namely the:[1]
- Superior vesical artery
- Uterine artery[lower-alpha 1]
- Middle rectal artery
- Vaginal arteries[lower-alpha 2]
- Inferior vesical artery (only in men)
There are many connections (anastamoses) between the arteries of the ureter,[1] particularly in the aventitia,[4] which means damage to a single vessel does not compromise the blood supply of the ureter.[1][4] Venous drainage mostly parallels that of the arterial supply.[4][1]
Lymphatic drainage depends on the position of lymphatic vessels in the ureter. Lymph collects in submucosal, intramuscular and advential lymphatic vessels. Those vessels closer to the kidney drain into renal collecting vessels; into the lateral aortic nodes near the gonadal vessels. In the lower ureter, lymph may drain into the common iliac lymph nodes, or lower down in the pelvis to the common, external, or internal iliac lymph nodes.[1]
Nerve supply
The ureters are richly supplied by nerves that form a network (plexus) of nerves, the ureteric plexus that lies in the adventitia of the ureters.[5][1] This plexus is formed from a number of nerve roots directly (T9-12, L1, and S2-4), as well as branches from other nerve plexuses and nerves; specifically, the upper third of the ureter receives nerve branches from the renal plexus and aortic plexus, the middle part receives branches from the upper hypogastric plexus and nerve, and the lower ureter receives branches from the lower hypogastric plexus and nerve.[1] The plexus is in the adventitia. The these nerves travel in individual bundles and along small blood vessels to form the ureteric plexus.[1] Sensation supplied is sparse close to the kidneys and increases closer to the bladder.[1]
The primary sensation to the ureters is provided by nerves that come from T12-L2 segments of the spinal cord. Thus pain may be referred to the dermatomes of T12-L2, namely the back and sides of the abdomen, the scrotum (males) or labia majora (females) and upper part of the front of the thigh.[2]:324–326
Microanatomy
The ureter is lined by urothelium, a type of transitional epithelium that is capable of responding to stretches in the ureters. The transitional epithelium may appear as a layer of column-shaped cells when relaxed, and of flatter cells when distended. Below the epithelium sits the lamina propria. The lamina propria is made up of loose connective tissue with many elastic fibers interspersed with blood vessels, veins and lymphatics. The ureter is surrounded by two muscular layers, an inner longitudinal layer of muscle, and an outer circular or spiral layer of muscle.[6][7] The lower third of the ureter has a third muscular layer.[7] Beyond these layers sits an adventitia containing blood vessels, lymphatic vessels, and veins.[7]
 Microscopic cross-section of the ureter, showing the epithelium (purple cells) sitting next to the lumen. A large amount of muscle fibres can be seen surrounding the epithelium, and the adventitia sits beyond this
Microscopic cross-section of the ureter, showing the epithelium (purple cells) sitting next to the lumen. A large amount of muscle fibres can be seen surrounding the epithelium, and the adventitia sits beyond this
Variation
Congenital disorders of the ureter and urinary tract affect 10% of infants.[8] These include duplication of the ureter (a duplex ureter), or the formation of a second irregularly placed (ectopic) ureter. [8]
Development
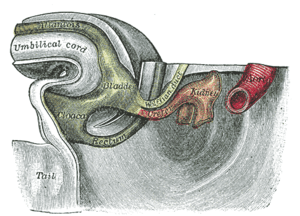
The ureters develop from the ureteric buds, which are outpuchings from the mesonephric duct. This is a duct, derived from mesoderm, found in the early embryo.[9] Over time, the buds elongate, moving into surrounding mesodermal tissue, dilate, and divide. Eventually, successive divisions from these buds form not only the ureters, but also the pelvis, major and minor calyces, and collecting ducts of the kidneys.[9]
The mesonephric duct is connected with the cloaca, which over the course of development splits into a urogenital sinus and the anorectal canal.[9] The urinary bladder forms from the urogenital sinus. Over time, as the bladder enlarges, it absorbs the surrounding parts of the primitive ureters.[9] Finally, the entry points of the ureters into the bladder move upwards, owing to the upward migration of the kidneys in the developing embryo.[9]
Function
The ureters are a component of the urinary system. Urine, produced by the kidneys, travels along the ureters to the bladder. It does this through regular contractions called peristalsis.[1]
 Ultrasound showing a jet of urine entering the bladder (large black section) through the ureter.
Ultrasound showing a jet of urine entering the bladder (large black section) through the ureter.
Clinical significance
Injury
Injuries to the ureter with certain forms of trauma including penetrating abdominal injuries and injuries at high speeds followed by an abrupt stop (e.g., a high speed car accident).[10] The ureter is injured in 0.2 per 1,000 cases of vaginal hysterectomies and 1.3 per 1,000 cases of abdominal hysterectomies,[11] near the infundibulopelvic (suspensory) ligament or where the ureter courses posterior to the uterine vessels, near the cardinal ligament.[12]
Ureteral stones
A kidney stone can move from the kidney and become lodged inside the ureter, which can block the flow of urine, as well as cause a sharp cramp in the back, side, or lower abdomen.[13] The affected kidney could then develop hydronephrosis, should a part of the kidney become swollen due to blocked flow of urine.[14] There are three sites where a kidney stone will commonly become stuck:
- at the ureteric junction of renal pelvis;
- as the ureter passes over the iliac vessels;
- where the ureter enters into the urinary bladder (vesicoureteric junction).
Reflux
Vesicoureteral reflux refers to the reflux of fluid from the bladder to the ureters during urination. This condition can be one cause of chronic urinary tract infections, particularly in children. It is unclear if there is a role of surgery in vesicoureteral reflux.[15]
Obstruction and enlargement
Blockage, or obstruction of the ureter can occur.[8]
Cancer
Cancer of the ureters is known as ureteral cancer and may have several causes. It is due to cancer of the urothelium, the cells that line the surface of the ureters. Urothelial cancer is more common after the age of 40, and more common in men than women. [16]
If the cancer is a squamous cell carcinoma, this is often associated with a change in the type of cells lining the ureters as a result of chronic inflammation associated with schistosomiasis or stones.[16]
Other
Failure of the ureteropelvic junction to become patent during development is the most frequent cause of bilateral hydronephrosis, particularly in male neonates. Pyeloplasty, which involves excision of the stenotic section and creation of a new junction, is the most common and effective treatment for this problem.
Other animals
Ureters are also found in all other amniote species, although different ducts fulfill the same role in amphibians and fish.[17] In marsupials, but not in placental mammals, the ureters pass between the oviducts during embryonic development.[18]
Notes
- only present in women
- only present in women
References
- Standring, Susan, ed. (2016). "Ureter". Gray's anatomy : the anatomical basis of clinical practice (41st ed.). Philadelphia. pp. 1251–1254. ISBN 9780702052309. OCLC 920806541.
- Drake, Richard L.; Vogl, Wayne; Mitchell, Adam W. M. (2005). Gray's Anatomy for Students. Illustrated by Richardson, Paul. Philadelphia: Elsevier/Churchill Livingstone. ISBN 978-0-8089-2306-0.
- Standring, Susan, ed. (2016). Gray's anatomy : the anatomical basis of clinical practice (41st ed.). Philadelphia. p. 1259. ISBN 9780702052309. OCLC 920806541.
- Wein, Alan J. (2011). Campbell-Walsh Urology (10th ed.). Elsevier. p. 31.
- Dudeck, Ronald W. (2007). High-Yield Kidney. High-Yield Systems (1st ed.). Lippincott Willams and Wilkins. p. 19. ISBN 978-0-7817-5569-6.
- Lowe, Alan Stevens, James S. (2005). Human histology (3rd ed.). Philadelphia & Toronto: Elsevier Mosby. p. 324. ISBN 0-3230-3663-5.
- Young, Barbara; O'Dowd, Geraldine; Woodford, Phillip. Wheater's functional histology: a text and colour atlas (6th ed.). Philadelphia: Elsevier. p. 314. ISBN 9780702047473.
- Ralston, Stuart H.; Penman, Ian D.; Strachan, Mark W.; Hobson, Richard P. (eds.) (2018). "Diseases of the collecting system and ureters". Davidson's principles and practice of medicine (23rd ed.). Elsevier. pp. 433–4. ISBN 978-0-7020-7028-0.CS1 maint: extra text: authors list (link)
- Sadley, TW (2019). "Urinary system". Langman's medical embryology (14th ed.). Philadelphia: Wolters Kluwer. pp. 256–266. ISBN 9781496383907.
- Stein, D. M.; Santucci, R. A. (July 2015). "An update on urotrauma". Current Opinion in Urology. 25 (4): 323–30. doi:10.1097/MOU.0000000000000184. PMID 26049876.
- Burks, F. N.; Santucci, R. A. (June 2014). "Management of iatrogenic ureteral injury". Therapeutic Advances in Urology. 6 (3): 115–24. doi:10.1177/1756287214526767. PMC 4003841. PMID 24883109.
- Santucci, Richard A. "Ureteral Trauma". Medscape. Retrieved 11 April 2012.
- "Symptoms of Kidney Stones". MedicalBug. 1 January 2012. Retrieved 11 April 2012.
- Resnick, Martin I.; Lam, Mildred; Zipp, Thomas (4 September 2009). "Kidney Stones". NetWellness. Retrieved 11 April 2012.
- Najar, M. S.; Saldanha, C. L.; Banday, K. A. (October 2009). "Approach to urinary tract infections". Indian Journal of Nephrology. 19 (4): 129–139. doi:10.4103/0971-4065.59333. ISSN 0971-4065. PMC 2875701. PMID 20535247.
- Ralston, Stuart H.; Penman, Ian D.; Strachan, Mark W.; Hobson, Richard P. (eds.) (2018). "Tumours of the kidney and urinary tract: Urothelial tumours". Davidson's principles and practice of medicine (23rd ed.). Elsevier. pp. 435–6. ISBN 978-0-7020-7028-0.CS1 maint: extra text: authors list (link)
- Romer, Alfred Sherwood; Parsons, Thomas S. (1977). The Vertebrate Body. Philadelphia, PA: Holt-Saunders International. p. 378. ISBN 0-03-910284-X.
- C. Hugh Tyndale-Biscoe (2005). Life of Marsupials. Csiro Publishing. pp. 7–. ISBN 978-0-643-09199-3.