Acid-fastness
Acid-fastness is a physical property of certain bacterial and eukaryotic cells, as well as some sub-cellular structures, specifically their resistance to decolorization by acids during laboratory staining procedures.[1][2] Once stained as part of a sample, these organisms can resist the acid and/or ethanol-based decolorization procedures common in many staining protocols, hence the name acid-fast.[2]
The mechanisms of acid-fastness vary by species, although the most well-known example is in the genus Mycobacterium, which includes the species responsible for tuberculosis and leprosy. The acid-fastness of Mycobacteria is due to the high mycolic acid content of their cell walls, which is responsible for the staining pattern of poor absorption followed by high retention. Some bacteria may also be partially acid-fast, such as Nocardia.
Acid-fast organisms are difficult to characterize using standard microbiological techniques, though they can be stained using concentrated dyes, particularly when the staining process is combined with heat. Some, such as Mycobacteria, can be stained with the Gram stain, but they do not take the crystal violet well and thus appear light purple, which can still potentially result in an incorrect gram positive identification.[3]
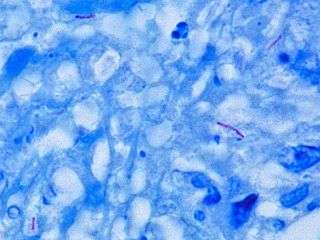
The most common staining technique used to identify acid-fast bacteria is the Ziehl-Neelsen stain, in which the acid-fast species are stained bright red and stand out clearly against a blue background. Another method is the Kinyoun method, in which the bacteria are stained bright red and stand out clearly against a green background. Acid-fast Mycobacteria can also be visualized by fluorescence microscopy using specific fluorescent dyes (auramine-rhodamine stain, for example).[4] The eggs of the parasitic lung fluke Paragonimus westermani are actually destroyed by the stain, which can hinder diagnosis in patients who present with TB-like symptoms.
Some acid-fast staining techniques
- Ziehl–Neelsen stain (classic and modified bleach types)[5]
- Kinyoun stain
- For color blind people (or in backgrounds where detecting red bacteria is difficult) Victoria Blue can be substituted for carbol fuchsin and picric acid can be used as the counter stain instead of methylene blue, and rest of Kinyoun technique can be used.[6]
- Fite stain[11]
- Ellis and Zabrowarny stain[15][16] (no phenol/carbolic acid)
- Auramine-rhodamine stain
- Auramine phenol stain
Notable acid-fast structures
Very few structures are acid-fast; this makes staining for acid-fastness particularly useful in diagnosis. The following are notable examples of structures which are acid-fast or modified acid-fast:
- All Mycobacteria - M. tuberculosis, M. leprae, M. smegmatis and atypical Mycobacterium
- Actinomycetes (especially some aerobic ones) with Mycolic acid in their cell wall (note Streptomyces do NOT have); not to be confused with Actinomyces, which is a non-acid-fast genera of Actinomycetes
- Nocardia
- Rhodococcus
- Gordonia (Actinomycete)
- Tsukamurella
- Dietzia
- Head of sperm
- Bacterial spores, see Endospore
- Legionella micdadei
- Certain cellular inclusions e.g.
- Cytoplasmic inclusion bodies seen in
- Neurons in layer 5 of cerebral cortex neuronal ceroid lipofuscinosis (Batten disease).
- Nuclear inclusion bodies seen in
- Lead poisoning
- Bismuth poisoning.
- Cytoplasmic inclusion bodies seen in
- Oocysts of some coccidian parasites in faecal matter, such as:
- A few other parasites:
- Sarcocystis
- Taenia saginata eggs stain well but Taenia solium eggs don't (Can be used to distinguish)
- Hydatid cysts, especially their "hooklets" stain irregularly with ZN stain but emanate bright red fluorescence under green light, and can aid detection in moderately heavy backgrounds or with scarce hooklets.[20]
- Fungal yeast forms are inconsistently stained with Acid-fast stain which is considered a narrow spectrum stain for fungi.[21] In a study on acid-fastness of fungi,[22] 60% of blastomyces and 47% of histoplasma showed positive cytoplasmic staining of the yeast-like cells, and Cryptococcus or candida did not stain, and very rare staining was seen in Coccidioides endospores.
References
- Madison B (2001). "Application of stains in clinical microbiology". Biotech Histochem. 76 (3): 119–25. doi:10.1080/714028138. PMID 11475314.
- Ryan KJ; Ray CG (editors) (2004). Sherris Medical Microbiology (4th ed.). McGraw Hill. ISBN 0-8385-8529-9.CS1 maint: extra text: authors list (link)
- Reynolds, Jackie; Moyes, Rita B.; Breakwell, Donald P. (November 2009). "Differential staining of bacteria: acid fast stain". Current Protocols in Microbiology. Appendix 3: Appendix 3H. doi:10.1002/9780471729259.mca03hs15. ISSN 1934-8533. PMID 19885935.
- Abe C (2003). "[Standardization of laboratory tests for tuberculosis and their proficiency testing]". Kekkaku. 78 (8): 541–51. PMID 14509226.
- "Acid fast / Auramine-rhodamine". www.pathologyoutlines.com.
- Theory and Practice of Histological Techniques, John D Bancroft, 6th ed, p314
- Dorner, W. 1926. Un procédé simple pour la colouration des spores. Le Lait 6:8-12.
- Schaeffer AB, Fulton M (1933). "A simplified method of staining endospores". Science. 77: 194.
- Endospore Stain Protocol from American Society for Microbiology website Archived 2012-06-01 at the Wayback Machine
- http://daignet.de/site-content/die-daig/fachorgan/2007-1/ejomr-2007_8-pdfs/S.356_Hayama.pdf
- "Stainsfile - Fite". stainsfile.info. Archived from the original on 2011-11-18. Retrieved 2012-06-28.
- "Fite-Faraco Staining Protocol for Leprosy Bacilli". www.ihcworld.com.
- "Stainsfile - Fite Faraco". stainsfile.info. Archived from the original on 2011-11-18. Retrieved 2012-06-28.
- "Stainsfile - Wade Fite". stainsfile.info. Archived from the original on 2011-11-18. Retrieved 2012-06-28.
- Ellis, R. C.; Zabrowarny, L. A. (1993). "Safer staining method for acid fast bacilli". Journal of Clinical Pathology. 46 (6): 559–560. doi:10.1136/jcp.46.6.559. PMC 501296. PMID 7687254.
- "Archived copy". Archived from the original on 2006-01-04. Retrieved 2006-03-11.CS1 maint: archived copy as title (link)
- Garcia LS, Bruckner DA, Brewer TC, Shimizu RY (July 1983). "Techniques for the recovery and identification of Cryptosporidium oocysts from stool specimens". J. Clin. Microbiol. 18 (1): 185–90. PMC 270765. PMID 6193138.
- Ng E, Markell EK, Fleming RL, Fried M (September 1984). "Demonstration of Isospora belli by acid-fast stain in a patient with acquired immune deficiency syndrome". J. Clin. Microbiol. 20 (3): 384–6. PMC 271334. PMID 6208216.
- Ortega YR, Sterling CR, Gilman RH, Cama VA, Díaz F (May 1993). "Cyclospora species--a new protozoan pathogen of humans". N. Engl. J. Med. 328 (18): 1308–12. doi:10.1056/NEJM199305063281804. PMID 8469253.
- Clavel A, Varea M, Doiz O, López L, Quílez J, Castillo FJ, Rubio C, Gómez-Lus R. "Visualization of hydatid elements: comparison of several techniques". J Clin Microbiol. 37: 1561–3. PMC 84828. PMID 10203521.
- "Dako Products - Agilent" (PDF). www.dako.com. Retrieved 3 December 2018.
- Wages ds, Wear dJ. acid-fastness of fungi in blastomycosis and histoplasmosis. Arch Pathol Lab Med 1982; 106:440-41.
Online protocol examples
- Ziehl-Neelsen protocol (PDF format).
- Alternate Ellis & Zabrowarny method for staining AFB.