We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
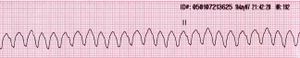
Tachycardia (wide)
From WikEM
(Redirected from Ventricular Tachycardia)
Contents
Background
- Consider Hyperkalemia, Dig Toxicity, severe metabolic acidosis
- Sustained ventricular tachycardia is VT > 30 seconds
- 3 beats is considered VT; less than 30 seconds is non-sustained VT
Epidemiology[1][2][3]
- WCT is due to ventricular tachycardia in 80% of cases
- For patients with underlying cardiac disease, this number increases to > 90%
Differential Diagnosis
Regular
- V-tach
- SVT w/ BBB (fixed or rate related)
- SVT w/ accessory pathway
- A flutter w/ BBB
- Sinus tachycardia with BBB (fixed or rate related)
- If less than or ~120 bpm, consider Accelerated Idioventricular Rhythm
Irregular
- A-fib/flutter w/ variable AV conduction AND BBB (fixed or rate-related)
- A-fib/flutter w/ variable AV conduction AND accessory pathway (eg WPW)
- A-fib + Hyperkalemia
- Polymorphic v-tach/torsades
Evaluation
- Assume ventricular tachycardia until proven otherwise
- See V Tach vs. SVT
Management
Pulseless: see Adult pulseless arrest
- Unstable:
- Regular: Synchronized cardioversion 100-200J
- Irregular: Unsynchronized cardioversion (defibrillation) 200J
- Stable
- Regular (treat as presumed V-tach)
- Procainamide 100 mg q5min at max rate of 25-50 mg/min[4]
- Until termination of arrhythmia, then start 2-6 mg/min (or 1-2 mg/min for renal/cardiac failure)
- OR max 17 mg/kg total dose given (12 mg/kg if renal failure)
- OR if QRS widens > 50%
- Amiodarone, agent of choice in setting of AMI or LV dysfunction
- 150 mg over 10min (15 mg/min), followed by 1 mg/min drip over 6hrs (360 mg total)[5]
- Then 0.5 mg/min drip over next 18 hrs (540 mg total)
- Oral dosage after IV infusion depends on IV infusion length:
- < 1 wk IV infusion: 800-1600 mg PO QD
- 1-3 wks: 600-800 mg PO QD
- > 3 wks: 400 mg PO QD
- Lidocaine 1-1.5mg/kg IV q5min, repeat prn until up to 300mg/hr
- Procainamide 100 mg q5min at max rate of 25-50 mg/min[4]
- Irregular (treat as presumed preexcited A-fib)
- Procainamide as above
- Amiodarone as above
- Sotalol (100mg IV over 5 minutes)
- Magnesium 1-2gm IV over 60-90s, then infuse 1-2gm/hr (for Torsades De Pointes)
- Regular (treat as presumed V-tach)
- Refractory
- ≥3 episodes within 24 hours considered electrical storm and may require alternate treatment (i.e. beta blockade, sedation, ablation)
- In very wide complex (>0.2 msec) and <120 bpm in a patient with significant history, consider giving calcium chloride to treat hyperkalemia and Bicarbonate for Na channelopathy
- Usually Vtach is >120 bpm
- Hyperkalemia, Acidosis, TCA toxicity poison Na channels
- Lidocaine, Procainamide, Amiodarone all block Na channels and may result in asystole in these patients
Disposition
- Admit all patients (even if converted to NSR with adenosine)
See Also
- ACLS: Tachycardia
- ACLS (Main)
- V Tach vs. SVT
- SVT
- Nonsustained ventricular tachycardia
- Polymorphic ventricular tachycardia
References
- ↑ Gupta AK, Thakur RK. Wide QRS complex tachycardias. Med Clin North Am. 2001;85(2):245–66– ix–x.
- ↑ Akhtar M, Shenasa M, Jazayeri M, Caceres J, Tchou PJ. Wide QRS complex tachycardia. Reappraisal of a common clinical problem. Ann Intern Med. 1988;109(11):905–912.
- ↑ Stewart RB, Bardy GH, Greene HL. Wide complex tachycardia: misdiagnosis and outcome after emergent therapy. Ann Intern Med. 1986;104(6):766–771.
- ↑ Procainamide. GlobalRPH. http://www.globalrph.com/procainamide_dilution.htm.
- ↑ Amiodarone. GlobalRPH. http://www.globalrph.com/amiodarone_dilution.htm.