We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
EFAST exam
From WikEM
Contents
Background
- Prioritize: Do primary survey of ATLS first ABCDE
- EFAST exam follows ABCDE to assess “C” looking for free fluid
- Sensitivity of 42% and specificity of ≥98%[1][2]
- As little as 100ml of free fluid can be seen[3][4], though >500ml is needed for the common user[5]
- If blunt trauma start with RUQ view first
- In penetrating start with cardiac views first to rule out tamponade
- Pulmonary ultrasound for clinically significant pneumothorax is associated with a sensitivity of 95.3%, specificity 91.1%, and negative predictive value 100%[6]
- Serial exams extremely helpful
Indications
- EFAST is useful in patients with blunt or penetrating traumatic injury
- Enables trauma bay decision:
- Stable patient with traumatic mechanism of injury + negative EFAST → observation
- Stable patient with traumatic mechanism of injury + positive EFAST → CT
- Unstable patient with traumatic mechanism of injury + negative EFAST → repeat FAST or CT
- Unstable patient with traumatic mechanism of injury + positive EFAST → laparotomy
- Patient with traumatic mechanism of injury + positive pulmonary findings on EFAST → chest tube
Technique
- Select probe
- Curvilinear/large convex probe is ideal but phased array probe may be substituted
- Linear probe for lung sliding though curvilinear or phased array probes can be substituted with depth decreased
- Location
- Sequence can vary depending on mechanism of injury
- Include cardiac, RUQ, pelvic, LUQ views, and pulmonary views
Cardiac
- Location
- Subxiphoid
- Landmarks
- Visualize the heart and pericardium using the liver as an acoustic window
- Scan anterior to posterior through the heart
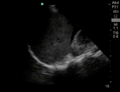
RUQ
- Location
- Coronal view over the right flank
- Landmarks
- Visualize the interface between the liver and kidney
- Scan anterior to posterior identifying Morison’s pouch and the superior and inferior pole of the kidney
Pelvic
- Location
- Sagittal view just superior to the pubic symphysis
- Landmarks
- Identify the bladder
- Scan medial to lateral to identify fluid posterior and superior to the bladder
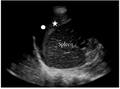
LUQ
- Location
- Coronal view over the left flank
- Landmarks
- Identify the space between the spleen and diaphragm and the spleen and the kidney
- Scan through anterior to posterior of the splenodiaphragmatic space and superior and inferior pole of the kidney
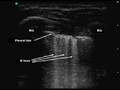
Pulmonary
- Location
- Coronal view over the right and left diaphragm (curvilinear probe)
- Sagittal view over the midclavicular line between the 2nd and 3rd intercostal space (linear probe)
- Landmarks
- Identify the interface between the diaphragm and lung on right and left (curvilinear probe)
- Identify lung sliding between two ribs over the anterior thorax (linear probe)
- Scan
- Scan anterior to posterior over the diaphragm on right and left (curvilinear probe)
- Hold probe in place between rib space observing for movement along the pleural line (linear probe)
Findings
- Positive FAST will have one of the following:
- Anechoic area within the pericardial space
- Anechoic areas between the liver and kidney
- Anechoic areas between the diaphragm and spleen
- Anechoic areas between the spleen and kidney
- Anechoic areas between superior and posterior to the posterior wall of the bladder
- Positive EFAST will have one of the added pulmonary findings:
- Anechoic area above the diaphragm between the diaphragm and lung
- Absent lung sliding - lack of lung rockets seen under the pleural line
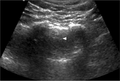
Images
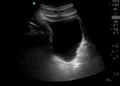
Normal
Abnormal
Pearls and Pitfalls
- Morison’s pouch
- Scans must scan through the inferior poles of the kidneys as this can contain small quantities of fluid
- Serial exam may be needed
- Negative exam does not rule out intraabdominal injuries
- Retroperitoneal hemorrhage no easily identified
- Those with delayed presentation may have clotted and not completely anechoic fluid collections
Documentation
Normal Exam
A bedside EFAST ultrasound was conducted to assess for free fluid with clinical indication of trauma. Cardiac, RUQ, pelvic, LUQ, and pulmonary views were adequately obtained. There was no free fluid identified. There was no pneumothorax or hemothorax identified.
Abnormal Exam
A bedside EFAST ultrasound was conducted to assess for free fluid with clinical indication of trauma. Cardiac, RUQ, pelvic, LUQ, and pulmonary views were adequately obtained. There was free fluid identified in the RUQ suggesting intraabdominal hemorrhage. There was a pneumothorax on the left.
Clips
Normal
Abnormal
External Links
- Sonoguide: Ultrasound in Trauma – The FAST Exam
- EMCrit: Podcast 102 – Don’t Half-Ass your FAST!
- eFAST : extended Focused Assessment with Sonography in Trauma
See Also
- FAST exam
- Cardiac ultrasound
- IVC ultrasound
- Ultrasound: Lungs
- Ultrasound (Main)
- Renal ultrasound
- Bladder ultrasound
- Abdominal Trauma
- Ultrasound: In Shock and Hypotension
References
- ↑ Natarajan B, Gupta PK, Cemaj S, et al. FAST scan: Is it worth doing in hemodynamically stable blunt trauma patients? Surgery. 2010;148(4):695-700.
- ↑ Miller MT, Pasquale MD, Bromberg WJ, et al. Not so FAST. J Trauma. 2003; 54(1):52-59.
- ↑ Goldberg GG. Evaluation of ascites by ultrasound. Radiology. 1970; 96(15):217–221.
- ↑ Von Kuenssberg Jehle D, Stiller G, Wagner D. Sensitivity in detecting free intraperitoneal fluid with the pelvic views of the FAST exam. Am J Emerg Med. 2003 Oct;21(6):476-478.
- ↑ McKenney KL, McKenney MG, Cohn SM, et al. Hemoperitoneum score helps determine need for therapeutic laparotomy. J Trauma 2001; 50(4):650–654.
- ↑ Lichtenstein DA and Menu Y. A bedside ultrasound sign ruling out pneumothorax in the critically ill. Lung sliding. Chest. 1995; 108(5):1345-1348.
.gif/120px-Subxiphoid_(Still).gif)