We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
Acute respiratory distress syndrome
From WikEM
(Redirected from ARDS)
Contents
Background
- Non-cardiogenic pulmonary edema due to lung capillary endothelial injury
- Proteinaceous material accumulate in alveoli in a heterogeneous manner
- Symptom of an underlying disease
Clinical Features
Diagnostic Criteria[1]
- New onset respiratory symptoms
- Bilateral pulmonary opacities
- Symptoms not explained by cardiac etiology or volume overload
Severity by Berlin Definition[1]
| PaO2/FiO2 | Severity | Mortality |
| 200-300 | Mild | 27% |
| 100-200 | Mod | 32% |
| <100 | Severe | 45% |
Presentation
- Severe dyspnea
- Hypoxemia
- Diffuse crackles
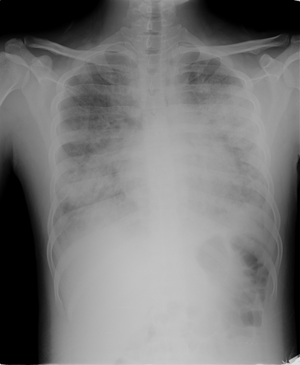
Imaging
- Diffuse patchy pulmonary infiltrates
Causes
- Sepsis
- Pancreatitis
- Burns
- Aspiration pneumonia and pneumonitis
- Trauma
- Near drowning
- Fat embolism syndrome
- Amniotic fluid embolism
- Overdose
- Massive transfusion
Differential Diagnosis
Pulmonary Edema Types
Cardiogenic pulmonary edema
Noncardiogenic pulmonary edema
- Negative pressure pulmonary edema
- Upper airway obstruction
- Reexpansion edema
- Neurogenic causes
- Iatrogenic fluid overload
- Multiple blood transfusions
- IV fluid
- Inhalation injury
- Pulmonary contusion
- Aspiration pneumonia and pneumonitis
- Other
Evaluation
- CXR
- CBC
- Chem 10
- Urinalysis
- LFT
- Lipase
- PT/PTT
- Influenza (seasonal)
- Blood cultures
- Lactate
- Consider bedside echo
- Consider ABG/VBG
- Consider BNP
Management
- Treat underlying cause
- Cover for sepsis
- Pneumonia in addition to other identified source
- Tamiflu 75mg BID oral or NGT if influenza season [2]
- Cover for sepsis
- Supplemental O2
- Noninvasive ventilation
- Limited data to support use
- Consider pulse dose steroids in early, established, severe ARDS in ICU setting[3]
- NOT for prevention of ARDS (will increase risk for ARDS and worsening sepsis if not in ARDS already)
- In theory, may reduce fibro-proliferative inflammatory changes during exudative phase (< 1 wk)
- No benefit to starting in late ARDS (> 2 wks)
- Meduri protocol (21 vs. 43% mortality)[4]
- 1mg/kg loading dose methyprednisolone
- Followed by infusion of 1mg/kg/day from day 1-14
- Then 0.5mg/kg/day from day 15-21
- Then 0.25mg/kg/day from day 22-25
- Finally 0.125mg/kg/day from day 26-28
- Ventilator Settings
- Permissive hypercapnia
- Tidal volume 6-8cc/kg of predicted body weight[5]
- Limit barotrauma to healthy area of lung
- Increase PEEP to improve oxygenation
- High FiO2 can cause absorptive atelectasis[6]
- Ardsnet PEEP/FiO2 protocol card[7]
- Maintain plateau pressures < 30 [8]
- Ensure adequate sedation
- Better synchrony with vent
- Decreased oxygen consumption
- Less delirium
- Increased patient comfort
- Prone ventilation [9]
- Increases survival for severe ARDS
- Consider for refractory hypoxemia
- Many consider this a type of recruitment maneuver
- APRV (BiVent) to recruit alveoli, if minimal to no respiratory acidosis[10][11]
- Start PHigh at PPlat at 28, try not to go beyond 35 cmH2O
- PPlateau = desired Pmean + 3 cmH2O
- PLow at 0 cmH2O for maximal expiration
- THigh at 4.5-6 seconds (inspiratory time)
- Tlow at 0.5-0.8 seconds (expiratory time), with TV 4-6 cc/kg
- Automatic tube compensation ON if patient spontaneously breathing[12]
- Full benefit of APRV is in patients that are not paralyzed that can provide spontaneous breaths
- Wean by "dropping and stretching"
- Every two hours or as tolerated, decrease PHigh by 1-2 cmH2O and increasing THight by 0.5 seconds per 1 cmH2O drop in PHigh
- Monitor for drop in SpO2, increased work of breathing, tachypnea
- Once PHigh reaches 10 cmH2O and THigh resaches 12-15 seconds with spontaneous respirations, change mode to CPAP with PEEP 10 cmH2O and PS 5-10 cmH2O, turn ATC off
- Pressure control ventilation (PCV) if acidosis with APRV
- Attempt to maintain same rate
- Maintain same Pmean
- PRVC or Volume control ventilation with paralysis to prevent barotrauma in breath stacking and vent dyssynchrony[13][14]
- Cisatricurium loading dose 0.15 mg/kg, followed by 1-3 mcg/kg/min
- Titrated to less than 2 twitches in train of four
- Cisatricurium preferred to pancuronium in renal impairment
- Cannot use paralysis with APRV
- Recruitment maneuver
- Varying methods and protocols
- Controversial in risks and benefits
Adjuncts
- Evidence of pulmonary hypertension
- ECMO
- Oscillation ventilation, High frequency oscillation ventilation (HFOV)
Disposition
- Admit to ICU
See Also
External Links
References
- ↑ 1.0 1.1 Ferguson ND et. al. The Berlin definition of ARDS: an expanded rationale, justification, and supplementary material. Intensive Care Med. 2012 Oct;38(10):1573-82.
- ↑ http://www.cdc.gov/flu/professionals/antivirals/summary-clinicians.htm
- ↑ Khilnani GC and Hadda V. Corticosteroids and ARDS: A review of treatment and prevention evidence. Lung India. 2011 Apr-Jun; 28(2): 114–119.
- ↑ Meduri GU, Golden E, Freire AX, Taylor E, Zaman M, Carson SJ, et al. Methylprednisolone infusion in early severe ARDS: Results of a randomized controlled trial. Chest. 2007;131:954–63.
- ↑ Brower RG, et al. "Ventilation With Lower Tidal Volumes As Compared With Traditional Tidal Volumes For Acute Lung Injury And The Acute Respiratory Distress Syndrome". The New England Journal of Medicine. 2000. 342(18):1301-1308.
- ↑ O'Brien J. Absorption Atelectasis: Incidence and Clinical Implications. AANA Journal. June 2013. Vol. 81, No. 3.
- ↑ Kallet RH, et al. "Respiratory controversies in the critical care setting. Do the NIH ARDS Clinical Trials Network PEEP/FIO2 tables provide the best evidence-based guide to balancing PEEP and FIO2 settings in adults?" Respiratory Care. 2007. 52(4):461-75.
- ↑ Hansen-Flaschen et al. Acute respiratory distress syndrome: Clinical features and diagnosis.UpToDate accessed 3/26/14
- ↑ Guerin, C. (2014) ‘Prone ventilation in acute respiratory distress syndrome’, European Respiratory Review, 23(132), pp. 249–257.
- ↑ CritCareMed. 2005;33:S228 Other Approaches to Open-Lung Ventilation–Airway Pressure Release Ventilation.
- ↑ CleveClinJMed 2011;78:101 Airway Pressure Release Ventilation–Alternative Mode of Mechanical Ventilation in Acute Respiratory Distress Syndrome.
- ↑ Guttmann J et al. Automatic tube compensation (ATC). Minerva Anestesiol. 2002 May;68(5):369-77.
- ↑ Gainnier M, Roch A, Forel JM, et al. Effect of neuromuscular blocking agents on gas exchange in patients presenting with acute respiratory distress syndrome. Crit Care Med. 2004;32:113-119.
- ↑ Papazian L, Forel JM, Gacouin A, et al. Neuromuscular blockers in early acute respiratory distress syndrome. N Engl J Med. 2010;363:1107-1116.