General Information
General Questions
What is Balamuthia?

Cyst of Balamuthia mandrillaris.
Balamuthia mandrillarisis a free-living ameba (a single-celled living organism) found in the environment. It is one of the causes of granulomatous amebic encephalitis (GAE), a serious infection of the brain and spinal cord 1,2,5,6. Balamuthia is thought to enter the body when soil containing Balamuthia comes in contact with skin wounds and cuts, or when dust containing Balamuthia is breathed in or gets in the mouth 1,2. The Balamuthia amebas can then travel to the brain through the blood stream and cause GAE 4. GAE is a very rare disease that is usually fatal.
Scientists at the Centers for Disease Control and Prevention (CDC) first discovered Balamuthia mandrillaris in 1986. The ameba was found in the brain of a dead mandrill baboon 2,7. After extensive research, B. mandrillaris was declared a new species of ameba in 1993 7. Since then, more than 200 cases of Balamuthia infection have been diagnosed worldwide, with at least 70 cases reported in the United States 2. Little is known at this time about how a person becomes infected 1, 3.
Where is Balamuthia found?
How do you get a Balamuthia infection and how is it spread?
Balamuthia infection is not spread from person to person.
Balamuthia is thought to enter the body when soil containing Balamuthia comes in contact with skin wounds and cuts, or when dust containing Balamuthia is breathed in or gets in the mouth 1,2. Once inside the body, the amebas can travel through the blood stream to the brain, where they cause GAE 1,5,6. There are also a few reports of dogs that might have become infected after swimming in ponds 7.
Balamuthia infection can occur at any time of year 7.
What are the symptoms of a Balamuthia infection?
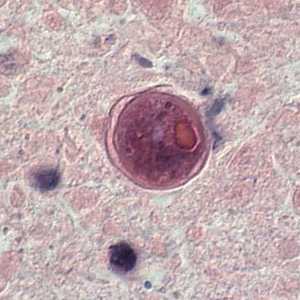
Cyst of Balamuthia mandrillaris in brain tissue.
The symptoms of Balamuthia infection can begin with a skin wound on the face, chest, torso, arms, or legs. If the infection involves the brain, the disease it causes is called granulomatous amebic encephalitis (GAE) 5,6. Diagnosis of Balamuthia GAE can be difficult, but some early symptoms might include:
- Headaches
- Stiff neck or head and neck pain with neck movement
- Sensitivity to light
- Nausea
- Vomiting
- Lethargy (tiredness)
- Low-grade fever
Other signs of Balamuthia GAE might include:
- Behavioral changes
- Seizures
- Weight loss
- Partial paralysis
- Difficulty speaking in full sentences
- Difficulty walking
The disease might appear mild at first but can become more severe over weeks to several months 6,7. Often the disease is fatal 7, with a death rate of more than 89% 1. Overall, the outlook for people who get this disease is poor, although early diagnosis and treatment may increase the chances for survival 1.
How long after infection do symptoms appear?
How long will symptoms last?
GAE is chronic and symptoms develop over a period of several weeks to as long as 2 years. Although Balamuthia GAE is often fatal 2, there are several recorded cases of Balamuthia infection where the patients survived after long-term treatment with multiple drugs 3,6. In some of those cases, the patients were able to return to normal, functioning lives 1,2.
Who is most likely to get a Balamuthia infection?
What should I do if I think I may have a Balamuthia infection?
Contact your healthcare provider as soon as possible if you think you may have a Balamuthia infection.
How is a Balamuthia infection diagnosed?
What is the treatment for a Balamuthia infection?
Currently, treatment recommendations include the use of a combination of several drugs. Most cases of Balamuthia are diagnosed right before death or after the patient has died 3,6,7. This delay in diagnosis limits the amount of experience doctors have using different drugs to treat Balamuthia infection 1. Current treatment plans are based on lab studies of the ameba and the few cases where the patients have survived.
Should I be worried about getting Balamuthia from others?
No. There have been no reports of a Balamuthia infection spreading from one person to another except through organ donation/transplantation.
How can I prevent a Balamuthia infection?
Currently, there are no known ways to prevent infection with Balamuthia since it is unclear how and why some people become infected while others do not. Research is currently underway to learn more about Balamuthia in hopes of finding ways to prevent future infections.
References
- Siddiqui R, Khan NA. Balamuthia amoebic encephalitis: an emerging disease with fatal consequences. Microb Pathog. 2008;44(2):89-97.
- Perez MT, Bush LM. Balamuthia mandrillaris amebic encephalitis. Curr Infect Dis Rep. 2007;9(4):323-8.
- Schuster FL, Glaser C, Honarmand S, Maguire JH, Visvesvara GS. Balamuthia amebic encephalitis risk, Hispanic-Americans. Emerg Infect Dis. 2004;10(8):1510-12.
- Huang ZH, Ferrante A, Carter RF. Serum antibodies to Balamuthia mandrillaris, a free-living amoeba recently demonstrated to cause granulomatous amoebic encephalitis. J Infect Dis. 1999;179(5):1305-8.
- Maciver SK. The threat from Balamuthia mandrillaris. J Med Microbiol. 2007;56(Pt 1):1-3.
- Perez MT, Bush LM. Fatal amebic encephalitis caused by Balamuthia mandrillaris in an immunocompetent host: a clinicopathological review of pathogenic free-living amebae in human hosts. Ann Diagn Pathol. 2007;11(6):440-7.
- Visvesvara GS, Moura H, Schuster FL. Pathogenic and opportunistic free-living amoebae: Acanthamoeba spp. , Balamuthia mandrillaris, Naegleria fowleri, and Sappinia diploidea. FEMS Immunol Med Microbiol. 2007;50(1):1-26.
- CDC. Balamuthia amebic encephalitis–California, 1999-2007. MMWR Morb Mortal Wkly Rep. 2008;57(28):768-71.
- Schuster FL, Visvesvara GS. Free-living amoebae as opportunistic and non-opportunistic pathogens of humans and animals. Int J Parasitol. 2004;34(9):1001-27.
- Schuster FL, Visvesvara GS. Opportunistic amoebae: challenges in prophylaxis and treatment. Drug Resist Updat. 2004;7(1):41-51.
- Martinez DY, Seas C, Bravo F, Legua P, Ramos C, Cabello AM, Gotuzzo E. Successful treatment of Balamuthia mandrillaris amoebic infection with extensive neurological and cutaneous involvement. Clin Infect Dis. 2010;51(2):e7-11.
- Page last reviewed: February 17, 2016
- Page last updated: February 17, 2016
- Content source:


 ShareCompartir
ShareCompartir
