U.S. Trends and Outbreaks
U.S. Trends
Each year on average in the United States, norovirus—
- causes 19–21 million cases of acute gastroenteritis (inflammation of the stomach or intestines or both)
- leads to 1.7–1.9 million outpatient visits and 400,000 emergency department visits, primarily in young children
- contributes to about 56,000–71,000 hospitalizations and 570-800 deaths, mostly among young children and the elderly
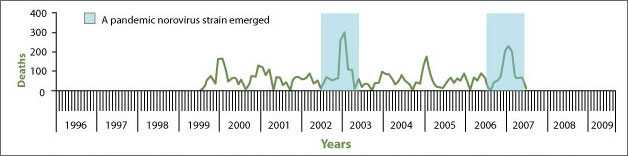
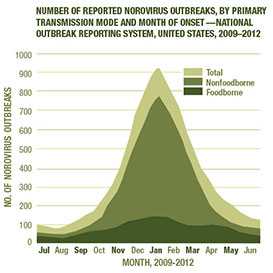
You can get norovirus illness at any time during the year. But, it is most common in the winter. Also, there can be 50% more norovirus illness in years when there is a new strain of the virus going around.
Norovirus-associated Deaths
See also:
Outbreaks
 Most outbreaks of norovirus illness happen when infected people spread the virus to others. But, norovirus can also spread by consuming contaminated food or water and touching things that have the virus on them.
Most outbreaks of norovirus illness happen when infected people spread the virus to others. But, norovirus can also spread by consuming contaminated food or water and touching things that have the virus on them.
Norovirus is the leading cause of illness and outbreaks from contaminated food in the United States. About 50% of all outbreaks of food-related illness are caused by norovirus. Food can get contaminated with norovirus at any point when it is being grown, shipped, handled, or prepared.
Foods that are commonly involved in outbreaks of norovirus illness are—
- leafy greens (such as lettuce),
- fresh fruits, and
- shellfish (such as oysters).
But, any food that is served raw or handled after being cooked can get contaminated.
 To search for foodborne outbreaks caused by norovirus, go to the Foodborne Outbreak Online Database (FOOD).
To search for foodborne outbreaks caused by norovirus, go to the Foodborne Outbreak Online Database (FOOD).
Common Norovirus Outbreak Settings
Norovirus in Healthcare Facilities
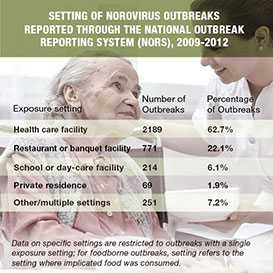
Health care facilities, including nursing homes and hospitals, are the most commonly reported settings for norovirus outbreaks in the United States and other industrialized countries (see Norovirus in Healthcare Settings). Over half of all norovirus outbreaks reported in the United States occur in long-term care facilities.
The virus can be introduced into healthcare facilities by infected patients—who may or may not be showing symptoms—or by staff, visitors, or contaminated foods. Outbreaks in these settings can be quite long, sometimes lasting months. Illness can be more severe, occasionally even fatal, in hospitalized or nursing home patients compared with otherwise healthy people.
Norovirus in Restaurants and Catered Events
Most norovirus outbreaks from contaminated food occur in food service settings like restaurants. Infected food workers are frequently the source of these outbreaks, often by touching ready-to-eat foods, such as raw fruits and vegetables, with their bare hands before serving them. (See For Food Workers: Norovirus and Working with Food.) Foodborne outbreaks of norovirus illness have also occurred in banquet halls, and even at family dinners, where people eat food handled or prepared by others.
Norovirus outbreaks can also occur from fecal (stool) contamination of certain foods at their source. For example, oysters harvested from contaminated water and raspberries irrigated with contaminated water have caused norovirus outbreaks.
Norovirus on Cruise Ships
Over 90% of diarrheal disease outbreaks on cruise ships are caused by norovirus (see Facts about Noroviruses on Cruise Ships). Norovirus can be especially challenging to control on cruises ships because of the close living quarters, shared dining areas, and rapid turnover of passengers. When the ship docks, norovirus can be brought on board in contaminated food or water or by passengers who were infected while ashore. Repeated outbreaks on consecutive cruises may also result from infected crew or environmental contamination. This is because norovirus can persist on surfaces and is resistant to many common disinfectants.
Norovirus in Schools and Other Institutional Settings
Norovirus outbreaks occur in a range of other institutional settings, for example, schools, child care centers, colleges, prisons, and military encampments. Norovirus outbreaks on university campuses have led to campus closures. Norovirus was the most common cause of gastroenteritis in U.S. Marines during Operation Iraqi Freedom and a common cause of outbreaks among British troops deployed to Iraq during 2002 to 2007.
Norovirus outbreaks have also been caused by contaminated water from sewage in wells and in recreational water settings, such as pools and lakes.
Learn More about Norovirus
- Overview
- Symptoms
- Transmission
- Prevention
- Treatment
- Norovirus and Working With Food
- Norovirus Worldwide
Resources for Public Health Practitioners
- Updated Norovirus Outbreak Management and Disease Prevention Guidelines (2011)
- Guideline for the Prevention and Control of Norovirus Gastroenteritis Outbreaks in Healthcare Settings (2011)
- A Norovirus Outbreak Control Resource Toolkit for Healthcare Settings (2012)
- Surveillance Summaries for Waterborne Disease and Outbreaks
For more information, see the "For Public Health Professionals" section of this Web site.
- Page last reviewed: June 24, 2016
- Page last updated: December 10, 2015
- Content source:


 ShareCompartir
ShareCompartir