module list
ELEMENTS OF ERGONOMICS PROGRAMS
Step 3: Collect Health and Medical Evidence
Now that you have identified the signs of a potential work-related musculoskeletal disorders (WMSD) problem and trained your staff, your next step is to determine the scope and characteristics of the problem by collecting health and medical evidence of WMSDs. It is essential to follow up on workers whose jobs cause undue physical fatigue, stress, or discomfort. If employees report their symptoms early and openly, you can take corrective measures to delay the development of musculoskeletal disorder (MSDs). In a scenario where workers in a certain department report more MSD problems than workers in other departments, it is best to immediately study possible MSD risk factors in that department.
Compute the incidence rate (IR) and prevalence rate (PR) of MSDs

Begin your review from the date of your last equipment or process change. Gather information on the extent of WMSDs from OSHA logs of work-related injuries and illnesses, company medical records, workers’ compensation claims, insurance claims, absentee records, and job transfer applications.
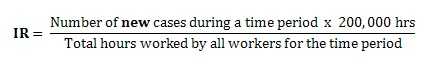
You can calculate incidence rates based on the number of new cases reported and the total hours worked in a calendar year. Incidence rates for partial years can be calculated using hours worked through the time period in question. Incident rates are typically computed for the Total Recordable Cases incidents (TRC rate includes both cases with and without lost workdays) and for those cases with only Days Away, Restricted days or Transferred to another job (DART). When the total hours worked by all workers is not available, an estimate of 2,000 hours per year for each full time worker can be used. Compare incidence rates to those of other departments, other industries, other occupations, or the nation using The U.S. Bureau of Labor Statistics.
The incidence rate equation is calculated by the number of new cases per 100 worker years (which is equivalent to 200,000 work hours.
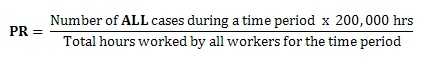
A prevalence rate is calculated when considering all active cases in a given time period regardless of when the case originated.
Conduct interviews and symptom surveys

Use interviews and symptom surveys to identify the onset and nature of possible WMSDs that might otherwise go unnoticed. Surveys ask for the usual background information (age, sex, occupational history, present job tile, etc.) along with the nature, onset, location, timing, duration, and severity of MSD symptoms. Surveys also inquire about symptoms at previous jobs, the difficulty of job tasks, and medical history. You may include a body map so that workers can illustrate their discomfort. Administer surveys that are anonymous, voluntary, and to be completed on work time only. Rank-order the frequency and severity of complaints for each body part, then average this data for each department and/or job. Out of respect for workers’ personal information, use surveys only if the company is prepared to act on the results.
Provide periodic medical exams

Gather evidence of WMSDs from periodic medical exams designed and administered by a health care provider. Workers give their medical history and complete a physical exam. Health care providers may also ask workers to complete range of motion tests, tenderness tests, etc. and report if they feel any pain. Physicians conducting medical exams should have no prior knowledge of workers’ existing diseases or job titles. WMSDs are present when MSDs in a certain part of the body are associated with a particular job function. Incidence rates and prevalence rates of MSDs are confirmed and specified by interviews, symptom surveys, and medical exams. For example, cashiers have more WMSDs in their hands and wrists than other supermarket workers, and those who perform more/longer checkout tasks have the most MSD problems.
Conduct job analyses

Brannick, Levine, & Morgeson (2007) define job analysis as the study of a job and all of its components. The tasks of any job can be described in terms of tools, equipment, materials, workstation layout, physical environment, job demands, or organizational climate. A human resources professional or other experienced personnel conducts a job analysis to be able to describe everything that happens on the job. There is no standard protocol for conducting a job analysis to assess MSD hazards, so you may want to follow these objectives:
- Obtain a complete description of the job, including the time needed to complete each task.
- Ask employees if the way their job is done has changed over time.
- Divide the job into tasks and actions.
- Count and categorize the risk factors in each task and action. Consider work postures, workstation layouts, work surface heights, and reach distances. With work surfaces, consider slip resistance, hardness, and surface edges. Also consider the sizes, weights, and vibration of tools that workers use.
- Determine the underlying cause for risk factors in each task and action. Don’t forget to consider whole body vibrations and other demands of the physical working environment. You can use biomechanics to measure muscle force and spinal disc pressure, physiological tests to measure oxygen consumption and heart rate, or psychological tests to measure perceived exertion.
- Record the severity, frequency, and duration of each risk factor.
It may be difficult to determine what level or amount of exposure is harmful to your workers. NIOSH uses a variety of approaches to determine the appropriate job analysis for each workplace situation. You can use the NIOSH Lifting Equation to assess the risks associated with lifting and lowering tasks. You can compare the muscle strength required to perform a task to the strength of the individual workers performing this task. You can ask your workers to determine what they consider acceptable working conditions.
Current assessment tools can be found on the Washington State Department of Labor & Industries, Ohio Bureau of Workers’ Compensation, Ergonomics – Thomas E. Bernard, Cornell University Ergonomics Web, AIHA Ergonomic Assessment toolkit and AIHA Flowchart to aide selection of an ergonomic assessment tool:
Table 3.1 Assessment Tools
| Whole Body & Screening | |
|---|---|
| Bureau of Workers’ Compensation CTD Risk Factor Identification Form | What it is: A checklist that focuses on the upper extremity, back & legs, and environmental job settings (e.g. lighting) Why we use it: To determine concerning elements in a job task |
| Bureau of Workers’ Compensation CTD Risk Factor Measurement Form | What it is: A table that focuses on the upper extremity, back and legs, and environmental job settings Why we use it: To determine task areas with high risk levels |
| Quick Exposure Check (QEC) | What it is: Tables and multiple steps that focus on back, shoulder/arm, wrist/hand, and neck Why we use it: To determine low, moderate, high, or very high exposure levels |
| Rapid Entire Body Assessment (REBA) | What it is: Tables and multiple steps that focus on the neck, trunk, legs, and arm & wrist positions Why we use it: To determine negligible, low, medium, high or very high risk levels |
| Rodgers Muscle Fatigue Assessment | What it is: A table that focuses on neck, shoulders, back, arms/elbows, wrists/hands/fingers, legs/knees, & ankles/feet/toes by task effort, duration, and frequency Why we use it: To determine if your range of muscle fatigue puts you at risk for WMSDs. If you meet a light, moderate, heavy, or very heavy risk level, you should modify the task accordingly. |
| Whole Body Vibration | What it is: A table based on the ISO 2631 standard that focuses on the upper and lower extremities. Why we use it: To determine the level and risk created by your task |
| Washington State WISHA Screening Tool | What it is: A checklist that focuses on low back, hand & wrist, neck & shoulder, and knee Why we use it: To determine the range of risk created by your task (i.e. none, caution, or hazard) |
| Back | |
| ACGIH TLV for Lifting | What it is: A checklist that focuses on the concern and risk for the back. It looks at the position of the object, and frequency and duration of the lift. Why we use it: The results are compared to a given standard to determine the action level. |
| Liberty Mutual Manual Material Handling Tables | What it is: Tables that focus on push/pull, carrying, and lift/lowering. Why we use it: To determine the percentile of men and women that this task would be acceptable to. |
| Revised NIOSH Lifting Equation | What it is: An equation designed to assess manual lifting that focuses on the back. It looks at the object’s weight, horizontal and vertical position, twisting angle, duration, frequency and coupling. Why we use it: To determine an acceptable weight for that task. |
| Utah Back Compressive Force | What it is: A table and equations that focus on back posture, load moment and direct compression. Why we use it: The results are compared to a given standard to determine if more detailed analysis or changes are needed to the task. |
| WISHA Lifting Analysis | What it is: A combined checklist and multiple steps for manual lifting that focus on the back. It factors in an object’s weight, and the frequency and posture of the task. Why we use it: The results are compared to a given standard to determine if the task is a WMSD hazard. |
| Upper Body | |
| ACGIH TLV for Hand Activity Level | What it is: A table that focuses on each hand’s activity level and estimated normalized peak force. Why we use it: The results are compared to an action limit and threshold limit value to evaluate the risk level. |
| ACGIH TLV Hand Arm (Segmental) Vibration | What it is: A table based on the ANSI/ASA S2.70-2006 standard that focuses on hand arm vibration. Why we use it: To determine the level and risk of exposure to vibration. |
| Moore-Garg Strain Index | What it is: A table that focuses on each hand. It looks at 6 different risk factors. Why we use it: To determine the range of risk created by your task (i.e. safe, uncertain, some risk, or hazardous risk) |
| Rapid Upper Limb Assessment (RULA) | What it is: Tables and multiple steps that focus on the neck, arm and wrist positions. Why we use it: To determine the range of risk created by your task (i.e. an acceptable task, further investigation, or implement changes) |
| WISHA Hand-Arm Vibration Analysis | What it is: A combined checklist and graph that focus on hand-arm vibration hazards. Why we use it: To determine the range of risk created by your task (i.e. okay, caution, or hazard) |
For Additional Assessment Tools:
- Page last reviewed: July 19, 2017
- Page last updated: July 19, 2017
- Content source:
- National Institute for Occupational Safety and Health Division of Applied Research and Technology


 ShareCompartir
ShareCompartir