NCEZID: Fighting Antibiotic Resistance
Each year in the United States, at least 2 million people become infected with bacteria that are resistant to antibiotics. Antibiotic resistance (AR) is the ability of microbes to resist the effects of drugs—that is, the germs are not killed, and their growth is not stopped. At least 23,000 people die each year as a direct result of these infections. Although some people are at greater risk than others, no one can completely avoid the risk of antibiotic-resistant infections. Infections with resistant organisms are difficult to treat, requiring costly and sometimes toxic alternatives. Some of the current trends in resistance:
- Antibiotics are among the most commonly prescribed drugs used in human medicine, but up to 50% of the time antibiotics are not prescribed properly (for example, often given when not needed or with incorrect drug dosing or duration).
- The germs that contaminate food can become resistant because of the use of antibiotics in food animals as well as people. Studies have shown that the use of antibiotics in food animals can lead to resistant infections, like those caused by Salmonella and Campylobacter in people.
- The other major factor in the alarming growth of antibiotic resistance is spread of resistant strains of bacteria from person to person, or from contaminated sources in the environment.
What we’re doing
In 2016, Congress appropriated $160 million for CDC to fight antibiotic resistance. With this investment, NCEZID is working with others to detect, respond, contain, and prevent resistant infections. Some key activities include:
- Investing in states and communities across the US for better response, containment, and prevention of AR threats.
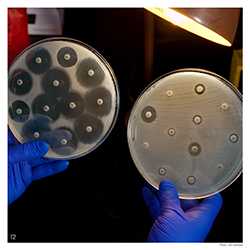
- Establishing the AR Lab Network made up of CDC labs, 7 regional labs in health departments, and expanded capacity of all state and local health department labs. The new lab network will conduct nationwide testing to fill data gaps and inform how we respond to some of the most serious antibiotic- resistant threats like the nightmare bacteria CRE (carbapenem-resistant Enterobacteriaceae), gonorrhea, and Salmonella.
- Funding innovation to understand how antibiotics disrupt a healthy microbiome, the community of naturally occurring microbes in and on our bodies.
We are in a post-antibiotic era where doctors and patients are faced with untreatable infections.
- Page last reviewed: August 28, 2017
- Page last updated: August 28, 2017
- Content source:
Centers for Disease Control and Prevention
National Center for Emerging and Zoonotic Infectious Diseases (NCEZID)


 ShareCompartir
ShareCompartir