Treatment
My Child Has Been Diagnosed with ADHD – Now What?
When their child is diagnosed with ADHD, parents often have concerns about deciding the best way to help their child. It is important for parents to remember that ADHD can be successfully managed. There are many treatment options, so parents should work closely with everyone involved in the child’s life—healthcare providers, therapists, teachers, coaches, and other family members. Taking advantage of all the resources available will help parents guide their child towards success.
This page provides you with information about treatment options for ADHD:
- Behavior therapy, including training for parents
- Medications
- School accommodations and interventions
For children 6 years of age and older, the American Academy of Pediatrics (AAP) recommends both behavior therapy and medication as good options, preferably both together. For young children (under 6 years of age) with ADHD, behavior therapy is recommended as the first line of treatment, before medication is tried. Good treatment plans will include close monitoring of whether and how much the treatment helps the child’s behavior, and making changes as needed along the way. To learn more about the AAP recommendations for treatment of children with ADHD, visit the Recommendations page.
Behavior Therapy, Including Training for Parents
What is behavior therapy?
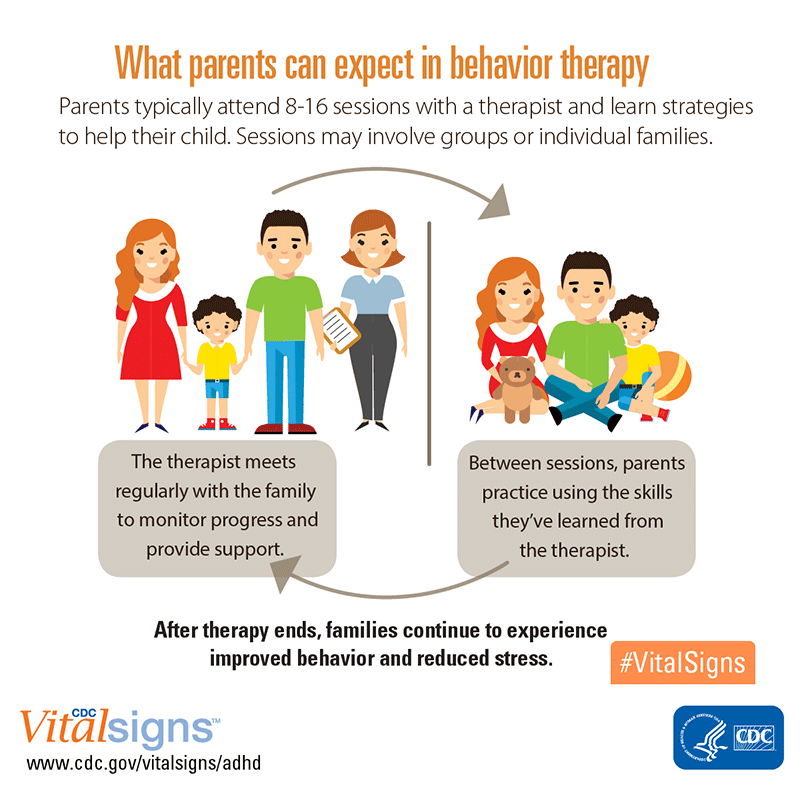
Research shows that behavior therapy is an important part of treatment for children with ADHD. ADHD affects not only a child’s ability to pay attention or sit still at school, it also affects relationships with family and other children. Children with ADHD often show behaviors that can be very disruptive to others. Behavior therapy is a treatment option that can help reduce these behaviors. It is often helpful to start behavior therapy as soon as a diagnosis is made.
The goals of behavior therapy are to learn or strengthen positive behaviors and eliminate unwanted or problem behaviors. Behavior therapy can include behavior therapy training for parents, behavior therapy with children, or a combination. Teachers can also use behavior therapy to help reduce problem behaviors in the classroom.
- In parent training in behavior therapy, parents learn new skills or strengthen their existing skills to teach and guide their children and to manage their behavior. Parent training in behavior therapy has been shown to strengthen the relationship between the parent and child, and to decrease children’s negative or problem behaviors. Parent training in behavior therapy is also known as behavior management training for parents, parent behavior therapy, behavioral parent training, or just parent training.
- In behavior therapy with children, the therapist works with the child to learn new behaviors to replace behaviors that don’t work or cause problems. The therapist may also help the child learn to express feelings in ways that do not create problems for the child or other people.
Behavior therapy for young children: Training for parents
The 2011 clinical practice guidelines from the American Academy of Pediatrics (AAP) recommend that doctors prescribe behavior therapy as the first line of treatment for preschool-aged children (4–5 years of age) with ADHD. Parent training in behavior therapy has the most evidence of being effective, but teachers and early childhood caregivers can use behavior therapy in the classroom as well.
Why should parents try behavior therapy first, before medication?
Behavior therapy is an important first step because:
- Behavior therapy gives parents the skills and strategies to help their child.
- Behavior therapy has been shown to work as well as medication for ADHD in young children.
- Young children have more side effects from ADHD medications than older children.
- The long-term effects of ADHD medications on young children have not been well-studied.
The Agency for Health Care Research and Quality (AHRQ) conducted a review in 2010 of all existing studies on treatment options for children younger than 6 years of age. The review found enough evidence to recommend parent training in behavior therapy as a good treatment option for children under 6 with ADHD symptoms and for disruptive behavior, in general.
The review also identified four programs for parents of young children with ADHD that reduced symptoms and problem behaviors related to ADHD:
- Triple P (Positive Parenting Program),
- Incredible Years Parenting Program
- Parent-Child Interaction Therapy
- New Forest Parenting Programme — Developed specifically for parents of children with ADHD
Read a summary of the AHRQ report here.
More recently, another intervention, Helping the Non-Compliant Child, was shown to be effective for young children with ADHD1. Other programs that help parents strengthen parent-child relationships and manage negative behavior with positive discipline may also be effective.
Learn more about behavior therapy here.
Overview for parents
Behavior therapy for school-age children and adolescents
For children over the age of 6, behavior therapy is an important part of treatment. The AAP recommends behavior therapy together with medication. The type of therapy that is effective for young children, parent training in behavior therapy, may also be effective for children with disruptive behavior through age 12.3
Research evidence points to the effectiveness of several types of behavior therapies for older children:
- Parent training in behavior therapy
- Classroom behavior management
- Peer interventions that focus on behavior
- Organizational skills training
- Combinations of behavior treatments
Read about effective therapies here.
Medications
Medication can help children with ADHD in their everyday life, and medication treatment may be an effective way to manage ADHD symptoms. Medication is an option that may help control some of the behavior problems that have led to trouble in the past with family, friends and at school.
Several different types of medications are FDA-approved to treat ADHD in children:
- Stimulants are the best-known and most widely used ADHD medications. Between 70-80 percent of children with ADHD have fewer ADHD symptoms when they take these fast-acting medications.
- Nonstimulants were approved for treating ADHD in 2003. Nonstimulants do not work as quickly as stimulants, but they can last up to 24 hours.
- Medications can affect children differently. One child may respond well to one medication, but not another. The doctor may need to try different medications and doses, so it is important for parents to work with their child’s doctor to find the medication that works best for their child.
For more information on treatments, please click one of the following links:
National Resource Center on ADHD
National Institute of Mental Health
Parent Education and Support
CDC funds the National Resource Center on ADHD (NRC), a program of Children and Adults with Attention Deficit/Hyperactivity Disorder (CHADD) The NRC provides resources, information, and advice for parents on how to help their child. Learn more about their services here.
ADHD and the Classroom

The symptoms of ADHD, inability to pay attention, difficulty sitting still, difficulty controlling impulses, can make it particularly hard for children with ADHD to do well in school. It is important for teachers to have the needed skills to help children manage their ADHD. However, since the majority of children with ADHD are not enrolled in special education classes, their teachers will most likely be regular education teachers who might know very little about ADHD and could benefit from assistance and guidance. The National Resource Center on ADHD provides information for teachers on how to help students with ADHD.
Here are some tips to share with teachers for classroom success:
- Make assignments clear – check with the student to see if they understood what they need to do
- Give positive reinforcement and attention to positive behavior
- Make sure assignments are not long and repetitive. Shorter assignments that provide a little challenge without being too hard are best.
- Allow time for movement and exercise
- Communicate with parents on a regular basis
- Use a homework folder to limit the number of things the child has to track
- Be sensitive to self-esteem issues
- Minimize distractions in the classroom
- Involve the school counselor or psychologist
What Every Parent Should Know…
Children with ADHD might be eligible for special services or accommodations at school under the Individuals with Disabilities in Education Act (IDEA) and an anti-discrimination law known as Section 504. The U.S. Department of Education has developed a resource guide to help educators, families, students, and other stakeholders better understand how these laws apply to students with ADHD so that they can get the services and education they need to be successful.
Learn more about education services and accommodations.
Learn more about how to help a child with attention and learning issues.
Healthcare providers can play an important part in collaborating with schools to help the child get the special services they need. Read more about the role of healthcare providers in assisting children with special needs.
Tips for Parents
Following are examples that might help with your child’s behavior:
- Create a routine. Try to follow the same schedule every day, from wake-up time to bedtime.
- Get organized. Encourage your child to put schoolbags, clothing, and toys in the same place every day so your child will be less likely to lose them.
- Manage distractions. Turn off the TV, limit noise, and provide a clean workspace when your child is doing homework. Some children with ADHD learn well if they are moving, or listening to background music. Watch your child and see what works.
- Limit choices. Offer choices between a few things so that your child doesn’t get overwhelmed and overstimulated. For example, offer choices between a few options, such as this outfit or that one, this meal or that one, or this toy or that one.
- Be clear and specific when you talk with your child. Let your child know you are listening by describing what you heard them say. Use clear, brief directions when they need to do something.
- Help your child plan. Break down complicated tasks into simpler, shorter steps. For long tasks, starting early and taking breaks may help limit stress.
- Use goals and praise or other rewards. Use a chart to list goals and track positive behaviors, then let your child know they have done well by telling your child or rewarding efforts in other ways. Be sure the goals are realistic—baby steps are important!
- Discipline effectively. Instead of yelling or spanking, use timeouts or removal of privileges as consequences for inappropriate behavior.
- Create positive opportunities. Children with ADHD may find certain situations stressful. Finding out and encouraging what your child does well — whether it’s school, sports, art, music, or play — can help create positive experiences.
- Provide a healthy lifestyle. Nutritious food, lots of physical activity, and sufficient sleep are important; they can help keep ADHD symptoms from getting worse.
ADHD in Adults
ADHD lasts into adulthood for at least one-third of children with ADHD2. Treatments for adults can include medication, psychotherapy, education or training, or a combination of treatments. For more information about diagnosis and treatment throughout the lifespan, please visit the websites of the National Resource Center on ADHD and the National Institutes of Mental Health.
References:
- Abikoff, H.B., Thompson, M., Laver-Bradbury, C., Long, N., Forehand, R. L., Miller Brotman, L., et al. (2015). Parent training for preschool ADHD: a randomized controlled trial of specialized and generic programs. Journal of Child Psychology and Psychiatry, 56, 618-31.
- Barbaresi, W. J., Colligan, R. C., Weaver, A. L., Voigt, R. G., Killian, J. M., & Katusic, S. K. (2013). Mortality, ADHD, and psychosocial adversity in adults with childhood ADHD: a prospective study. Pediatrics, 131(4), 637-644.
- McCart, M. R., Priester, P. E., Davies, W. H., & Azen, R. (2006). Differential effectiveness of behavioral parent-training and cognitive-behavioral therapy for antisocial youth: A meta-analysis. Journal of Abnormal Child Psychology, 34, 527-543. doi:10.1007/s10802-006-9031-1
- Page last reviewed: May 31, 2017
- Page last updated: May 31, 2017
- Content source:


 ShareCompartir
ShareCompartir