Depression
Overview
Depression is a serious medical illness and an important public health issue. Depression is characterized by persistent sadness and sometimes irritability (particularly in children) and is one of the leading causes of disease or injury worldwide for both men and women. Depression can cause suffering for depressed individuals and can also have negative effects on their families and the communities in which they live. The economic burden of depression, including workplace costs, direct costs and suicide- related costs, was estimated to be $210.5 billion in 2010.1
Depression is associated with significant healthcare needs, school problems, loss of work, and earlier mortality.
Depression…
- Is associated with an increased risk for mortality from suicide as well as other causes, such as heart disease
- Is associated with lower workplace productivity and more absenteeism, which result in lower income and higher unemployment.
- Is associated with higher risk for other conditions and behaviors, including:
- Other mental disorders (anxiety disorders, substance use disorders, eating disorders)
- Smoking
Depression can occur at any time over a person’s life. Follow the links below to learn about depression and different life stages.
Although effective treatments are available, many individuals with depression do not have access to treatment or do not take advantage of services. If not effectively treated, depression is likely to become a chronic disease. Just experiencing one episode of depression places an individual at a 50% risk for experiencing another episode, and further increases the chances of having more depression episodes in the future.
Public health surveillance systems measure the prevalence and impact of depression providing valuable information that can be used to guide mental health promotion, mental illness prevention, and treatment programs.
Diagnostic Criteria
According to the American Psychiatric Association’s diagnostic criteria for Major Depressive Disorder, a person must experience five or more symptoms below for a continuous period of at least two weeks.2
- Feelings of sadness, hopelessness, depressed mood
- Loss of interest or pleasure in activities that used to be enjoyable
- Change in weight or appetite (either increase or decrease)
- Change in activity: psychomotor agitation (being more active than usual) or psychomotor retardation (being less active than usual)
- Insomnia (difficulty sleeping) or sleeping too much
- Feeling tired or not having any energy
- Feelings of guilt or worthlessness
- Difficulties concentrating and paying attention
- Thoughts of death or suicide.
Most symptoms must be present every day or nearly every day and must cause significant distress or problems in daily life functioning.
For more information about depression or where you can go to find help, please visit MentalHealth.gov.
Depression Statistics
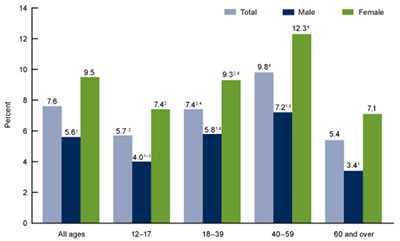
- More than 1 out of 20 Americans 12 years of age and older reported current depression (moderate or severe depressive symptoms in the past 2 weeks) in 2009-2012. (Figure at right.)
- Among Americans 12 years of age and over, a greater percentage of females reported depression than females. Almost 10% of adults aged 40-59 reported current depression.
Major Reports and Publications
- CDC. Mental illness surveillance among adults in the United States. MMWR 2011
- CDC. Mental health surveillance among children — United States, 2005–2011. MMWR
- Pratt LA, Brody DJ. Depression in the U.S. household population, 2009–2012 . NCHS data brief, no 172. Hyattsville, MD: National Center for Health Statistics. 2014.
- Other Featured Publications
Surveillance Data Sources for Depression
Behavioral Risk Factor Surveillance System (BRFSS)
The BRFSS is an annual state-based telephone survey of the U.S. civilian, non-institutionalized adult population. The core questionnaire contains questions asked of all respondents, while states may choose to also include optional modules addressing various topics. The core questionnaire asks about whether a person has been diagnosed with depression. An optional Anxiety and Depression Module assesses the prevalence of anxiety and depressive disorders in the general population at the state level. This module is composed of the Patient Health Questionnaire (PHQ-8) which has been validated against the diagnostic criteria for a depressive disorder in the Diagnostic and Statistical Manual for Mental Disorders (DSM-IV).
- For more information on BRFSS
National Health and Nutrition Examination Survey (NHANES)
NHANES is a program of studies designed to assess the health and nutritional status of adults and children in the U. S., which is conducted in 2-year cycles. The survey is unique in that it combines interviews and physical examinations. A depression screener has been administered during a computer-assisted personal interview as part of NHANES since 2005.
During 2000–2004, NHANES assessed major depression and dysthymia during the past 12 months using parent and child report using the Diagnostic Interview Schedule for Children (DISC-IV). Currently, NHANES uses self-reported symptoms drawn from the Patient Health Questionnaire (PHQ-9) to assess depression during the past 2 weeks among adolescents aged 12–17 years.
- For more information on NHANES.
National Survey of Children’s Health (NSCH)
The NSCH is a cross-sectional national (50 states and DC) telephone survey of parents in households with at least one child aged 0 to 17 years at the time of the interview. Parents report on their children’s health. To assess for depression, parents are asked: “Has a doctor or other health care provider ever told you that [CHILD] had depression.” If “yes” parents were asked “Does [CHILD] currently have depression?” and if yes, parents were asked to rate current depression as mild, moderate or severe.
- For more information on NSCH.
National Survey of Drug Use and Health (NSDUH)
The NSDUH is sponsored by SAMHSA and uses a series of questions asked through an audio computer-assisted self-interviewing (ACASI) household interview to assess whether adolescents have experienced a major depressive episode, based on DSM criteria and is measured for the lifetime and past year.
- More on NSDUH.
Pregnancy Risk Assessment Monitoring System (PRAMS)
PRAMS is a state-based, cross-sectional survey of women who have recently delivered a live-born infant. The survey provides population-based data that can be used to develop maternal and infant health programs and policies. Data are collected in 37 states and New York City and represent approximately 75% of the births in the U. S. PRAMS provides estimates of postpartum depression by using two questions similar to those included in the Patient Health Questionnaire (PHQ-8): 1) “Since your new baby was born, how often have you felt down, depressed, or hopeless?” and 2) “Since your new baby was born, how often have you had little interest in doing things?” Possible responses are “never,” “rarely,” “sometimes,” “often,” and “always.”
- For more information on PRAMS.
Youth Risk Behavior Survey (YRBS)
The national Youth Risk Behavior Survey (YRBS) was developed to monitor health-risk behaviors that contribute substantially to the leading causes of death, disability, and social problems among children and young adults in the United States. YRBS uses a three-stage cluster sample design to produce a representative sample of public and private high school students in grades 9–12 in the 50 states and DC. YRBS questionnaires are self-administered; students record their responses on a computer-scannable booklet or answer sheet. One symptom of depression, feeling sad or hopeless, is assessed by the question: "During the past 12 months, did you ever feel so sad or hopeless almost every day for 2 weeks or more in a row that you stopped doing some usual activities?"
- For more information on YRBS.
Behaviors and Conditions Associated with Depression
In addition to the many symptoms associated with depression, depression is associated with several chronic and other diseases as well as with factors that increase risk for those diseases. In many cases, it is difficult to determine whether depression is the result of a behavior or condition, or whether depression causes (or contributes to) the behavior or condition. Depression may also affect whether individuals follow the treatments for diagnosed conditions as recommended by their healthcare providers. Follow the links below to learn more about selected behaviors and conditions associated with depression.
References
1. Greenberg PE, Fournier AA, Sisitsky T, Pike CT, Kessler RC. The economic burden of adults with major depressive disorder in the United States (2005 and 2010). J Clin Psychiatry. 2015 Feb;76(2):155-62.
2. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5). 5th ed. Washington, DC: American Psychiatric Publishing; 2013.
- Page last reviewed: March 30, 2016
- Page last updated: March 30, 2016
- Content source:


 ShareCompartir
ShareCompartir