The Microbiome & Innovations to Slow Antibiotic Resistance
The AR Solutions Initiative provides critical support to combat AR. Use the Antibiotic Resistance Investment Map to learn how CDC is collaborating with investigators in your area to find and implement new ways to prevent antibiotic-resistant infections and their spread.
As part of its continued efforts to protect patients and slow antibiotic resistance, CDC is investing in research to discover and develop new ways to prevent antibiotic-resistant infections and their spread, as well as unlock the mysteries of the microbiome. These efforts support CDC’s Antibiotic Resistance Solutions Initiative and implement the tracking, prevention, and antibiotic stewardship activities outlined in the National Action Plan for Combating Antibiotic-Resistant Bacteria [63 pages]
Applied Microbiome Research to Improve Public Health
CDC is expanding its work in the microbiome to slow antibiotic resistance.
The microbiome is a community of naturally-occurring germs in and on our bodies. Bacteria live naturally on our skin, in our gut, in our mouths or respiratory tracts, and in our urinary tracts.
Antibiotics impact the microbiome by wiping out or disrupting the natural composition of both good and bad bacteria. With a disrupted microbiome, resistant bacteria can take over (or colonize) and the body is less able to defend against infection, putting people at risk for potentially untreatable illnesses.
Microbiomes disrupted by antibiotics are vulnerable to infections by tough-to-kill germs such as Methicillin-resistant Staphylococcus aureus (MRSA), Carbapenem-resistant Enterobacteriaceae (CRE), Clostridium difficile (C. difficile), and E. coli. These patients can carry drug-resistant bacteria and can easily spread bacteria to other people, especially those who also have a disrupted microbiome.
Antibiotics are life-saving medicines, but they also change, unbalance, and disrupt your microbiome. This change could put people at risk for drug resistant infections.
CDC is conducting applied research on the microbiome to identify effective public health approaches that protect people, their microbiomes, and the effectiveness of antibiotics. CDC is investing in research and collaborating with investigators to determine:
- How Antibiotics Disrupt a Healthy Microbiome – CDC and investigators will study novel strategies that can protect and restore the microbiome, and determine how exposure to antibiotics early in life affects microbiome development.
- How a Disrupted Microbiome Puts People at Risk – CDC and investigators will develop a predictive index that identifies a patient’s risk of disruption from a specific antibiotic, to carry antibiotic-resistant bacteria, or become infected with one. CDC and investigators will also work to develop and test microbiome measurements that monitor a patient’s risk for disruption, and assess enhanced infection control triggers.
- How Antibiotic Stewardship Can Protect the Microbiome – CDC and investigators will improve strategies to tailor antibiotic stewardship to a patient’s individual microbiome, as well as assess how to fit antibiotic stewardship to a specific population of patients (e.g., hospital unit, nursing home, doctor’s office).
See a more extensive list of AR Solutions Initiative projects, including those related to the microbiome, below.
Innovations to Track & Prevent Antibiotic-Resistant Infections
To combat antibiotic resistance effectively, CDC is working to better understand antibiotic-resistant infections found across healthcare and the community—like drug-resistant healthcare-associated infections and foodborne infections. CDC and investigators will create innovative prevention and tracking strategies to protect people from these infections and stop spread.
See a more extensive list of AR Solutions Initiative research investigations, including innovative prevention and tracking across healthcare and the community, below.
Research Topics
Microbiome Assessment & Intervention
Brown University
Rectal microbiome disruption indices associated with acquisition of multidrug-resistant organism among subjects exposed to antimicrobials
The goal of this study is to identify characteristics of the microbiome, that can predict which patients are at highest risk of acquiring multidrug-resistant organisms. This information may be helpful for future efforts to develop novel strategies that can prevent people from acquiring drug-resistant bacteria.
Cornell University
Surveillance of resistance gene carriage in patients with hematologic malignancies: A taxonomy-focused approach
Understanding the transfer of antibiotic resistance genes in Leukemia patients and what role the microbiome is playing.
Georgia Institute of Technology
Optimization of therapeutic strategies to manage polymicrobial Cystic Fibrosis lung infections
The project aims to reduce the risk of dangerous lung infections in patients with cystic fibrosis, by determining what protective alterations can be made to their microbiome.
OpenBiome
Randomized controlled trial of autologous microbiome reconstitution to prevent colonization by antibiotic resistant bacteria
Study in which stool will be collected from patients before they go to nursing homes. Then the stool will be re-administered to them after they receive antibiotics, to restore their microbiomes and prevent drug resistant infection.
Synthetic Biologics
A longitudinal assessment of the resistome amongst patients treated with IV Ceftriaxone +/- SYN-004 (ribaxamase), an oral β-lactamase designed to be administered with intraxvenous β-lactam antibiotics and prevent exposure of gut bacteria to selective antibiotic pressure
This project will explore how selective pressure in the form of intravenous-administered ceftriaxone excreted into the gastrointestinal (GI) tract may lead to the emergence of antibiotic resistance in the gut microbiome, and whether specific intervention from SYN-004 (ribaxamase), the company’s clinical-stage beta-lactamase designed to protect the gut microbiome, may prevent the emergence of antibiotic-resistant organisms in the gut microbiome.
University of Cincinnati
Metagenomic shotgun sequencing to detect colonization, invasion, and transmission of multidrug-resistant organisms
Investigators at Cincinnati Children’s Hospital will use new methods to analyze the microbiome to precisely monitor colonization, infection, and transmission of multi-drug resistant bacteria.
University of Michigan
Longitudinal impact of prophylactic antibiotic use on the gut microbiota in health human populations
The study will try to determine how the microbiome of surgery patients are impacted by antibiotics used before, during, and after orthopedic surgery.
University of Michigan
Detection and prognosis of colonization by Extended-Spectrum Beta-lactamase producing Enterobacteriaceae
Development of a molecular assay to detect colonization and domination of the microbiome with extended spectrum Beta-Lactamase (ESBL)- producing bacteria.
University of Pennsylvania
Stool microbiome features to discriminate Clostridium difficile (C. difficile) colonization and infection
The study will apply microbiome analysis to define stool bacterial community types in patients who are colonized or infected with C. difficile, in order to better understand non-C. difficile microbes, with the hope of improving our ability to diagnose, treat, and prevent C.difficile infection.
University of Pennsylvania
Respiratory tract microbiome composition and risk for antibiotic-resistant lower respiratory infection during long-term acute care
The study will comprehensively characterize respiratory tract microbiome composition and change, during the course of prolonged mechanical ventilation in order to define bacterial community features associated with hazard for lower respiratory tract infection, particularly lower respiratory tract infection due to antibiotic-resistant pathogens.
Washington University
Enduring effects of early life antibiotic therapy on microbiota development and antibiotic resistance gene carriage in the preterm infant gut
To research the long-term effects of early-life antibiotic therapy on microbiota development and how that affects the mobility of antibiotic-resistances genes in the preterm infant gut.
Washington University
Prospective study characterizing fecal microbiome disruptions during and after receipt of antimicrobials
To characterize the extent and duration of microbiome disruptions observed during and after usual courses of antimicrobials used to treat community-acquired pneumonia.
Washington University
Intestinal metabolomic factors affecting Clostridium difficile colonization and infection
To lead a group of clinicians, chemists and mathematicians to identify how diet, metabolism and intestinal microbes interact to protect against C. difficile infection.
Yale University
Identification of microbial disruption indices (MDI) predictive of colonization by multidrug resistant Pseudomonas aeruginosa
Tracking the microbiome of ICU patients over time, to predict risk of infection of multi-drug-resistant Pseudomonas.
Innovations to Track & Prevent AR across Healthcare & the Community
Emory University
Evaluating the use of an Adenosine Triphosphate (ATP) Bioluminescence assay to optimize hospital cleaning
The study will evaluate the use of a new technology to measure and thereby optimize hospital room cleaning.
Columbia University School of Nursing
Barriers and facilitators for NHSN adoption in nursing homes
The Columbia University School of Nursing will conduct a national study to determine the barriers of nursing homes to tracking C. difficile and multidrug-resistant organisms (MDROs) using CDC’s National Healthcare Safety Network (NHSN), and what resources are needed to overcome these barriers.
Ohio State University
Preventing the dissemination of Carbapenem-resistant Enterobacteriaceae (CRE) from healthcare facilities into surface waters in the U.S.
The study will evaluate potential discharge of antibiotic resistance bacteria from hospital sewage and test a technology to prevent it.
OpenBiome
A randomized controlled trial of encapsulated fecal microbiota for vancomycin-resistant enterococcus decolonization
A study of fecal microbiota transplantation administered as a capsule to decolonize patients with vancomycin-resistant enterococcus (VRE).
Pennsylvania State University
Doctor-patient communication
Studying doctor-patient communication in acute care visits, including communications that may include educating patients about antibiotics.
Rutgers University
A comprehensive study of multidrug resistance determinants and drivers in the major fungal pathogen Candida glabrata
A study to better define the genetic mechanisms and drivers fueling the emergence of drug-resistant fungal infections, and validate a new diagnostic platform to rapidly identify resistant strains of Candida glabratra in the clinic and community.
Rutgers University
Unlocking the microbial ecology of environmental antibiotic resistance
This project targets adapting molecular tools to improve understanding of the role of microbial communities in antibiotic resistance in the environment.
The Joint Commission
Challenges and facilitators to standardized measurement of infections related to Clostridium difficile and multi-drug resistant organisms (MDROs) in nursing homes: A prospective, multisite study
This project will identify challenges and facilitators to implementing standardized measurement of C.difficile and other multidrug-resistant organism events in nursing homes.
University of California Berkley
Resistance and genetics of community acquired foodborne urinary tract infections
The project will study the role of retail food as a potential source of multidrug-resistant E. coli that cause community-acquired urinary tract infections among college-age women.
University of California, Davis
A multifaceted intervention to improve prescribing for acute respiratory infection
Project evaluating behavioral approaches, audit and feedback, and peer-to-peer comparisons to reduce unnecessary antibiotic prescribing among physicians for adult and pediatric patients who come to emergency departments and urgent-care centers with respiratory infections.
University of Colorado
UTIDecide: improving antibiotic stewardship in long term care through the UTIDecide electronic clinical decision support
Studying the use of an electronic clinician decision support tool to improve antibiotic use for urinary tract infections in nursing home patients.
University of Georgia
Nitric oxide releasing ultra-low fouling antibacterial intravascular catheters
Researchers in the University Of Georgia College Of Engineering will be developing next-generation coatings to combat antibiotic-resistant bacteria in medical devices.
University of Maryland School of Medicine
Implementation of a Clostridium difficile Infection Reduction Bundle in Acute Care Hospitals: Feasibility and Pilot to Guide a Multicenter Stepped Wedge Cluster Trial
A project to implement and assess a prevention bundle for C.difficile infection in acute care hospitals.
University of Michigan
Genomic insights into the origin and spread of antibiotic resistance in nursing homes
Project seeks to apply genome sequencing to understand how antibiotic resistance spreads within and between healthcare facilities.
University of Michigan
Patient Hand Hygiene Initiative
Studying how improving hand hygiene of patients could prevent them from becoming colonized or infected with drug resistant bacteria.
University of Oregon
Preventing spread of CRE among veterans through an automated tracking system.
An effort to develop and use a CRE patient registry in the Veterans Affairs hospital system.
University of Pennsylvania
Targeted reduction of antimicrobials for prevention of Clostridium difficile Infection (TRAP-CDI)
The study aims to compare the effectiveness of two antimicrobial use strategies for prevention of C. difficile infection in the hospital setting and to better understand the attitudes, social norms and beliefs of healthcare providers about C.difficile infection and antimicrobial stewardship.
University of Utah
Impact of human and food animal wastes on antimicrobial gene abundance and E. coli susceptibility patterns: a watershed approach
The use of advanced genetic analyses to investigate how the spread of antibiotic-resistant genes in a river system is influenced by discharges of antimicrobials and human and animal wastes.
University of Virginia
Assessing the risk of acquisition of carbapenemase producing Enterobacteriaceae (CPE) from exposure to contaminated waste water premise plumbing
Use of geospatial modeling and whole genome sequencing to understand the role of the hospital environment in transmission of antibiotic-resistant bacteria.
Virginia Commonwealth University
Development of NHSN’s AUR data and SAAR to support antibiotic benchmarking program among Vizient members
This project will identify how to create and deliver antibiotic use data reports to hospitals. It will identify aspects of compelling reports that best help hospitals address inappropriate prescription practices.
AR Solutions Initiative: Microbiome Factsheet
Download Infographic [PDF – 1 MB]
Infographic Details
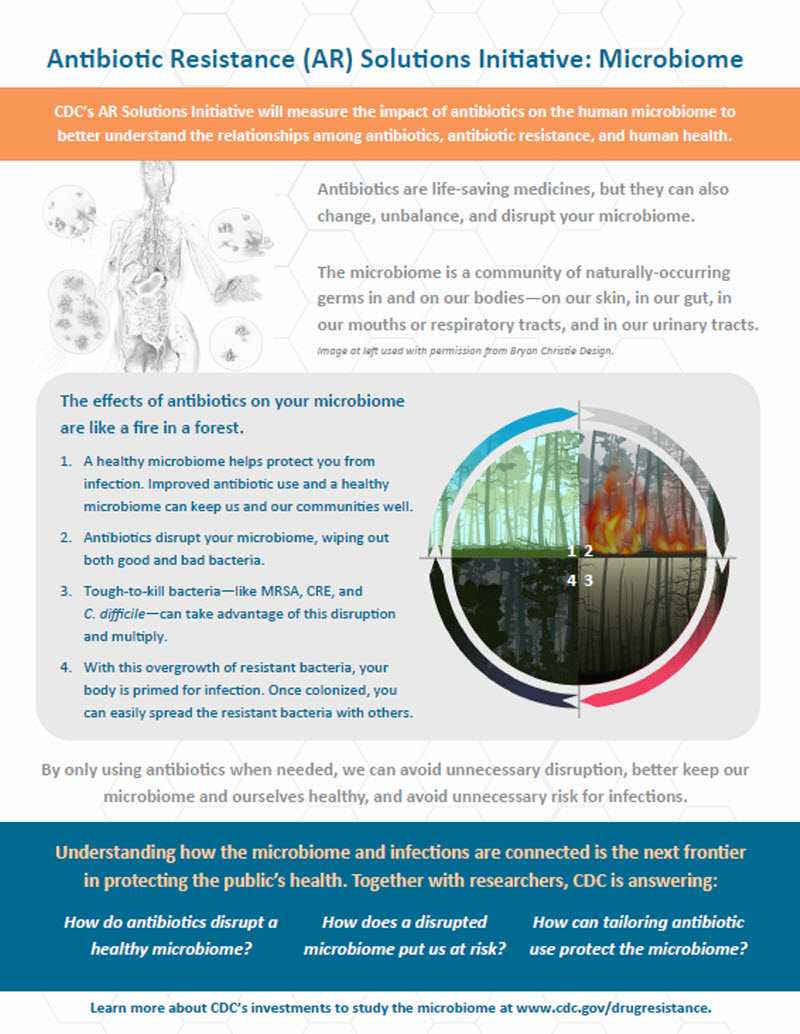
Antibiotic Resistance (AR) Solutions Initiative: Microbiome
CDC’s AR Solutions Initiative will measure the impact of antibiotics on the human microbiome to better understand the relationships among antibiotics, antibiotic resistance, and human health
Antibiotics are life-saving medicines, but they can also change, unbalance, and disrupt your microbiome.
The microbiome is a community of naturally-occurring germs in and on our bodies—on our skin, in our gut, in our mouths or respiratory tracts, and in our urinary tracts.
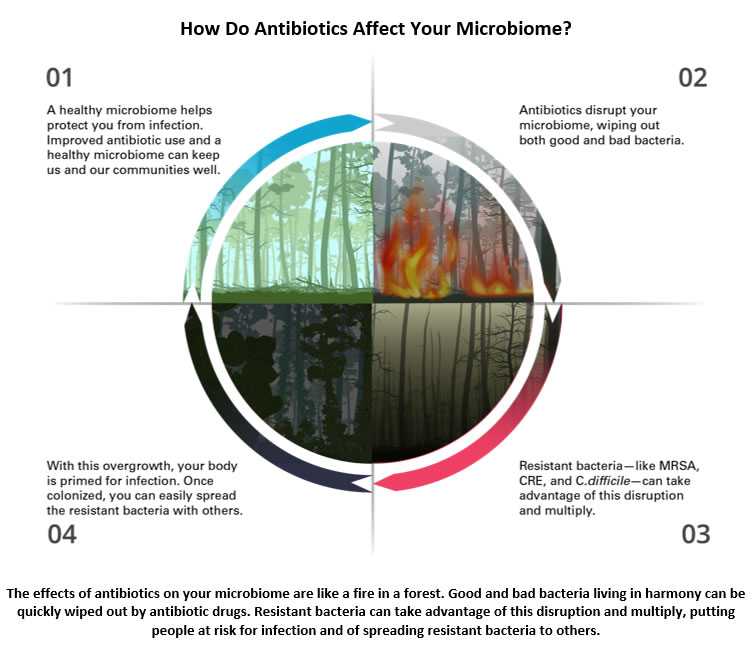
The effects of antibiotics on your microbiome are like a fire in a forest.
- A healthy microbiome helps protect you from infection. Improved antibiotic use and a healthy microbiome can keep us and our communities well.
- Antibiotics disrupt your microbiome, wiping out both good and bad bacteria.
- Tough-to-kill bacteria—like MRSA, CRE, and C. difficile—can take advantage of this disruption and multiply.
- With this overgrowth of resistant bacteria, your body is primed for infection. Once colonized, you can easily spread the resistant bacteria with others.
By only using antibiotics when needed, we can avoid unnecessary disruption, better keep our microbiome and ourselves healthy, and avoid unnecessary risk for infections.
Understanding how the microbiome and infections are connected is the next frontier in protecting the public’s health. Together with researchers, CDC is answering:
- How do antibiotics disrupt a healthy microbiome?
- How does a disrupted microbiome put us at risk?
- How can tailoring antibiotic use protect the microbiome?
Learn more about CDC’s investments to study the microbiome at www.cdc.gov/drugresistance.
Top of Page
- Page last reviewed: February 1, 2017
- Page last updated: May 10, 2017
- Content source:


 ShareCompartir
ShareCompartir
