CDC’s Role
On this Page
Top 10 2016 Accomplishments Report
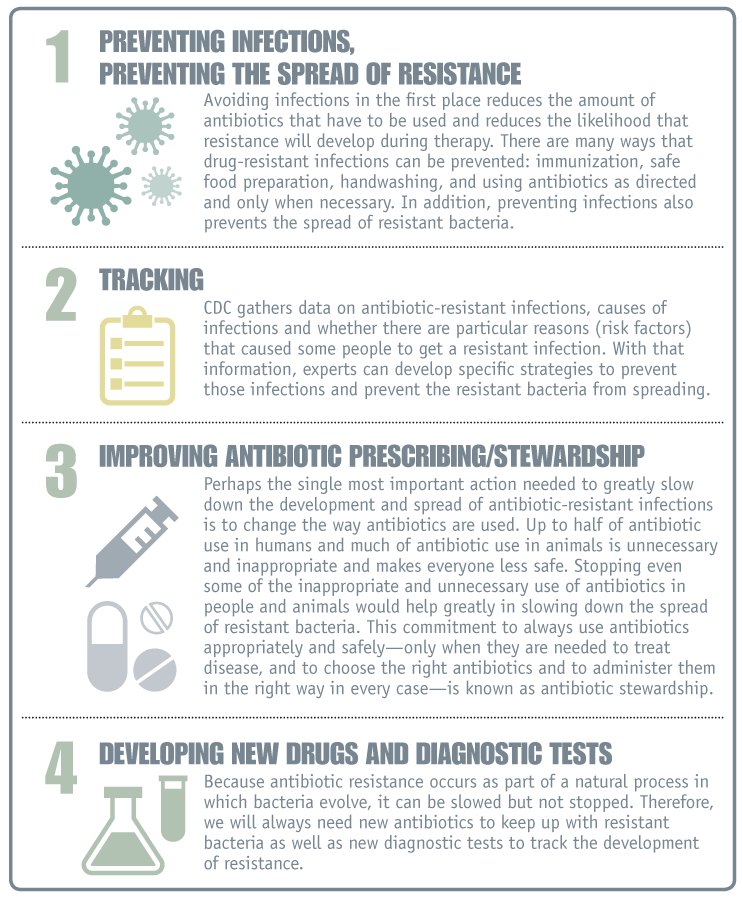
Bacteria will inevitably find ways of becoming resistant to existing and new antibiotics, which is why aggressive action is needed now to keep new resistance from developing and to prevent the resistance that already exists from spreading. CDC serves as a national resource for putting into practice the four core actions recommended to prevent antibiotic resistance.
1. Preventing Infections, Preventing the Spread of Resistance
Preventing infections from developing reduces the amount of antibiotics used. This reduction in antibiotic use, in turn, slows the pace of antibiotic resistance. Preventing infections also prevents the spread of resistant bacteria. CDC works to prevent antibiotic-resistant infections in healthcare settings, in the community, and in food.
Healthcare Settings
CDC works to prevent antibiotic resistance in healthcare settings by providing a system to track resistance and prescribing patterns at national, regional, and local levels; providing guidance to healthcare facilities through infection control guidelines, assistance implementing these guidelines, and laboratory expertise.
-
Tracking
- CDC’s National Healthcare Safety Network (NHSN) [https://www.cdc.gov/nhsn/] is used by healthcare facilities to electronically report infections, antibiotic use, and resistance.
- CDC’s specialized, national reference laboratory tests bacteria samples from around the country to detect new and emerging resistance patterns that affect patient health.
-
Improving Antibiotic Prescribing
- CDC manages the Get Smart Programs [https://www.cdc.gov/getsmart/], a national effort to improve antibiotic prescribing and use in both outpatient and inpatient settings.
-
Protecting Patients from Infections
- To help prevent infections, CDC conducts research to find new ways of preventing infections; provides the nation with infection prevention guidelines and tools to prevent infections; serves as the nation’s reference laboratory to identify microorganisms; and offers the nation’s largest healthcare-associated infection tracking system, NHSN, allowing facilities and states to identify and address problem areas.
Community
CDC works to prevent antibiotic resistance in the community by providing systems to track infections and changes in resistance; working with partners to improve prescribing at national, regional, and local levels; and limiting or interrupting the spread of infections.
-
Tracking
- Active Bacterial Core surveillance (ABCs) [https://www.cdc.gov/abcs/index.html]: Tracking infections caused by Neisseria meningitidis, Streptococcus pneumoniae, Groups A and B Streptococcus, and Methicillin-resistant Staphylococcus aureus.
- Gonococcal Isolate Surveillance Project (GISP) [https://www.cdc.gov/std/gisp/default.htm]: Collecting isolates from gonorrhea infections to monitor antibiotic resistance.
- National Tuberculosis Surveillance System (NTSS) [https://www.cdc.gov/tb/statistics/default.htm]: National Electronic Disease Surveillance System (NEDSS)-based reporting of tuberculosis cases including resistance data.
- Healthcare-Associated Infections-Community Interface (HAIC): Tracking infections with C. difficile and with multidrug-resistant gram-negative microorganisms.
-
Improving Antibiotic Prescribing
- CDC manages the Get Smart Programs [https://www.cdc.gov/getsmart/], a national effort to improve antibiotic prescribing and use in both outpatient and inpatient settings.
-
Limiting and Interrupting the Spread of Infections
- Contact Tracing: A prevention strategy that has proven successful is tracking cases (individuals who are infected) and tracking contacts (people who have had contact with a case that puts them at risk for infection as well). This process is used to ensure that all persons requiring an intervention such as treatment, prophylaxis or temporary isolation from the general public are identified and managed appropriately.
- Vaccination: There are few vaccines for antibiotic-resistant bacteria, but the S. pneumoniae vaccine has proven that an effective vaccine can reduce antibiotic resistance rates. The vaccine targets certain types of the bacteria, even if tis a resistant type, and reduces the overall number of infections, including those that are caused by resistant strains.
- Treatment Guidelines: The spread of antibiotic resistance can be prevented if infections are effectively treated before the pathogen is spread to others. For some infections, laboratory tests for guiding treatment are not easily available or the turn-around time is slow or incomplete. This is the case for treating gonorrhea [https://www.cdc.gov/std/Gonorrhea/treatment.htm] and tuberculosis. For these infections, healthcare providers rely on treatment guidelines for proper management of infections. CDC monitors resistance trends in Neisseria gonorrhoeae (the cause of gonorrhea) and Mycobacterium tuberculosis (the case of tuberculosis) and publishes treatment guidelines to limit the progression of these diseases and the spread of bacteria.
- Promotion of Safe Sex: Increases in the spread of drug-resistant Neisseria gonorrhoeae poses unique challenges. To prevent transmission of this infection, CDC works to promote safer sexual behaviors such as abstinence, mutual monogamy, and correct and consistent condom use.
Food
To prevent antibiotic-resistant foodborne infections, CDC works closely with state and local health departments; with the U.S. Food and Drug Administration (FDA), which regulates antibiotics, many foods, animal feed, and other products; and with the U.S. Department of Agriculture (USDA), which regulates meat, poultry, and egg products.
-
Tracking
- National Antimicrobial Resistance Monitoring System (NARMS): Tracks antibiotic resistance among Salmonella, Campylobacter, and other bacteria transmitted commonly through food.
- Estimating how much foodborne illness occurs.
- Monitoring tends in foodborne infections.
- Attributing illnesses to specific foods and settings.
- Tracking and responding to changes in resistance.
- Determining the sources of antibiotic-resistant enteric infections.
-
Improving Antibiotic Use
- The use of antibiotics in food-producing animals contributes to the emergence of antibiotic-resistant bacteria in these animals. CDC encourages and supports efforts [PDF – 18 pages] to minimize inappropriate use of antibiotics in animals.
Preventing Infections
-
- Investigating outbreaks and sporadic cases of foodborne illness to stop outbreaks and improve prevention.
- Educating consumers and food workers about safe food handling practices.
- Identifying and educating groups at high risk for infection.
- Promoting proper handwashing.
- Strengthening the capacity of state and local health departments to detect, respond to, and report foodborne infections.
- Developing better diagnostic tools to rapidly and accurately find sources of contamination.
- Providing recommendations for travelers on safe food and clean water.
2. Tracking Resistance Patterns
CDC gathers data on antibiotic-resistant infections, causes of infections, and whether there are particular reasons (risk factors) that caused some people to get a resistant infection. With that information, experts develop specific strategies to prevent those infections and prevent the resistant bacteria from spreading.
| CDC’s Antibiotic Resistance and Antibiotic-Resistant Infections Tracking Platform
|
||
|---|---|---|
| Tracking Networks | Data Collected | ResistantBacteria/Fungus3 |
|
EIP
|
A network of public health-academichospital The three main programs within EIP
|
ABCs: Streptococcus pneumoniae Groups A and B Streptococcus Methicillin-resistant Staphylococcus aureus HAIC: C. difficile Candida (a fungus) Carbapenem-R Enterobacteriaceae MDR Acinetobacter FoodNet: (see NARMS list) |
| NARMS National Antimicrobial Resistance Monitoring System |
A national public health surveillance system that tracks changes in the susceptibility of foodborne and other enteric bacteria to antibiotics of human and veterinary medical importance NARMS is a collaboration among CDC, FDA, USDA, and state and local health departments CDC tests bacterial isolates from humans, while FDA and USDA test isolates from retail meats and food animals. |
Salmonella
Campylobacter Shigella |
| NHSN National Healthcare Safety Network |
A system that collects and provides data on infections and drug-resistance in healthcare settings. Since NHSN collects data directly from healthcare facilities, it can provide facility-level information on healthcare-associated infections and antibiotic resistance (and in the future, on antibiotic use). |
Staphylococcus aureus
Enterococcus Enterobacteriaceae Acinetobacter Pseudomonas aeruginosa Candida (a fungus) |
| GISP Gonococcal Isolate Surveillance Program |
A program to track antibiotic resistance data for gonococcal isolates. Isolates are collected from sexually transmitted disease clinics in approximately 28 cities. |
Neisseria gonorrhoeae |
| NTSS National Tuberculosis Surveillance System |
National Electronic Disease Surveillance System (NEDSS)-based reporting of tuberculosis cases including resistance data. Public health departments from 50 states and the US territories contribute data. |
Mycobacterium tuberculosis |
3ABCs also includes surveillance for Neisseria meningitidis and Haemophilus influenzae. NARMS also includes surveillance for
E. coli O157 and Vibrio (non-V. cholerae).
3. Antibiotic Stewardship: Improving Prescribing and Use
Antibiotics are a limited and exhaustible resource. The more that antibiotics are used today, the less likely they will still be effective in the future. Therefore, doctors and other health professionals around the world are increasingly adopting the principles of responsible antibiotic use, often called antibiotic stewardship. Stewardship is a commitment to always use antibiotics only when they are necessary to treat, and in some cases prevent, disease; to choose the right antibiotics; and to administer them in the right way in every case. Effective stewardship ensures that every patient gets the maximum benefit from the antibiotics, avoids unnecessary harm from allergic reactions and side effects, and helps preserve the life-saving potential of these drugs for the future. Efforts to improve the responsible use of antibiotics have not only demonstrated these benefits but have also been shown to improve outcomes and save healthcare facilities money in pharmacy costs.
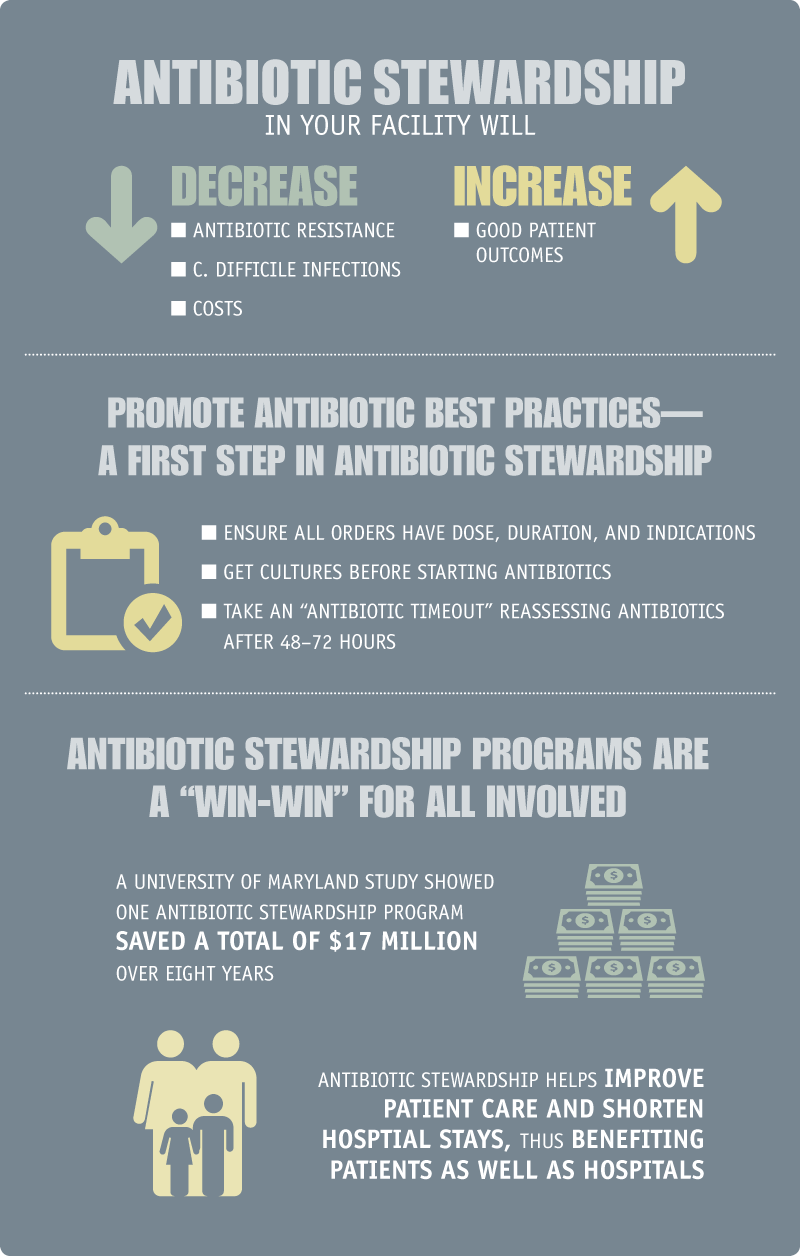
Click here to enlarge image [PDF – 1 page]
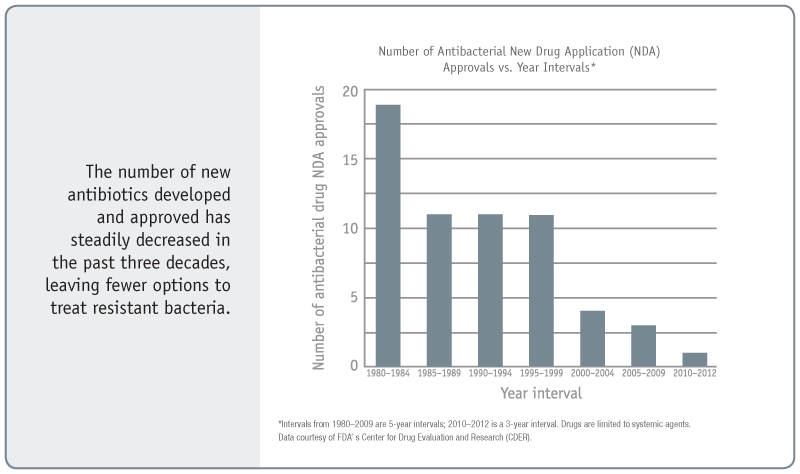
4. Developing New Antibiotics and Diagnostic Tests
Because antibiotic resistance occurs as a part of a natural evolution process, it can be significantly slowed but not stopped. Therefore, new antibiotics will always be needed to keep up with resistant bacteria as well as new diagnostic tests to track the development of resistance.
- Page last reviewed: July 19, 2010
- Page last updated: March 8, 2017
- Content source:


 ShareCompartir
ShareCompartir