Improving Antibiotic Prescribing with Rapid Diagnostics and Education
Story Highlights
- CDC estimates about 80 percent of patients with Valley fever are given one or more rounds of antibiotics to kill bacteria before they receive a proper diagnosis or treatment.
- These types of antibiotics do not cure Valley fever because it is caused by fungus, not bacteria.
- Through CDC’s Antibiotic Resistance Solutions Initiative, the agency is taking new approaches to improve antibiotic use and prescribing.
- CDC is working to help healthcare providers better diagnose Valley fever, in part by supporting development of rapid diagnostic tests. These tests can quickly provide clinicians with the information they need to appropriately treat patients.
Most types of pneumonia, or lung infections, are caused by bacteria, so people with pneumonia often receive antibiotics that kill bacteria. But when a person has pneumonia caused by a fungus, as in Valley fever, these types of antibiotics will not work!
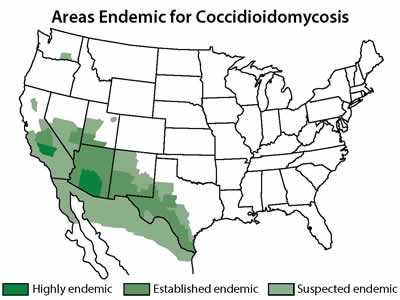
Map showing the approximate areas where the fungus that causes Valley fever is known to live or suspected to live.
Taking antibiotics that are not helpful can put people at risk for a negative drug reaction and can kill healthy bacteria in the gut, allowing more harmful bacteria, such as Clostridium difficile (or C. difficile), to grow in its place. Through the Antibiotic Resistance Solutions Initiative, CDC is taking new approaches to improve antibiotic use and prescribing.
CDC estimates about 80 percent of patients with Valley fever are given one or more rounds of antibiotics before receiving a correct diagnosis of Valley fever and appropriate treatment. However, Valley fever is only one example of how improved diagnosis and prescribing can help protect patients. CDC estimates that at least 30 percent of antibiotics prescribed in the outpatient setting are unnecessary, meaning that no antibiotic was needed at all.
Anyone living in or traveling to areas where the Valley fever fungus (called Coccidioides) is in the environment can get the disease. About 10,000 cases of Valley fever are reported every year, but tens of thousands more illnesses are likely to occur. In areas where Valley fever is common, like parts of California and the U.S. Southwest, the fungus can cause up to one in three cases of community-acquired pneumonia. However, many patients are not tested for Valley fever, so their illnesses may be misdiagnosed.
Transformative Investments
CDC is making transformative improvements nationwide to combat AR using resources provided by Congress in fiscal year 2016. To improve outpatient prescribing, CDC is:
- Expanding antibiotic use education for both providers and patients.
- Encouraging outpatient clinicians and facilities to use the Core Elements for Antibiotic Stewardship for Outpatient Settings.
- Working with partners to explore the expansion of physician quality measures.
- Collaborating with academic partners to scale up and test interventions to improve outpatient prescribing.
Early testing for Valley fever reduces unnecessary antibiotic use and allows for appropriate treatment, which may include antifungal medicine. However, only laboratory tests can identify Valley fever. CDC is working to improve awareness about Valley fever and supporting the development of rapid diagnostic tests. A rapid diagnostic test for Valley fever would provide clinicians the tool they need to quickly diagnose patients, get them the correct treatment, and prevent the use of unneeded antibiotics.
Learn more:
- Page last reviewed: April 6, 2017
- Page last updated: May 4, 2017
- Content source:


 ShareCompartir
ShareCompartir