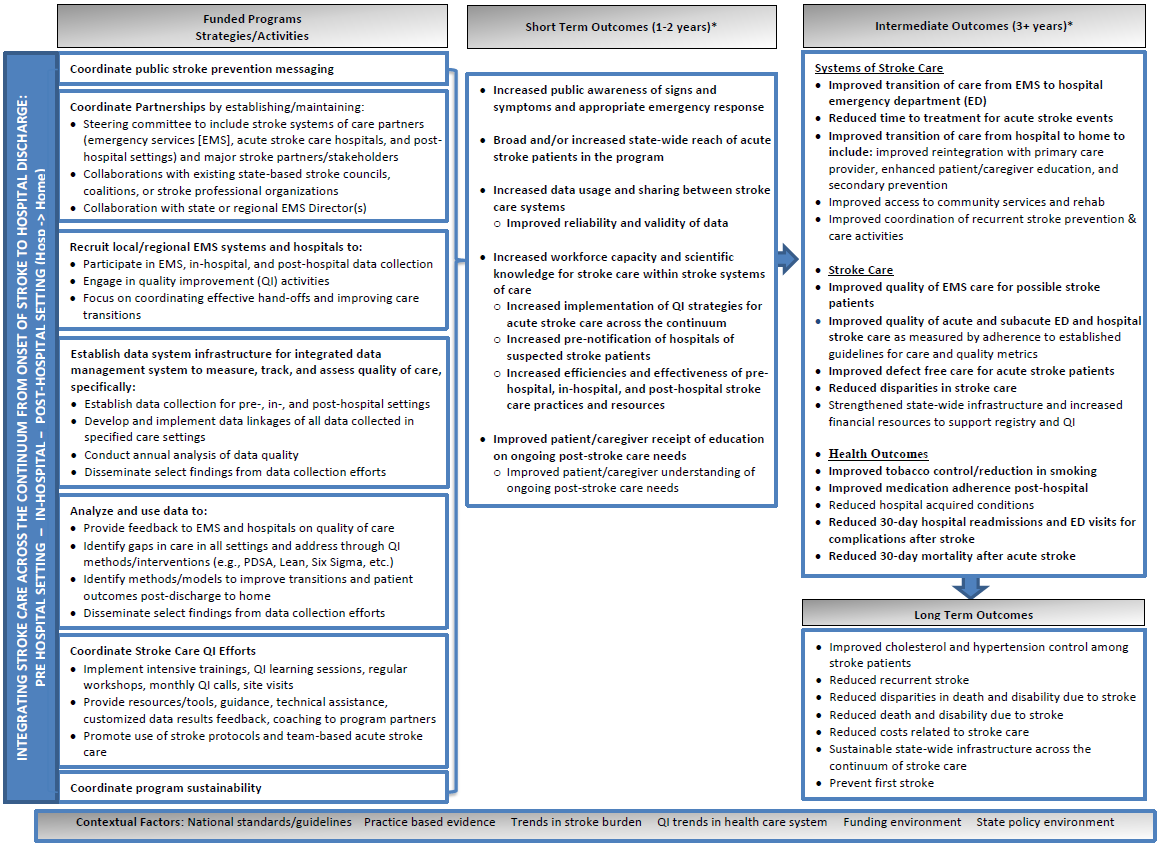
Logic Model
The Paul Coverdell National Acute Stroke Program Logic Model highlights key program activities and intended outcomes, and shows how they align with the CDC chronic disease prevention and health promotion domains. Download the Logic Model [PDF-247K].
- Page last reviewed: December 21, 2016
- Page last updated: December 21, 2016
- Content source:


 ShareCompartir
ShareCompartir