ABCs Report: Methicillin-Resistant Staphylococcus aureus, 2013
This website is archived for historical purposes and is no longer being maintained or updated.
May 18, 2015: Content on this page kept for historical reasons.
Active Bacterial Core Surveillance (ABCs): Emerging Infections Program Network
Print-friendly version of this surveillance report [3 pages]
ABCs Areas
California (3 county San Francisco Bay area); Colorado (5 county Denver area); Connecticut; Georgia (8 county Atlanta area); Maryland (Baltimore City and County); Minnesota (2 metro Twin City counties); New York (1 Rochester county); Oregon (3 county Portland area); Tennessee (1 Nashville county).
ABCs Population
The surveillance areas represent 19,842,441 persons
Source: National Center for Health Statistics bridged race vintage 2013 postcensal file.
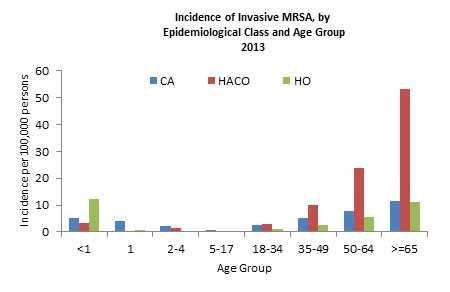
ABCs Case Definition
Invasive methicillin-resistant Staphylococcus aureus (MRSA) disease: isolation of MRSA from a normally sterile site in a resident of the surveillance area in 2013. Cases of disease are classified into one of three epidemiologic classifications. A case is classified as hospital-onset (HO) if the MRSA culture was obtained on or after the fourth calendar day of hospitalization, where admission is hospital day 1; as healthcare-associated community-onset (HACO) if the culture was obtained in an outpatient setting or before the fourth calendar day of hospitalization and had one or more of the following: 1) a history of hospitalization, surgery, dialysis, or residence in a long term care facility in the previous year, or 2) the presence of a central vascular catheter (CVC) within 2 days prior to MRSA culture; and as community-associated (CA) if none of the previously mentioned criteria are met.
ABCs Methodology
ABCs personnel routinely contacted all microbiology laboratories serving healthcare facilities in their area to identify cases. Standardized case report forms that include information on demographic characteristics, clinical syndrome, and outcome of illness were completed for each identified case. Convenience samples of isolates were collected and sent to CDC for routine testing, including antimicrobial susceptibility testing, toxin testing, SCCmec typing, and spa typing. Pulsed field gel electrophoresis (PFGE) of all isolates was discontinued in 2008; up until 2012, PFGE was inferred based on a validated algorithm. Starting in 2012, spa typing was added to the routine laboratory testing. Pulsed field type is currently inferred based on spa type, inferred MLST clonal complex and molecular characteristics of the isolates. In 2013, isolates were only collected in five sites (California, Georgia, Minnesota, New York, and Tennessee). Regular laboratory audits were performed to ensure completeness of case detection.
Rates of invasive MRSA disease among all patients were calculated using population estimates for 2013. Cases with unknown race were assigned race based on distribution of known age, race, and gender by EIP site. Confidence intervals for nationally estimated incidence rates of disease and mortality were calculated based on the gamma distribution (Stat Med, 1997 16:791-801).
Rates of invasive MRSA disease among patients who were undergoing chronic dialysis treatment were calculated using the December 31, 2012 point prevalent counts of patients on dialysis from the United States Renal Data System (USRDS).
ABCs Results
| Race | No. | (Ratea) |
|---|---|---|
| White | 2843 | (20.6) |
| Black | 1563 | (40.6) |
| Other | 170 | (7.9) |
Unknown race (n=390) distributed amongst known
aCases per 100,000 population for ABCs areas (crude rates)
| Dialysis and Access Type | No. (%) |
|---|---|
| Peritoneal | 29 (3.3) |
| Hemodialysis | 834 (95.6) |
| Hemodialysis - AV Fistula/Graft | 340 (39.0) |
| Hemodialysis - CVC | 462 (53.0) |
| Hemodialysis - Unkown | 32 (3.7) |
| Unkown | 9 (1.0) |
| MRSA Class | No. (Rate) Casesb |
No. (Rate) Deaths c |
Inferred PFGE Type (%) Tot N |
Inferred PFGE Type (%) USA100 |
Inferred PFGE Type (% USA300 |
Inferred PFGE Type (%) USA500/ Iberian |
|---|---|---|---|---|---|---|
| CA | 998 (5.0) | 102 (0.5) | 150 | 22 (14.7) | 103 (68.7) | 6 (4.0) |
| HCAa | 3529 (17.8) | 480 (2.4) | 554 | 243 (43.9) | 165 (29.8) | 75 (13.5) |
| HCA-HO | 704 (3.6) | 135 (0.7) | 111 | 48 (43.2) | 41 (36.9) | 9 (8.1) |
| HCA-HACO | 2825 (14.2) | 345 (1.7) | 443 | 195 (44.0) | 124 (28.0) | 66 (14.9) |
aHCA: Healthcare-associated invasive MRSA infection; sum of patients that are classified as either the HO or HACO classes
bn= 49 epidemiologic category unknown
cn=6; epidemiologic category unknown
| Syndromea | CA (n=998) No. (%) |
HACO (n=2825) No. (%) |
HO (n=704) No. (%) |
|---|---|---|---|
| Bloodstream Infection with other syndromeb | 521 (52.2) | 1363 (48.2) | 216 (30.7) |
| Bloodstream Infection with no other syndromeb | 210 (21.0) | 963 (34.1) | 247 (35.1) |
| Pneumonia | 141 (14.1) | 349 (12.4) | 95 (13.5) |
| Pneumonia - Lower Respiratory Infectionc | 44 (4.4) | 103 (3.6) | 28 (4.0) |
| Osteomyelitis | 154 (15.4) | 418 (14.8) | 142 (20.2) |
| Endocarditis | 75 (7.5) | 168 (5.9) | 29 (4.1) |
| Cellulitis | 180 (18.0) | 233 (8.2) | 56 (8.0) |
| Wounds - Surgicald | 8 (0.8) | 136 (4.8) | 28 (4.0) |
| Wounds - Decubitus/Pressure Ulcers | 10 (1.0) | 53 (1.9) | 11 (1.6) |
| Wounds - Skin Abscessese | 94 (9.4) | 87 (3.1) | 18 (2.6) |
| Wounds - Other woundsf | 32 (3.2) | 96 (3.4) | 32 (4.5) |
| Wounds - Traumatic | 11 (1.1) | 6 (0.2) | 3 (0.4) |
aSome case patients had more than one syndrome.
bCatheter site infection or AV fistula infection only are included in BSI with other syndrome.
cLower Respiratory Infection is defined as: a patient with pneumonia documented in their discharge summary who has a positive MRSA non-sterile respiratory specimen with accompanying chest radiology results documenting any of the following: bronchopneumonia/pneumonia, air space density/opacity, new or changed infiltrates.
dCombines deep tissue/organ infection and infection of a surgical wound, post operatively.
eCategory includes skin abscess, necrotizing fasciitis, gangrene.
fCategory includes non-traumatic and other chronic wound infections.
| Epidemiologic Category | Estimated Cases of Infection | |||||
|---|---|---|---|---|---|---|
| Non-Dialysis Patients | Dialysis Patients | Total | ||||
| Estimated No. | Incidence Rate (Confidence Interval)a | Estimated No. | Incidence Rate (Confidence Interval)b | Estimated No. | Incidence Rate (Confidence Interval)d | |
| CA | 16,117 | 5.10 (3.92-6.74) | NA | NA | 16,117 | 5.10 (3.92-6.74) |
| HCA | 43,864 | 13.90 (12.02-16.23) | 13,919 | 3079.89 (2331.21-4076.80) | 57,783 | 18.28 (15.34-22.04) |
| HCA-HO | 9,820 | 3.11 (2.24-4.39) | 1,584 | 350.44 (153.54-710.62) | 11,404 | 3.61 (2.46-5.40) |
| HCA-HACO | 34,044 | 10.78 (9.21-12.76) | 12,335 | 2729.00 (2026.78-3681.88) | 46,379 | 14.67 (12.10-18.00) |
| Overallc | 60,772 | 19.25 (16.94-22.05) | 13,921 | 3079.89 (2331.21-4076.80) | 74,693 | 23.63 (20.24-27.84) |
aNational Estimates and Incidence (no. per 100,000 population per year) are adjusted for age, race, gender and receipt of chronic dialysis using 2013 US Census Data.
bNational Estimates and Incidence (no. per 100,000 dialysis patients per year) for dialysis patients are adjusted for age, race and gender using 2012 USRDS point prevalence data.
c49 cases could not be classified into an epidemiological category or category is unknown and therefore are counted in the overall estimate only.
dStarting in 2011, confidence intervals on national estimates were determined for each of the 72 age/race/gender/dialysis specific strata and summarized for an overall national estimate, accounting for variance across all strata producing a more conservative estimate (with wider confidence intervals) compared to estimates prior to 2011.
| Epidemiologic Class | Estimated No. | Mortality Rate (Confidence Interval)a |
|---|---|---|
| CA | 1,710 | 0.54 (0.28-1.00) |
| HCA | 8,150 | 2.58 (1.68-4.01) |
| HCA-HO | 2,331 | 0.74 (0.33-1.59) |
| HCA-HACO | 5,819 | 1.84 (1.12-3.02) |
| Overallb | 9,937 | 3.14 (2.14-4.68) |
aNational Estimates and Mortality Rate (no. per 100,000 population per year) are adjusted for age, race, gender and receipt of chronic dialysis using 2013 US Census Data
b49 cases could not be classified into an epidemiological category or category is unknown and therefore are counted in the overall estimate only.
| Disease Rate | Estimate of Cases in United States.a | |||||
|---|---|---|---|---|---|---|
| Baseline (07-08) | 2013 | % Change | Baseline (07-08) | 2013 | Difference | |
| HCA | 27.08 | 18.28 | -32.50 | 82,000 | 58,000 | 24,000 |
aDisease Rate (no. per 100,000 population per year) and National Estimates are adjusted for age, race, gender and receipt of chronic dialysis using 2012 US Census Data
ABCs Discussion
Surveillance data from 2013 represent the ninth full year of performing population-based surveillance for invasive MRSA infections through the Emerging Infections Program/Active Bacterial Core Surveillance Activity.
Compared to 2012, incidence of healthcare-associated MRSA decreased by 1.01% while incidence of community-associated MRSA increased by 6.51%. Compared to the baseline incidence (2007-2008 calendar years) identified in the HHS Action Plan, there was a decrease of 32.50% for healthcare-associated MRSA.
Citation
- Centers for Disease Control and Prevention. 2013. Active Bacterial Core Surveillance Report, Emerging Infections Program Network, Methicillin-Resistant Staphylococcus aureus, 2013.
- Page last reviewed: May 18, 2015 (archived document)
- Content source:


 ShareCompartir
ShareCompartir