Levobupivacaine
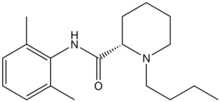
Levobupivacaine (rINN) /liːvoʊbjuːˈpɪvəkeɪn/ is a local anaesthetic drug belonging to the amino amide group. It is the S-enantiomer of bupivacaine.[1]
 | |
| Clinical data | |
|---|---|
| AHFS/Drugs.com | Micromedex Detailed Consumer Information |
| Pregnancy category |
|
| Routes of administration | Parenteral |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | n/a |
| Metabolism | Hepatic |
| Elimination half-life | 2–2.6 hours |
| Excretion | Renal 70%, faecal 24% |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| Chemical and physical data | |
| Formula | C18H28N2O |
| Molar mass | 288.43 g/mol g·mol−1 |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
| | |
Levobupivacaine hydrochloride is commonly marketed by AbbVie under the trade name Chirocaine.[2]
Clinical use
Compared to bupivacaine, levobupivacaine is associated with less vasodilation and has a longer duration of action. It is approximately 13 percent less potent (by molarity) than racemic bupivacaine and has a longer motor block onset time.[3]
Indications
Levobupivacaine is indicated for local anaesthesia including infiltration, nerve block, ophthalmic, epidural and intrathecal anaesthesia in adults; and infiltration analgesia in children.
Contraindications
Levobupivacaine is contraindicated for IV regional anaesthesia (IVRA).
Adverse effects
Adverse drug reactions (ADRs) are rare when it is administered correctly. Most ADRs relate to administration technique (resulting in systemic exposure) or pharmacological effects of anesthesia, however allergic reactions can rarely occur.
Systemic exposure to excessive quantities of bupivacaine mainly result in central nervous system (CNS) and cardiovascular effects – CVS effects usually occur at lower blood plasma concentrations and additional cardiovascular effects present at higher concentrations, though cardiovascular collapse may also occur with low concentrations. CNS effects may include CNS excitation (nervousness, tingling around the mouth, tinnitus, tremor, dizziness, blurred vision, seizures) followed by depression (drowsiness, loss of consciousness, respiratory depression and apnea). Cardiovascular effects include hypotension, bradycardia, arrhythmias, and/or cardiac arrest – some of which may be due to hypoxemia secondary to respiratory depression.[2]
Postarthroscopic glenohumeral chondrolysis
Levobupivacaine is toxic to cartilage and their intra-articular infusions can lead to postarthroscopic glenohumeral chondrolysis.[4]
References
- Burlacu CL, Buggy DJ (April 2008). "Update on local anesthetics: focus on levobupivacaine". Ther Clin Risk Manag. 4 (2): 381–92. PMC 2504073. PMID 18728849.
- Rossi S, editor. Australian Medicines Handbook 2006. Adelaide: Australian Medicines Handbook; 2006. ISBN 0-9757919-2-3
- Gulec D (Apr 2014). "Intrathecal bupivacaine or levobupivacaine: which should be used for elderly patients?". J Int Med Res. 42 (2): 376–385. doi:10.1177/0300060513496737. PMID 24595149.
- Gulihar, Abhinav; Robati, Shibby; Twaij, Haider; Salih, Alan; Taylor, Grahame J.S. (December 2015). "Articular cartilage and local anaesthetic: A systematic review of the current literature". Journal of Orthopaedics. 12: S200–S210. doi:10.1016/j.jor.2015.10.005. PMC 4796530. PMID 27047224.