Legius syndrome
Legius syndrome (LS) is an autosomal dominant condition characterized by cafe au lait spots.[2] It was first described in 2007 and is often mistaken for neurofibromatosis type I (NF-1). It is caused by mutations in the SPRED1 gene.[5][6] It is also known as neurofibromatosis type 1-like syndrome (NFLS).[1] The condition is a RASopathy, a group of developmental syndromes due to germline mutations in genes.[7][8]
| Legius syndrome | |
|---|---|
| Other names | Neurofibromatosis 1-like syndrome[1] |
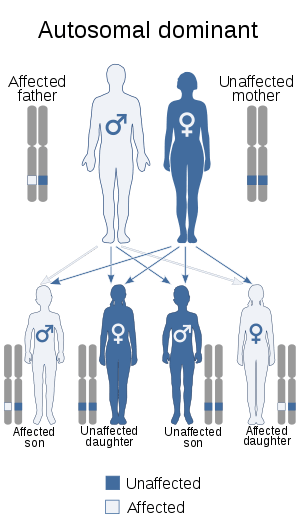 | |
| This condition is inherited in an autosomal dominant manner. | |
| Causes | Mutations in the SPRED1 gene[2] |
| Diagnostic method | Clinical findings, Genetic test[3] |
| Treatment | Physical therapy, Speech therapy[4][1] |
Symptoms and signs
Nearly all individuals show multiple café au lait spots.[7] Features common in neurofibromatosis – Lisch nodules, bone abnormalities, neurofibromas, optic pathway gliomas and malignant peripheral nerve sheath tumors – are absent in this condition.[1] Symptoms, however, may include:[4]
Cause
Legius syndrome is autosomal dominant in regards to inheritance and caused by mutations to the SPRED1 gene at chromosome 15, specifically 15q14 (or (GRCh38): 15:38,252,086-38,357,248).[9][10] The gene in question demonstrates almost 100 mutations.[1]
Mechanism
In terms of the mechanism of Legius syndrome, the Ras-MAPK signaling, which is a chain of proteins in a cell that sends signals to the nucleus of a cell from the surface receptors, can be regulated adversely by SPRED1 protein. When SPRED1 is dysfunctional then this in turn affects the aforementioned pathway, which in turn eventually leads to the physical symptoms created by this condition.[4][11]
Diagnosis
.jpg)
Genetic testing is necessary to identify the syndrome. The DNA test is necessary sometimes because symptoms may not be sufficient to definitely diagnose this condition.[3][1][12]
Differential diagnosis
Between this condition and NF-1 an important difference is the absence of tumor growths (Lisch nodules and neurofibromas which are common in NF-1) in LS.[4] The symptoms of Legius syndrome and NF-1 are very similar; this is the reason why the two are easily confused. A genetic test is often the only way to make sure a person has LS and not NF-1; the similarity of symptoms stem from the fact that the different genes affected in the two syndromes code for proteins that carry out a similar task in the same reaction pathway.
Treatment
The prognosis of this condition is generally considered good with the appropriate treatment. Management of Legius syndrome is done via the following:[4][1]
- Physical therapy
- Speech therapy
- Pharmacologic therapy (e.g. methylphenidate for ADHD)[13]
References
- RESERVED, INSERM US14 -- ALL RIGHTS. "Orphanet: Legius syndrome". www.orpha.net. Retrieved 2017-06-01.
- "Legius syndrome", Genetics Home Reference, National Institutes of Health
- "Legius syndrome | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program". rarediseases.info.nih.gov. Retrieved 2017-06-01.
- Stevenson, David; Viskochil, David; Mao, Rong (1993). "Legius Syndrome". GeneReviews. Retrieved 1 June 2017.update 2015
- "SPRED1", Genetics Home Reference, National Institutes of Health
- "Legius Syndrome Often Mistaken for Neurofibromatosis Type 1", by Allison Gandley, November 18, 2009, Medscape
- "OMIM Entry - # 611431 - LEGIUS SYNDROME". omim.org. Retrieved 2017-06-01.
- Tidyman, William (2009). "The RASopathies: Developmental syndromes of Ras/MAPK pathway dysregulation". Current Opinion in Genetics & Development. 19 (3): 230–236. doi:10.1016/j.gde.2009.04.001. PMC 2743116. PMID 19467855.
- "OMIM Entry - * 609291 - SPROUTY-RELATED EVH1 DOMAIN-CONTAINING PROTEIN 1; SPRED1". www.omim.org. Retrieved 2017-06-01.
- "Homo sapiens sprouty related EVH1 domain containing 1 (SPRED1), RefSeq - Nucleotide - NCBI". www.ncbi.nlm.nih.gov. Retrieved 2017-06-01.
- Molina, Julian R.; Adjei, Alex A. (2006-01-01). "The Ras/Raf/MAPK Pathway". Journal of Thoracic Oncology. 1 (1): 7–9. doi:10.1016/S1556-0864(15)31506-9.
- "SPRED1 sprouty related EVH1 domain containing 1 - Gene - GTR - NCBI". www.ncbi.nlm.nih.gov. Retrieved 2017-06-01.
- Jakob Storebø Ole (2015). "Benefits and harms of methylphenidate for children and adolescents with attention deficit hyperactivity disorder (ADHD) | Cochrane". Reviews (11): CD009885. doi:10.1002/14651858.CD009885.pub2. PMID 26599576.
Further reading
- MD, Robert P. Erickson; PhD, Anthony J. Wynshaw-Boris MD (2016). Epstein's Inborn Errors of Development: The Molecular Basis of Clinical Disorders of Morphogenesis. Oxford University Press. ISBN 9780190275426. Retrieved 1 June 2017.
- Zhang, Jia (2016). "Molecular screening strategies for NF1-like syndromes with café-au-lait macules (Review)". Molecular Medical Reports. 14 (5): 4023–4029. doi:10.3892/mmr.2016.5760. PMC 5112360. PMID 27666661. Review
External links
| Classification | |
|---|---|
| External resources |
|