Blue baby syndrome
Blue baby syndrome can refer to a number of conditions that affect oxygen transportation in the blood, resulting in blueness of the skin in babies. Historically, the term "blue baby syndrome" has referred to babies with one of two conditions:
- Cyanotic heart disease, which is a category of congenital heart defect that results in low levels of oxygen in the blood. This can be caused by either reduced blood flow to the lungs or mixing of oxygenated and deoxygenated blood.[1]
- Methemoglobinemia, which is a disease defined by high levels of methemoglobin in the blood. Increased levels of methemoglobin prevent oxygen from being released into the tissues and result in hypoxemia.[2]
| Blue baby syndrome | |
|---|---|
| Other names | Blue baby, cyanotic infant, cyanotic baby, cyanotic newborn |
 | |
| A cyanotic newborn, or "blue baby". Note the blue coloration of the fingertips. | |
| Specialty | Pediatrics, cardiac surgery |
Both of these conditions cause cyanosis, or a bluish discoloration of skin or mucous membranes.[3] Normally, oxygenated blood appears red and deoxygenated blood has more of a blue appearance. In babies with low levels of oxygen or mixing of oxygenated and deoxygenated blood, the blood can have a blue or purple color, causing cyanosis.[4]
Causes
Cyanotic heart disease
Specific types of congenital heart defects that cause blood to pass directly from the right side of the heart to the left side result in cyanosis.[5] In these defects, some of the blood that is pumped to the body has not been oxygenated by the lungs and therefore will appear more blue. Infants with these types of heart defects may have a constant bluish tint to their skin, or they may have temporary episodes of cyanosis. The degree of cyanosis is dependent on how much deoxygenated blood is mixed with oxygenated blood before being pumped to the body.
The five most common cyanotic heart defects that may result in Blue Baby Syndrome include the following:
| Pathology | Brief Description | Epidemiology | Diagram |
|---|---|---|---|
| 1. Persistent (or patent) truncus arteriosus | Instead of two separate major blood vessels leaving the heart, there is one common outgoing vessel.[6] | 3-5/100,000 births[7] | 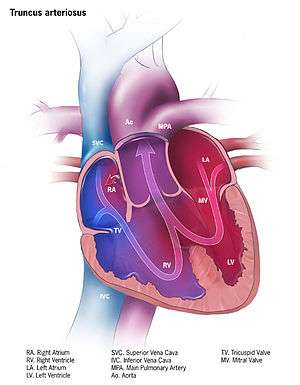 |
| 2. Transposition of the great vessels | The positions of the pulmonary artery and the aorta are switched, with the aorta connecting to the right ventricle and the pulmonary artery connecting to the left ventricle.[8] | 1-5/10,000 births[9] | 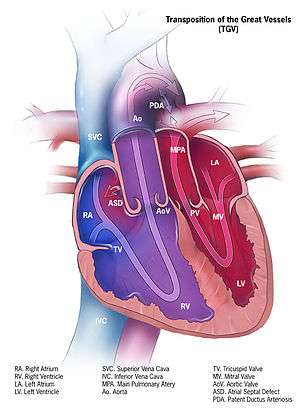 |
| 3. Tricuspid atresia | The heart valve connecting the right atrium to the right ventricle does not form properly, disrupting blood flow in the heart.[10] | 1-9/100,000 births[11] | 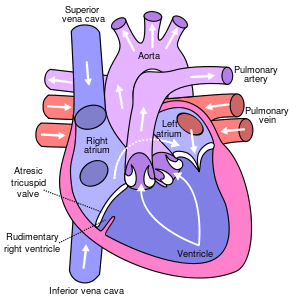 |
| 4. Tetralogy of Fallot | A heart defect with 4 features including a narrow pulmonary artery, a thick right ventricle, an aorta that connects to both the right and left ventricles, and a hole in the ventricular wall.[12] | 1-5/10,000 births[13] | 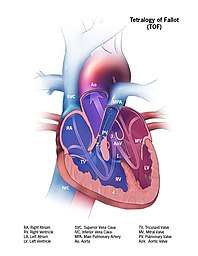 |
| 5. Anomalous pulmonary venous connection | The pulmonary veins returning oxygenated blood from the lungs do not connect properly to the heart.[14] | 6-12/100,000 births[15] | 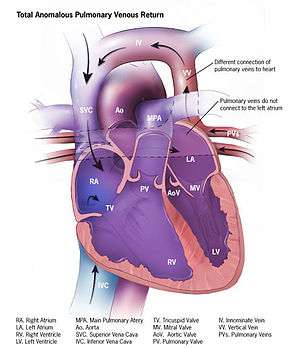 |
Methemoglobinemia
Blue baby syndrome can also be caused by methemoglobinemia, either due to a hereditary or acquired condition. Congenital methemoglobinemia is typically caused by an inherited deficiency in the enzyme NADH-cytochrome b5 reductase, which is responsible for reducing methemoglobin in the blood.[16] Methemoglobinemia can be acquired in infancy from a number of exposures, including certain drugs or nitrates in drinking water.[17] Nitrates from polluted drinking water form compounds in the body that change haemoglobin to methemoglobin, decreasing the ability of blood to carry oxygen. In infants, the condition can be fatal.[18] The sources of nitrate can include fertilizers used in agricultural lands, waste dumps or pit latrines.[19] For example, cases of blue baby syndrome have been reported in villages in Romania and Bulgaria, and were thought to be caused by groundwater polluted by nitrate leaching from pit latrines.[20] Nitrate levels are subject to monitoring to comply with drinking water quality standards in the United States and other countries.[21][22] The link between blue baby syndrome and nitrates in drinking water is widely accepted, but some studies indicate that other contaminants, or dietary nitrate sources, may also play a role in the syndrome.[20][23][24]
Other causes
Other problems in neonates, such as respiratory distress syndrome, can also produce temporary cyanosis. Like methemoglobinemia, these are not structural lesions and are not regarded by most doctors as true "cyanotic lesions."
Diagnosis
Symptoms of blue baby syndrome are often subtle. Cyanosis can be noted in babies around the lips, tongue, and sublingual area, where the skin is thinnest.[25] If cyanosis is suspected, pulse oximetry can used to measure oxygen saturation in the blood. While severe cyanosis can be easily noticed, an oxygen saturation as low as 80% causes only mild clinical cyanosis that is difficult to see.[26]
Babies with cyanosis due to congenital heart disease usually present with symptoms hours to days after birth. In addition to cyanosis, they often show signs of tachypnea (fast breathing), a heart murmur, and decreased peripheral pulses.[26][27] If congenital heart disease is suspected in a newborn, doctors will likely perform several tests to evaluate the heart, including a chest x-ray, echocardiogram, and electrocardiogram.[28]
Babies with cyanosis due to methemoglobinemia also usually present with cyanosis in the neonatal period, but pulse oximetry may be falsely elevated and does not always reveal low blood oxygen saturation. A co-oximeter can be used to detect levels of methemoglobin in the blood if methemoglobinemia is suspected.[29]
Management
Treatment for blue baby syndrome will depend on the underlying cause.
Cyanotic heart disease
Some babies born with cyanotic heart disease are treated with prostaglandin E1 after birth to keep the ductus arteriosus open and allow for more oxygenated blood to be pumped to the body. Many also receive oxygen therapy to increase the percentage of oxygen in the blood. Most of these babies will require surgery during infancy to correct their structural heart defect.[30]
Severe methemoglobinemia
The first-line treatment for severe methemoglobinemia is methylene blue, a medication that will reduce methemoglobin in the blood.[31]
History
The first successful operation to treat blue baby syndrome caused by Tetralogy of Fallot occurred at Johns Hopkins University in 1944. Through a collaboration between pediatric cardiologist Helen Taussig, surgeon Alfred Blalock, and surgical technician Vivien Thomas, the Blalock-Thomas-Taussig shunt was created. Dr. Taussig had recognized that children with Tetralogy of Fallot who also had a patent ductus arteriosus (PDA) typically lived longer, so the trio tried to create the same effect as a PDA by joining the subclavian artery to the pulmonary artery, relieving the child's cyanosis.[32] The operation was published in the Journal of the American Medical Association in 1945 and impacted management of blue babies around the world.[33]
References
- "Cyanotic heart disease: MedlinePlus Medical Encyclopedia". medlineplus.gov. Retrieved 1 November 2019.
- "Methemoglobinemia: MedlinePlus Medical Encyclopedia". medlineplus.gov. Retrieved 1 November 2019.
- Snider, H. L. (1990), Walker, H. Kenneth; Hall, W. Dallas; Hurst, J. Willis (eds.), "Cyanosis", Clinical Methods: The History, Physical, and Laboratory Examinations (3rd ed.), Butterworths, ISBN 9780409900774, PMID 21250208, retrieved 1 November 2019
- Silove, E. D. (1994). "Assessment and management of congenital heart disease in the newborn by the district paediatrician". Archives of Disease in Childhood: Fetal and Neonatal Edition. 70 (1): F71–74. doi:10.1136/fn.70.1.f71. ISSN 1359-2998. PMC 1060995. PMID 8117134.
- Lin, Pei-Yi; Hagan, Katherine; Fenoglio, Angela; Grant, P. Ellen; Franceschini, Maria Angela (16 May 2016). "Reduced cerebral blood flow and oxygen metabolism in extremely preterm neonates with low-grade germinal matrix- intraventricular hemorrhage". Scientific Reports. 6: 25903. Bibcode:2016NatSR...625903L. doi:10.1038/srep25903. ISSN 2045-2322. PMC 4867629. PMID 27181339.
- CDC (22 January 2019). "Congenital Heart Defects - Facts about Truncus Arteriosus | CDC". Centers for Disease Control and Prevention. Retrieved 20 November 2019.
- RESERVED, INSERM US14-- ALL RIGHTS. "Orphanet: Truncus arteriosus". www.orpha.net. Retrieved 20 November 2019.
- CDC (15 November 2019). "Congenital Heart Defects - dextro-Transposition of the Great Arteries". Centers for Disease Control and Prevention. Retrieved 20 November 2019.
- RESERVED, INSERM US14-- ALL RIGHTS. "Orphanet: Transposition of the great arteries". www.orpha.net. Retrieved 20 November 2019.
- CDC (19 November 2019). "Congenital Heart Defects - Facts about Tricuspid Atresia | CDC". Centers for Disease Control and Prevention. Retrieved 20 November 2019.
- RESERVED, INSERM US14-- ALL RIGHTS. "Orphanet: Tricuspid atresia". www.orpha.net. Retrieved 20 November 2019.
- CDC (19 November 2019). "Congenital Heart Defects - Facts about Tetralogy of Fallot | CDC". Centers for Disease Control and Prevention. Retrieved 20 November 2019.
- RESERVED, INSERM US14-- ALL RIGHTS. "Orphanet: Tetralogy of Fallot". www.orpha.net. Retrieved 20 November 2019.
- CDC (19 November 2019). "Congenital Heart Defects - Facts about TAVPR | CDC". Centers for Disease Control and Prevention. Retrieved 20 November 2019.
- "Total Anomalous Pulmonary Venous Return", The Pediatric Cardiac Anesthesia Handbook, John Wiley & Sons, Ltd, 2017, pp. 107–111, doi:10.1002/9781119095569.ch16, ISBN 978-1-119-09556-9
- Da-Silva, S. S.; Sajan, I. S.; Underwood, J. P. (1 August 2003). "Congenital Methemoglobinemia: A Rare Cause of Cyanosis in the Newborn--A Case Report". Pediatrics. 112 (2): e158–e161. doi:10.1542/peds.112.2.e158. ISSN 0031-4005. PMID 12897322.
- van de Vijver, M; Parish, E; Aladangady, N (2013). "Thinking outside of the blue box: a case presentation of neonatal methemoglobinemia". Journal of Perinatology. 33 (11): 903–904. doi:10.1038/jp.2013.74. ISSN 0743-8346. PMID 24169929.
- Manassaram, Deana M.; Backer, Lorraine C.; Moll, Deborah M. (2006). "A review of nitrates in drinking water: maternal exposure and adverse reproductive and developmental outcomes". Environmental Health Perspectives. 114 (3): 320–327. doi:10.1289/ehp.8407. ISSN 0091-6765. PMC 1392223. PMID 16507452.
- Majumdar Deepanjan (2003). "The Blue Baby Syndrome". Resonance. 8 (10): 20–30. doi:10.1007/BF02840703.
- Fewtrell, Lorna (22 July 2004). "Drinking-Water Nitrate, Methemoglobinemia, and Global Burden of Disease: A Discussion". Environmental Health Perspectives. 112 (14): 1371–1374. doi:10.1289/ehp.7216. PMC 1247562. PMID 15471727.
- "National Primary Drinking Water Regulations". EPA: United States Environmental Protection Agency. 30 November 2015. Retrieved 14 July 2018.
- "Water-related diseases". World Health Organization. Retrieved 14 July 2018.
- van Grinsven, Hans JM; Ward, Mary H = 2006 (2006). "Does the evidence about health risks associated with nitrate ingestion warrant an increase of the nitrate standard for drinking water?". Environ Health. 5 (1): 26. doi:10.1186/1476-069X-5-26. PMC 1586190. PMID 16989661.
- Ward, Mary H.; deKok, Theo M.; Levallois, Patrick; Brender, Jean; Gulis, Gabriel; Nolan, Bernard T.; VanDerslice, James (23 June 2005). "Workgroup Report: Drinking-Water Nitrate and Health—Recent Findings and Research Needs". Environmental Health Perspectives. 113 (11): 1607–1614. doi:10.1289/ehp.8043. PMC 1310926. PMID 16263519.
- McMullen, Sarah M.; Patrick, Ward (2013). "Cyanosis". The American Journal of Medicine. 126 (3): 210–212. doi:10.1016/j.amjmed.2012.11.004. ISSN 1555-7162. PMID 23410559.
- Silove, E D (1994). "Assessment and management of congenital heart disease in the newborn by the district paediatrician". Archives of Disease in Childhood: Fetal and Neonatal Edition. 70 (1): F71–F74. doi:10.1136/fn.70.1.f71. ISSN 1359-2998. PMC 1060995. PMID 8117134.
- Khalil, Markus; Jux, Christian; Rueblinger, Lucie; Behrje, Johanna; Esmaeili, Anoosh; Schranz, Dietmar (2019). "Acute therapy of newborns with critical congenital heart disease". Translational Pediatrics. 8 (2): 114–126. doi:10.21037/tp.2019.04.06. ISSN 2224-4344. PMC 6514285. PMID 31161078.
- "Symptoms and Diagnosis of Congenital Heart Defects". www.heart.org. Retrieved 13 November 2019.
- Da-Silva, Shonola S.; Sajan, Imran S.; Underwood, Joseph P. (1 August 2003). "Congenital Methemoglobinemia: A Rare Cause of Cyanosis in the Newborn—A Case Report". Pediatrics. 112 (2): e158–e161. doi:10.1542/peds.112.2.e158. ISSN 0031-4005. PMID 12897322.
- Khalil, Markus; Jux, Christian; Rueblinger, Lucie; Behrje, Johanna; Esmaeili, Anoosh; Schranz, Dietmar (2019). "Acute therapy of newborns with critical congenital heart disease". Translational Pediatrics. 8 (2): 114–126. doi:10.21037/tp.2019.04.06. ISSN 2224-4344. PMC 6514285. PMID 31161078.
- Da-Silva, Shonola S.; Sajan, Imran S.; Underwood, Joseph P. (1 August 2003). "Congenital Methemoglobinemia: A Rare Cause of Cyanosis in the Newborn—A Case Report". Pediatrics. 112 (2): e158–e161. doi:10.1542/peds.112.2.e158. ISSN 0031-4005. PMID 12897322.
- Thomas, Vivien, 1910-1985. (1985). Partners of the heart : Vivien Thomas and his work with Alfred Blalock : an autobiography. Thomas, Vivien, 1910-1985. Philadelphia: University of Pennsylvania Press. ISBN 0-8122-1634-2. OCLC 36761685.CS1 maint: multiple names: authors list (link)
- "That First Operation". Johns Hopkins Medical Institutions. Retrieved 13 November 2019.
External links
| Classification |
|---|