We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
Ventilator associated lung injury
From WikEM
Contents
Background
- Abbreviation: VALI
Terminology
- An acute lung injury that is suspected to have developed during mechanical ventilation is termed ventilator-associated lung injury (VALI)
- If it can be proven that the mechanical ventilation caused the acute lung injury it is termed ventilator-induced lung injury (VILI)
- VALI is the appropriate term in most clinical situations because it is virtually impossible to prove causation outside of the research laboratory
Epidemiology
- 1 in 4 mechanically ventilated patients will develop VALI for reasons other than acute lung injury (ALI) or Acute respiratory distress syndrome (ARDS)[1]
Pathogenesis
- VALI is alveolar injury caused by overexpansion of alveoli (volutrauma), repeated alveolar collapse and expansion (RACE), and cyclic atelectasis
- Eventually, in serve VALI/ARDS alveoli edema/bleeding and loss of surfactant can cause complete alveoli collapse[2]
Clinical Features
Indistinguishable from ARDS
Clinical signs
- Hypoxemic - or requiring a greater fraction of inspired oxygen (FiO2) to maintain the same arterial oxygen tension
- Tachypneic
- Tachycardic
- VALI may also be associated with multiple organ dysfunction syndrome (MODS)[3]
Imaging
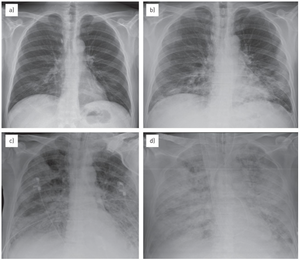
ARDS/VALI progression over the course of 1 week (a) Day 1 - No pathological findings. (b) Day 2 - some pulmonary consolidations in lower lobes. (c) Progressing to diffuse alveolar involvement, with “white lung” appearance (d). The normal-sized heart and vascular structures help in the differential diagnosis of pulmonary oedema due to heart failure.[4]
- CXR - increased bilateral interstitial or alveolar opacities of any severity.
- Computed tomography (CT) - heterogeneous consolidation and atelectasis, as well as focal hyperlucent areas that represent overdistended lung.[4]
Differential Diagnosis
- ARDS
- Cardiogenic Pulmonary Edema
- Acute exacerbation of idiopathic pulmonary fibrosis
- Pneumonia
- PE
- Diffuse alveolar hemorrhage
- DIC
- Pneumothorax
- Equipment failure
Evaluation
Overview
- VALI does NOT need to be distinguished from Acute respiratory distress syndrome because evaluation and management are the same[5]
- Both VALI and ARDS are a diagnosis of exclusion
- Check for Deterioration after intubation and exclude other etiologies
Imaging
- CXR
- Echocardiography
Labs
- BNP
- Below 100 pg/mL favors ARDS
- But higher levels neither confirm heart failure nor exclude ARDS[6]
- CBC
Other
- Noninvasive respiratory sampling
- Lower respiratory tract can be sampled via tracheobronchial aspiration or mini-bronchoalveolar lavage (mini-BAL)
- Tracheobronchial aspiration is performed by advancing a catheter through the endotracheal tube until resistance is met and then applying suction
Management
- Prevention is key with ventilator lung protective settings
- Management is the same as ARDS:
- Continue mechanical ventilation
- Apply lung protective settings (see Lung Injury Strategy section of Ventilation (Settings))
- Treat underlying causes
- Supportive care
Management by Injury Type[7]
| Injury | Mechanism | Management |
|---|---|---|
| Volutrauma & Barotrauma | Over-distension alveoli to pressures ≥ 30 cm H20 causing basement membrane stress | (a.) Maintain Plateau pressure ≤ 30 cm H20
(b.) Use tidal volume 6ml/kg of PBW (see EBQ:ARDSnet Trial) |
| Biotrauma | Release of chemokines and cytokines cause influx WBC resulting in pulmonary and systemic inflammation and multi-organ dysfunction | (a.) Protective lung ventilation
(b.) neuromuscular blockers may help. |
| Atelectotrauma | Repeated alveolar collapse and expansion (RACE) with tidal ventilation will contribute to lung injury. Alveoli especially easy to collapse if edematous | (a.) High PEEP of 5 cm H20
(b.) Consider prone positioning |
| Oxygen toxicity | Higher than needed O2 leads to free radicals with cause oxidative injury | (a.) Limit FiO2 and maintain higher PEEP.
(b.) Accept SaO2 at "shoulder" of oxyhaemoglobin dissociation curve (SaO2 88-94%). |
Ventilator Lung Protective Settings[5]
| Setting | Parameter |
|---|---|
| Mode | Assist Control (AC) - Fully supported mode (rather than partially supported) on either volume (better studied) or pressure control (both acceptable). |
| Tidal Volume | 6ml/kg of predicted body weight (PBW) |
| Respiratory Rate | 12-14bpm |
| PEEP | 5cm H20 |
| I:E | 1:2 |
| Plateau Pressure | ≤30 cm H2O |
Disposition
- Admit to ICU
External Links
See Also
References
- ↑ Gajic O, Dara SI, Mendez JL, et al. Ventilator-associated lung injury in patients without acute lung injury at the onset of mechanical ventilation. Crit Care Med 2004; 32:1817.
- ↑ Rouby JJ, Brochard L (2007). "Tidal recruitment and overinflation in acute respiratory distress syndrome: yin and yang.". Am J Respir Crit Care Med 175 (2): 104–6. doi:10.1164/rccm.200610-1564ED. PMID 17200505.
- ↑ Plötz FB, Slutsky AS, van Vught AJ, Heijnen CJ. Ventilator-induced lung injury and multiple system organ failure: a critical review of facts and hypotheses. Intensive Care Med 2004; 30:1865.
- ↑ 4.0 4.1 Zompatori M, Ciccarese F, Fasano L. Overview of current lung imaging in acute respiratory distress syndrome. Eur Respir Rev. 2014;23(134):519-30.
- ↑ 5.0 5.1 Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome Network. N Engl J Med 2000; 342:1301.
- ↑ Levitt JE, Vinayak AG, Gehlbach BK, et al. Diagnostic utility of B-type natriuretic peptide in critically ill patients with pulmonary edema: a prospective cohort study. Crit Care 2008; 12:R3.
- ↑ Nickson, Chris. "Ventilator Associated Lung Injury (VALI) | LITFL." LITFL Life in the Fast Lane Medical Blog. N.p., n.d. Web. 02 Aug. 2016.
