We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
Multiple myeloma
From WikEM
Contents
Background
- Malignant proliferation of plasma cells overproduction of abnormal antibodies (paraproteins or light-chain protein)
- Symptoms result from accumulation of plasma cells and paraproteins
Clinical Features
- Percentages below correspond to clinical presentations in newly diagnosed disease
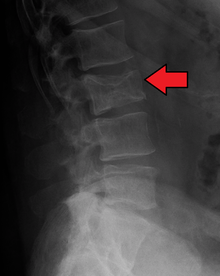
- Bone (plasma cell proliferation in marrow) lesions in ~80%
- Pathologic fractures
- Due to lytic lesions and osteopenia
- ”Punched-out” lytic lesion on x-ray
- Frequently involve spine, as well as ribs, skull, extremities
- Bone pain (even in absence of fracture) in ~60%[1]
- Commonly in back, ribs, extremities, often worse with movement
- Pathologic fractures
- Renal impairment in 20-40%[2]
- Ranges from mild creatinine elevation to ESRD
- Due to light-chain deposition, myeloma cast nephropathy and/or amyloidosis
- Hypercalcemia exacerbates
- Vulnerable to further damage from nephrotoxic mediations/contrast
- Hematologic
- Anemia in ~70%[3]
- Due to plasma cell infiltration in marrow +/- renal failure
- Hyperviscosity syndrome
- Increase serum viscosity due to paraproteins poor capillary flow and organ congestion
- Neuro
- Spinal cord compression due to vertebral fracture or collapse or plasmacytoma
- Intracranial plasmacytoma (rare)
- Peripheral neuropathy, radiculopathy
- Hypercalcemia
- Due to local osteolysis
- Though overall uncommon as first presentation finding
- Infection
- Impaired plasma cell function decreased effective antibody production
- Often on immunosuppressive chemotherapy or bone marrow transplant meds
- Splinting due to rib pain/fractures increased pneumonia risk
Differential Diagnosis
Anemia
RBC Loss
- Hemorrhage
RBC consumption (Destruction/hemolytic)
- Hereditary
- Acquired
- Microangiopathic Hemolytic Anemia (MAHA)
- Autoimmune hemolytic anemia
Impaired Production (Hypochromic/microcytic)
- Iron deficiency
- Anemia of chronic disease
- Thalassemia
- Sideroblastic anemia
Aplastic/myelodysplastic (normocytic)
Megaloblastic (macrocytic)
- Vitamin B12/folate deficiency
- Drugs (chemo)
- HIV
Evaluation
- Definitive diagnosis is by biopsy of marrow or plasmacytoma
- CBC
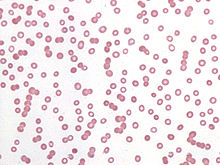
- Peripheral smear- may see Rouleaux formation of RBCs, atypical plasma cells
- BMP, ionized Ca, Mg, phos
- Paraproteins bind calcium, so non-ionized Ca levels could be falsely elevated
- Serum and urine testing for monoclonal protein (to aid in initial diagnosis if patient not already known to have MM)
- SPEP and UPEP electrophoresis, Bence Jones protein
- Other work up contingent on presentation:
- MRI spine: low threshold if any clinical evidence of cord compression
- Plain films of suspected pathologic fractures
- Infectious work up
Management
- Treat pain
- Consider referring to palliative care if feasible (or suggesting consult to patient/inpatient team)
- Manage other complications:
- If febrile, get cultures, start broad-spectrum antibiotics
- Splint fractures and/or consult ortho as appropriate
- See Hypercalcemia, Hypercalcemia of malignancy
- Prednisone 60mg PO daily can be helpful in addition to standard hypercalcemia treatments
- See Cord Compression, Malignant spinal cord compression, Epidural compression syndromes
- See Renal failure
- See Anemia
- If patient is eligible for transplant and indication equivocal, may want to avoid transfusion and/or consult oncology
Disposition
- Consideration for heme/onc consultation
See Also
External Links
References
- ↑ Kyle RA, Gertz MA, Witzig TE, et al. Review of 1027 patients with newly diagnosed multiple myeloma. Mayo Clin Proc 2003;78:21-33.
- ↑ Eleutherakis-Papaiakovou V, Bamias A, Gika D, et al. Renal failure in multiple myeloma: incidence, correlations, and prognostic significance. Leuk Lymphoma 2007;48:337-341.
- ↑ Birgegard G, Gascon P, Ludwig H. Evaluation of anaemia in patients with multiple myeloma and lymphoma: findings of the European Cancer Anaemia Survey. Eur J Haematol 2006;77:378-386.
- Multiple Myeloma. Antonio Palumbo, M.D., and Kenneth Anderson, M.D. N Engl J Med 2011; 364:1046-1060March 17, 2011. DOI: 10.1056/NEJMra1011442