We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
Mandibular dislocation
From WikEM
Contents
Background
- Anterior Dislocation
- Most common
- Mandibular condyle is forced in front of the articular eminence
- Risk factors: Prior dislocation, weak capsule, torn ligaments
- Often occurs spontaneously while patient is yawning, "popping" ears, or laughing
- Posterior Dislocation
- Follows a blow to the mandible that may or may not break the condylar neck
- Condylar head may prolapse into the external auditory canal
- Lateral Dislocation
- Often associated with mandibular fracture
- Superior Dislocation
- Occur from blow to the partially opened mouth
- Associated with cerebral contusions, facial nerve palsy, deafness
Clinical Features
- Anterior Dislocation
- Difficulty speaking or swallowing
- Malocclusion
- Pain localized anterior to the tragus
- Prominent-appearing lower jaw
- Preauricular depression
- Posterior Dislocation
- Must examine the external auditory canal
- Lateral Dislocation
- Condylar head is palpable in the temporal space
Differential Diagnosis
Jaw Spasms
- Dystonic reaction
- Acute tetanus
- Conversion disorder
- Mandibular dislocation
- Electrolyte abnormality
- Hypocalcemic tetany
- Magnesium
- Meningitis
- Seizure disorder
- Strychnine poisoning
- Akathisia
- Stroke
- Drug toxicity (anticholinergic, phenytoin, valproate, carbamazepine)
- Torticollis
- PTA
- Rabies
- TMJ
Evaluation
- Spontaneous, Atraumatic Anterior Dislocation: Clinical Diagnosis.
- Traumatic Dislocation: Obtain a CT scan.
- Always examine the cranial nerves to rule out concomitant injury.
Management
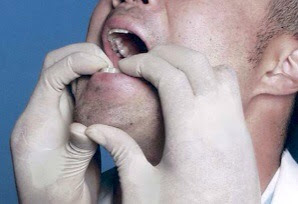
Standard Technique
- Place patient in seated position (anterior approach) or supine (posterior approach)
- Advisable to wrap thumbs in gauze to guard against accidental bite
- Placed gloved thumbs in patient's mouth over the occlusal surfaces of the molars, or lateral to patient's molars in buccal fold (to avoid being bitten)
- Apply pressure downward (toward the feet) and then backward (posteriorly)
Wrist Pivot Method[1]
- Place patient in seated position
- While facing the patient, grasp the mandible with your thumbs at the apex of the mentum and fingers on the occlusal surface of the inferior molars.
- Apply cephalad force with the thumbs and caudad pressure with the fingers
- Then pivot your wrists.
- Note: This is a more physiologic reduction technique for the provider, allowing greater and more sustained force to be exerted.
Tips
- Massage the TMJ externally prior to beginning the reduction attempt.
- Don't Forget the Analgesia!
- Consider IV benzodiazepines, opioids, or procedural sedation.
- Inject local anesthetic into the preauricular depression just anterior to the tragus.
- If dislocation is bilateral it may be easier to relocate one side at a time.
Disposition
Admit
- Open dislocation
- Superior dislocation
- Associated with fracture
- Nerve injury
- Inability to reduce
Discharge
Spontaneous, successfully reduced anterior dislocation with:
- Soft diet
- Tell patient not to open mouth wider than 2cm x 2wks
- Tell patient to support the mandible with a hand when they yawn
References
- ↑ Lowery LE, Beeson MS, Lum KK. The wrist pivot method, a novel technique for temporomandibular joint reduction. J Emerg Med. 2004 Aug;27(2):167-70. http://www.ncbi.nlm.nih.gov/pubmed/15261360