Transcript
Download Transcript as PDF
Jacqueline Moline, MD, MSc: Hello, I am Jacqueline Moline, chair of Occupational Medicine, Epidemiology and Prevention at Hofstra North Shore-LIJ School of Medicine at Hofstra University in Hempstead, New York. Welcome to this program titled "Advances in the Screening and Treatment of World Trade Center Responders and Survivors."
Hello, I am Jacqueline Moline, chair of Occupational Medicine, Epidemiology and Prevention at Hofstra North Shore-LIJ School of Medicine at Hofstra University in Hempstead, New York. Welcome to this program titled "Advances in the Screening and Treatment of World Trade Center Responders and Survivors."
Before we begin our discussion, please take a moment to test your knowledge on this topic by answering a few questions. You will have another chance to answer these questions at the end of the activity to see what you have learned.
There are several types of environmental exposures. They can occur from natural disasters or events precipitated by humans, such as terrorism or corporate or government negligence. Natural disasters include events such as earthquakes and hurricanes. Man-made disasters include the terrorist attacks that affected the World Trade Center on September 11 and other events such as the Indian Bhopal gas disaster.
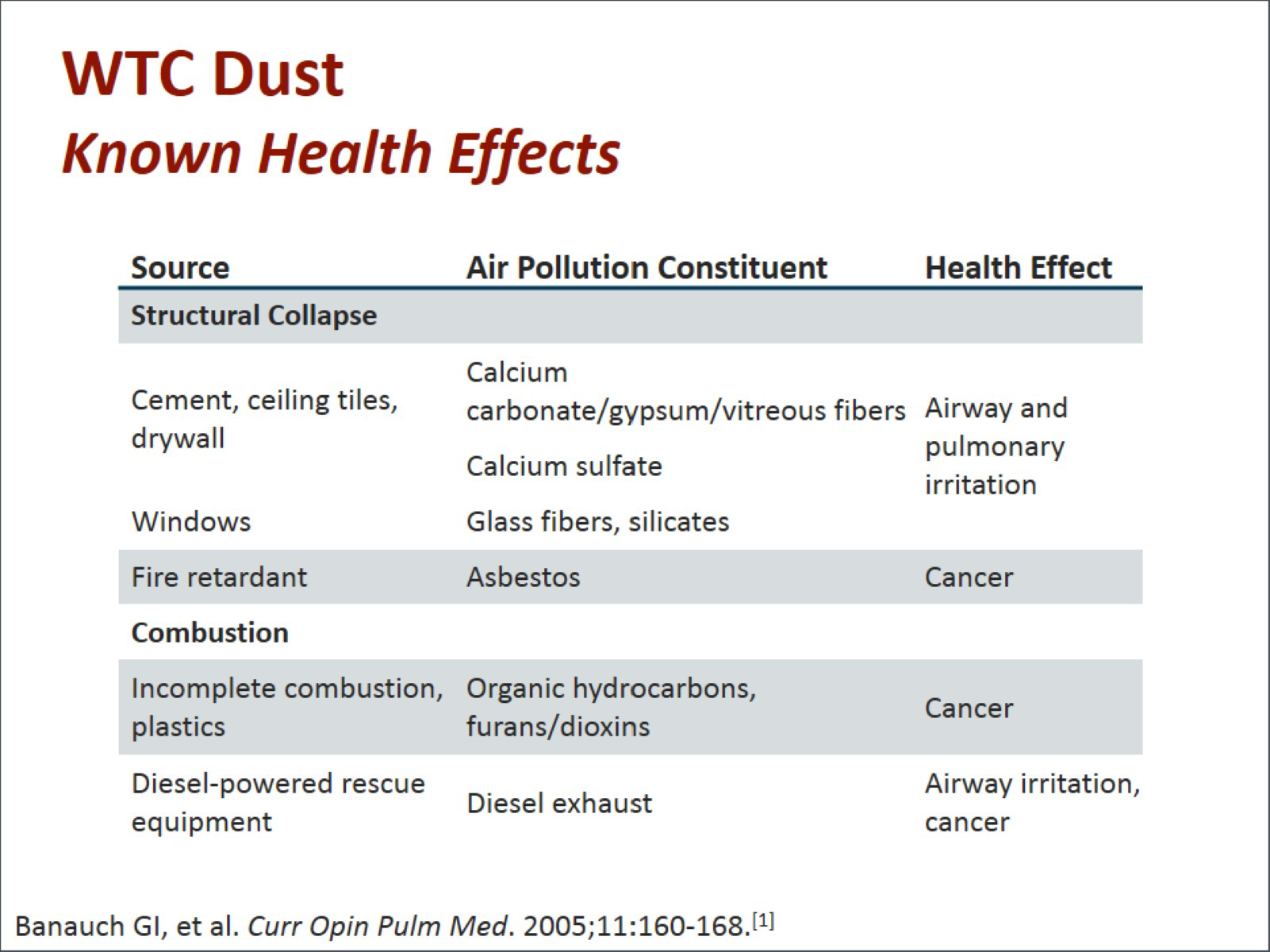
The World Trade Center dust had several constituents that have led to the many adverse health effects that we will be talking about in this program. There were a variety of compounds from the structural collapse, including the cement, ceiling tiles, drywall, windows, fire retardant; from the combustion, including the products of combustion; and from the diesel-powered rescue equipment. Many of these constituents led to different compounds such as calcium carbonate, gypsum, asbestos, glass fibers, silicates, hydrocarbons, dioxins, and diesel exhaust.
The health effects that we will be talking about in detail in this program include airway and pulmonary irritation, cancer, and other health concerns.
We are going to talk about the lessons we have learned from prior disasters and how we can use those experiences to inform us and move forward. We will talk about medical and psychological surveillance, exposure assessment, and the mental health consequences of disasters.
Let's discuss the World Trade Center surveillance programs. This includes our screening and monitoring program, which was initially designed to identify responders with possible World Trade Center health effects and provide appropriate referral for follow-up diagnostic testing and treatment. The treatment components of the World Trade Center Health Program developed and integrated both physical and mental health treatment. There were limits on coverage for care that presented challenges for both the provider and the patient.
To give you a timeline on the establishment of the programs, it is important to go back and see the initial setup. In April 2002, the World Trade Center Worker and Volunteer Medical Screening Program was started. Initially, it was a 1-year program. It was then extended to 2 years because of the demand for services. In March 2004, it became the World Trade Center Medical Monitoring Program with 5-year funding that was eventually extended for 2 additional years. In 2006, on the fifth anniversary of the attacks, federal funding for treatment of World Trade Center conditions began and the program was renamed the World Trade Center Medical Monitoring and Treatment Program.
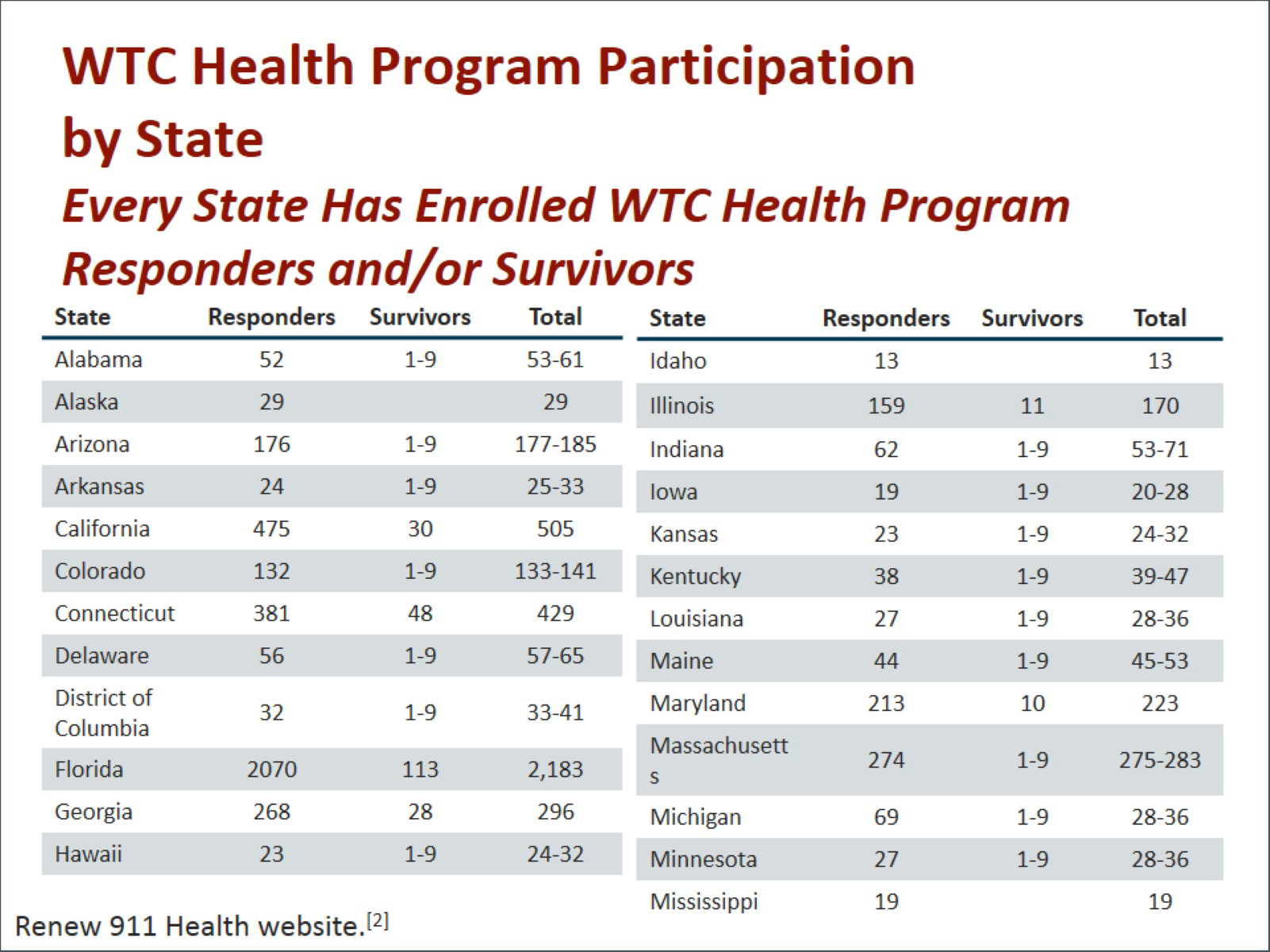
Every state has World Trade Center Health Program participants. If you look, you will see that there is representation from every state in both the responder and survivor programs, which we will discuss a little later. The majority of responders come from the New York Metropolitan area.
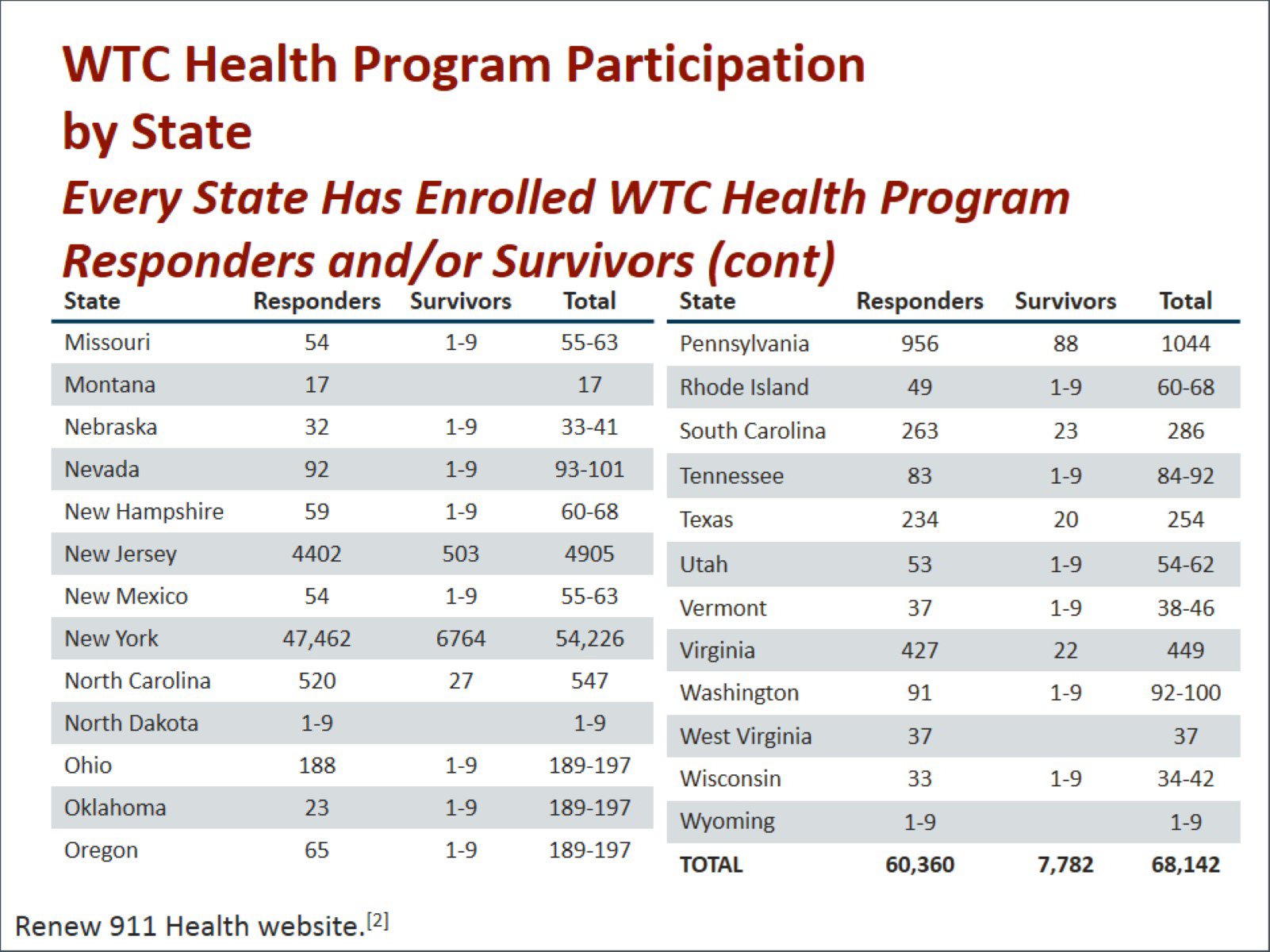
As you can see, there are about 54,000 participants in New York, but overall in the program there have been over 60,000 responders and almost 8000 survivors. To date, the total program participation is 68,142 individuals.
There were a number of components in the medical and psychological screening. These components of the program included self- and interviewer-administered medical questionnaires and a physician-administered examination, exposure assessment that was interviewer administered using a questionnaire, psychological screening and evaluation, spirometry done both pre- and post-bronchodilator, chest x-rays, and routine blood work.
When we think about assessment of exposure from the disaster, we have learned several lessons. There needed to be earlier testing of ambient exposures both at the site and nearby. There should have been more of a focus on toxicants other than asbestos. There should have been testing of indoor settings to establish a gradient of exposure with respect to distance from Ground Zero that would help guide recommendations. There needed to be consistent messaging on cleanup procedures.
There were other elements of exposure assessment that would have helped follow-up medical and mental health care. This became a problem because of issues related to Worker’s Compensation delays and a lack of occupational specialists who understood what to do in the wake of the disaster.
The population struggling with mental and behavioral health problems related to the World Trade Center attacks is heterogeneous. There were few psychiatrists or other mental health providers familiar with the nuances of the World Trade Center experience. There is still a need for mental health experts that speak a variety of languages, including Polish, Mandarin, Spanish, and others. These were the languages spoken by many of the responders at the World Trade Center site.
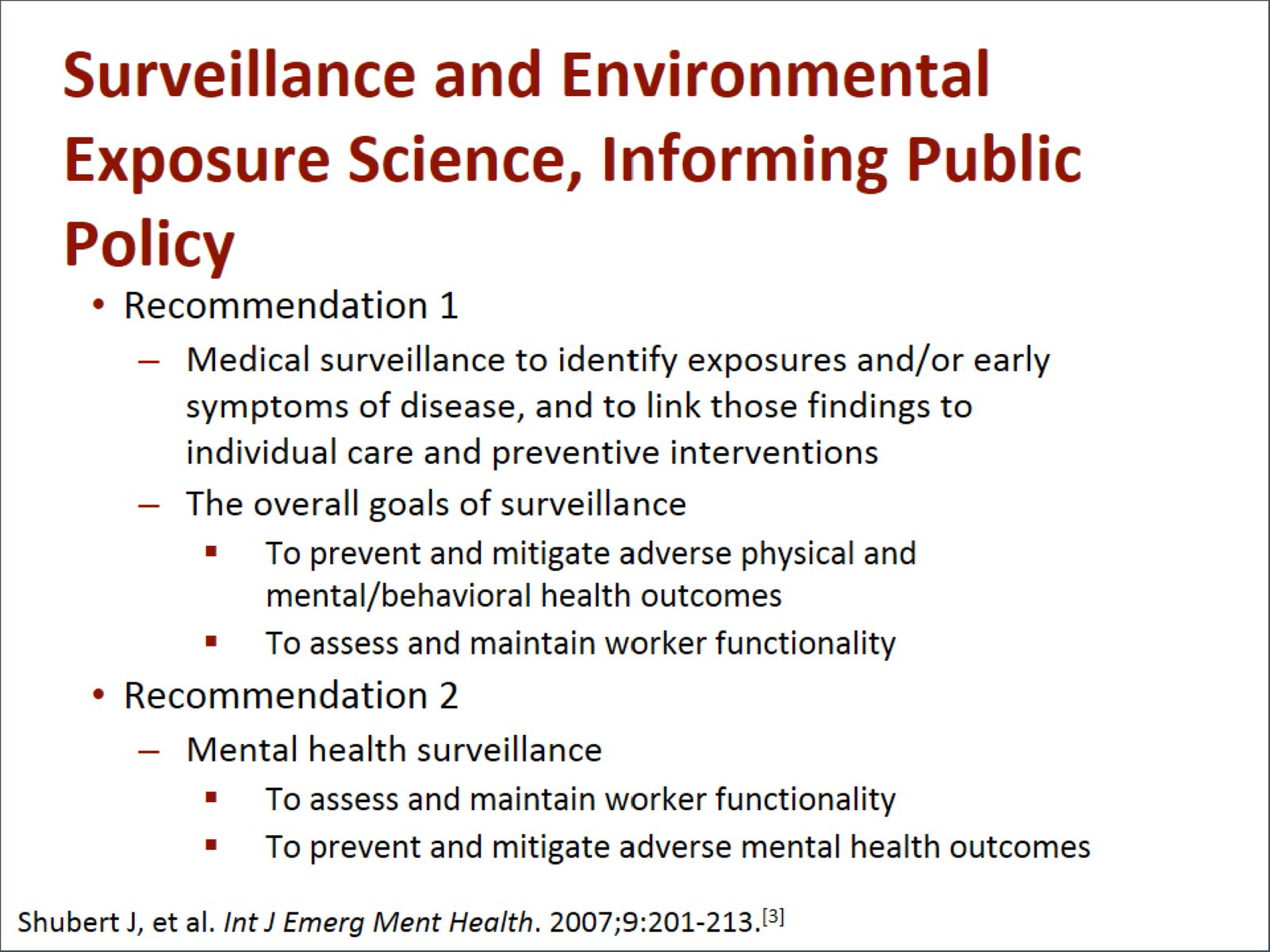
There are a number of recommendations that have come from surveillance and environmental exposure science that help us inform public policy. The first recommendation is to conduct medical surveillance to identify exposures and early symptoms of disease to link those findings to individual care and preventive interventions. The overall goals of surveillance are to prevent and mitigate adverse physical, mental, and behavioral health outcomes, and also to assess and maintain worker functionality.
A second recommendation is related to mental health surveillance. This is required to assess and maintain worker functionality and to prevent and mitigate adverse mental health outcomes.
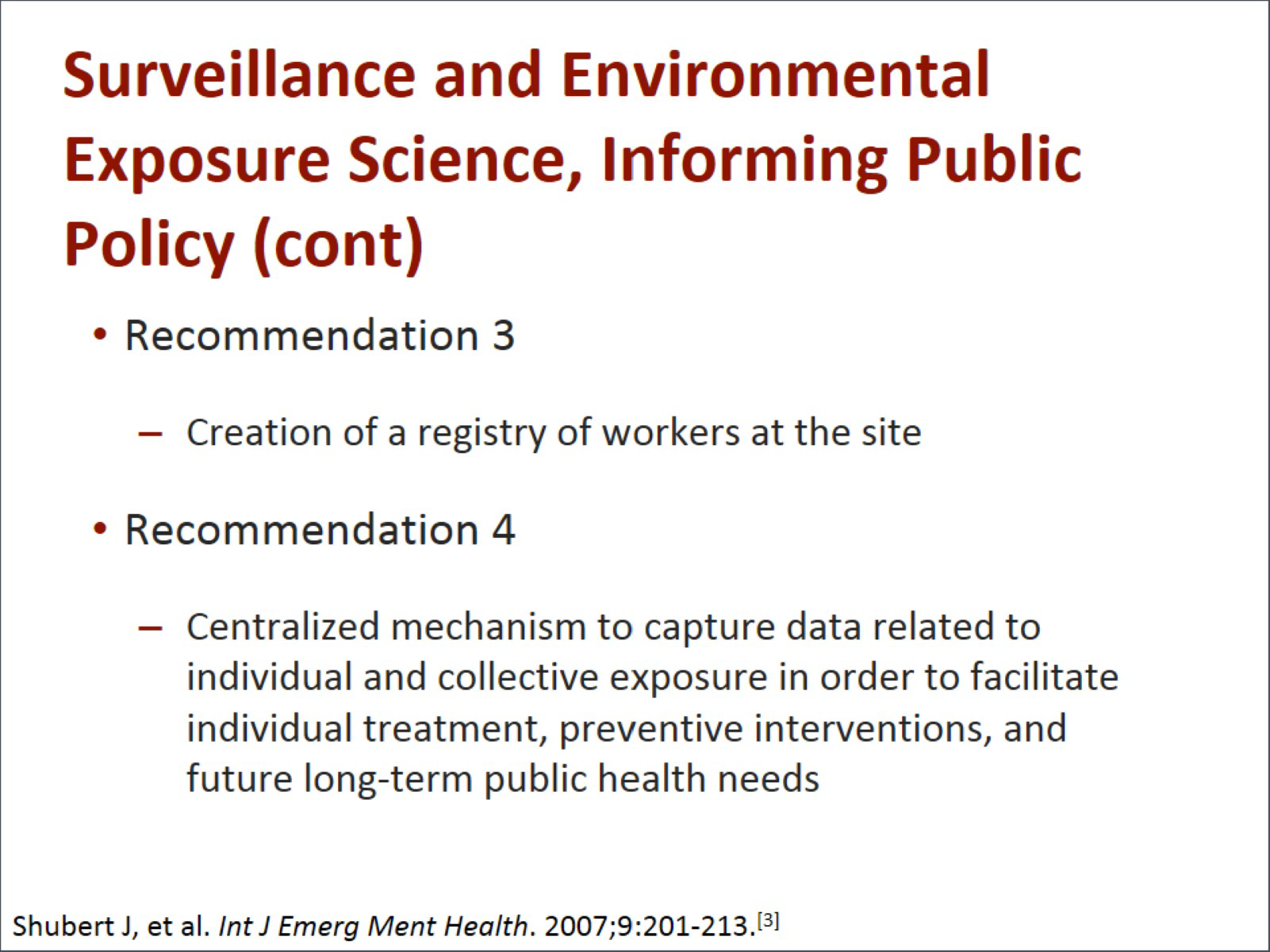
A third recommendation is the creation of a registry of all the workers at a disaster site. A fourth recommendation includes a centralized mechanism to capture the data related to the individual and collective exposures so we can facilitate individual treatment, preventive interventions, and future long-term public health needs.
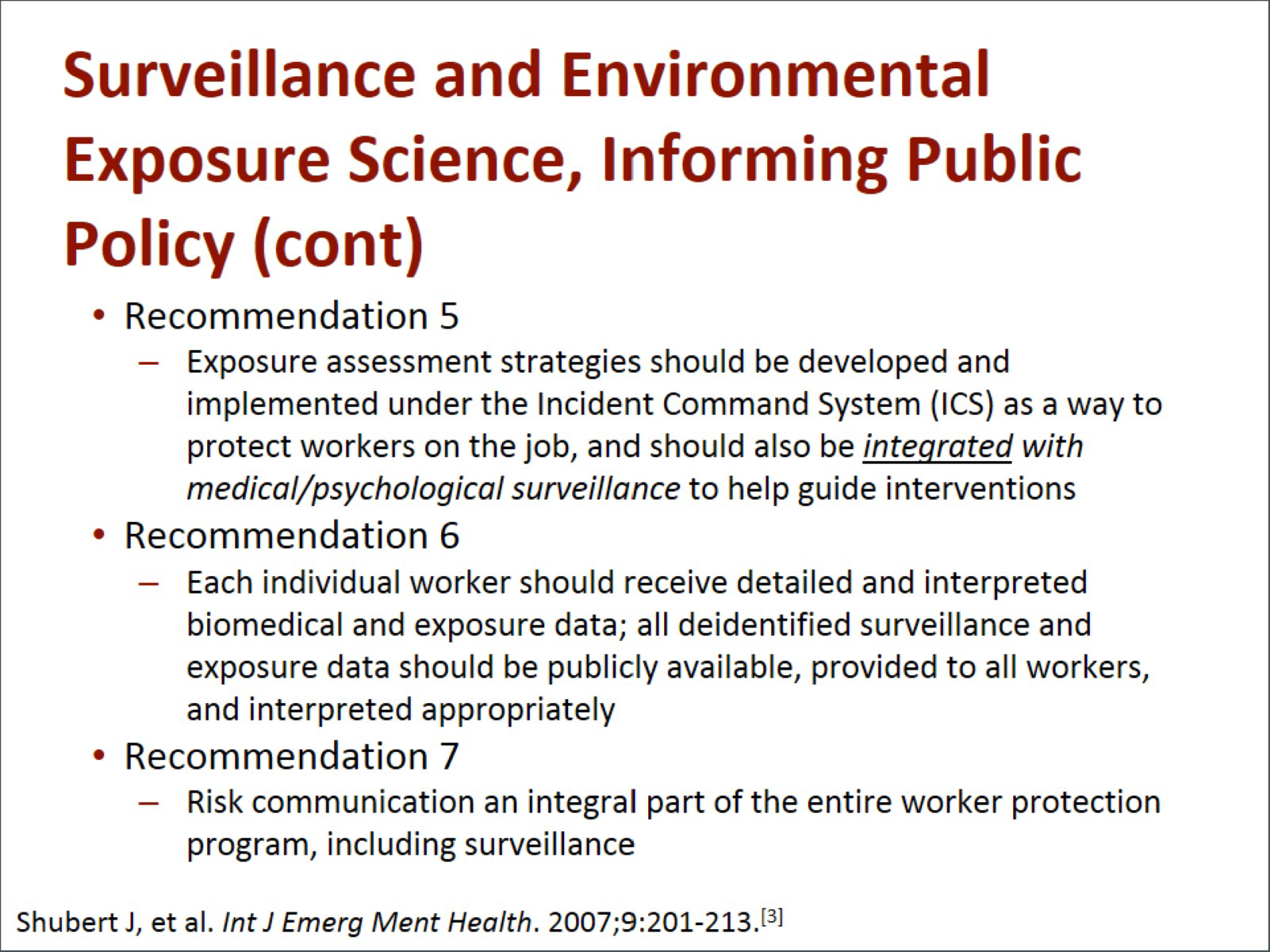
The fifth recommendation is for exposure assessment strategies that are developed under Incident Command Systems as a way to protect workers on the job. These should be integrated with medical and psychological surveillance programs to help guide interventions. Each individual worker should receive his or her own detailed and interpreted biomedical and exposure data. The sixth recommendations is that these results should also include deidentified surveillance and exposure data for all exposed individuals. The data should be available to the public, provided to the workers, and interpreted appropriately. A seventh recommendation is critical: Risk communication needs to be an integral part of an overall worker protection program, including surveillance.
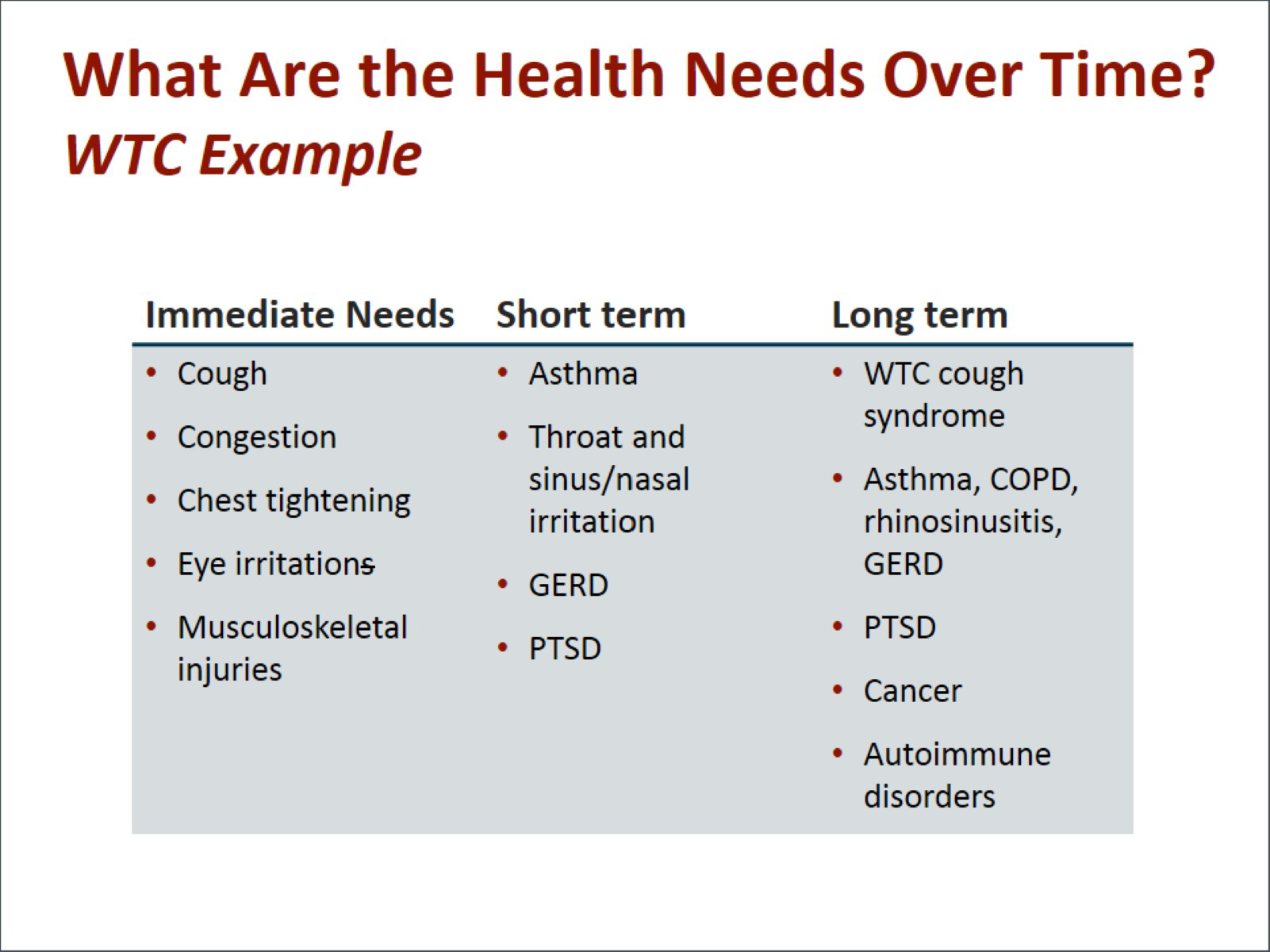
Let's look at the health needs that have developed over time. In the World Trade Center disaster, the immediate needs were related to cough, congestion, chest tightness, eye irritation, and musculoskeletal injuries. Short-term medical conditions included asthma, throat and sinus/nasal irritation, gastroesophageal reflux disease (GERD), and posttraumatic stress disorder (PTSD).
Long-term medical problems include the World Trade Center cough syndrome, asthma, chronic obstructive pulmonary disease (COPD), rhinosinusitis, GERD, autoimmune disorders, cancer, and PTSD. Many of the common disorders and complaints related to the World Trade Center disaster include respiratory problems such as asthma, shortness of breath, and chronic cough; GERD (which is a very common symptom, related to both acid and nonacid reflux); allergies; skin problems; and over 50 cancer types, with elevation seen particularly in rates of prostate cancer, thyroid cancer, multiple myeloma, and lymphoma.
Common mental health disorders seen among World Trade Center exposed individuals include PTSD, anxiety, depression, and substance abuse (especially tobacco, alcohol, cannabis, and opiates). Other symptoms include insomnia, headaches, memory and attention problems, interpersonal difficulties, and chronic pain syndromes.
The World Trade Center Health Registry was begun in approximately 2002. It was started using a questionnaire-based survey, with 71,437 people enrolled. The registry includes data on 17.4% of the estimated eligible-exposed population. This population of over 400,000 included building occupants, persons on the street or in transit in Lower Manhattan on September 11, local residents, rescue and recovery workers and volunteers, and school children and staff. Many of the folks participating in the World Trade Center Health Registry reported having been in the dust cloud emanating from the collapsing World Trade Center towers. In fact, over 51% of people responding in the World Trade Center Health Registry were in the dust cloud, 70% witnessed traumatic events, and 13% sustained an injury.
After September 11, 67% of the adult enrollees reported new or worsening respiratory symptoms, and 3% had newly diagnosed asthma. This was most frequently seen in the rescue and recovery workers who worked in the debris pile. When looking at mental health, we found that 16% of enrollees registered positive for probable PTSD and 8% for serious psychological distress. PTSD was higher among some groups, including those with low household income and those who were injured; many were of Hispanic ethnicity.
It was estimated that overall, between 3800 and 12,600 adults experienced newly diagnosed asthma and 34,000 to 70,000 adults experienced PTSD following the attacks, showing the sheer scope of folks affected after this man-made disaster.
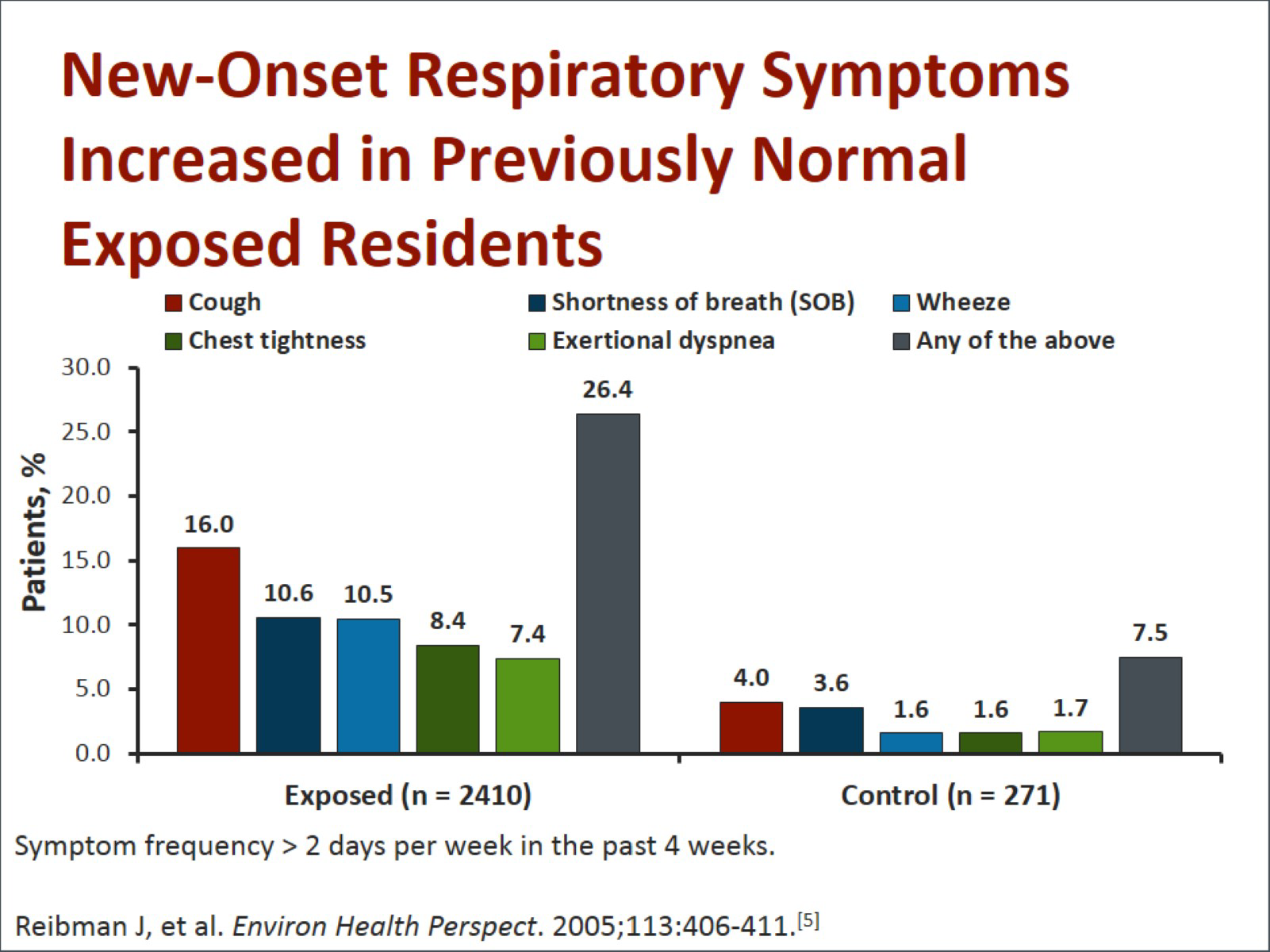
This graph shows new-onset respiratory symptoms in previously normal, exposed residents in Lower Manhattan. You can see that over 25% had symptoms compared to only 7% of controls who were not exposed. These symptoms included cough, chest tightness, shortness of breath, exertional dyspnea, or wheeze.
This survivor population, which included building reoccupants, local residents, school children, and those who lived in Lower Manhattan, exhibited symptoms related to cough, wheezing, dyspnea on exertion, chest tightness, and sinus and nasal problems.
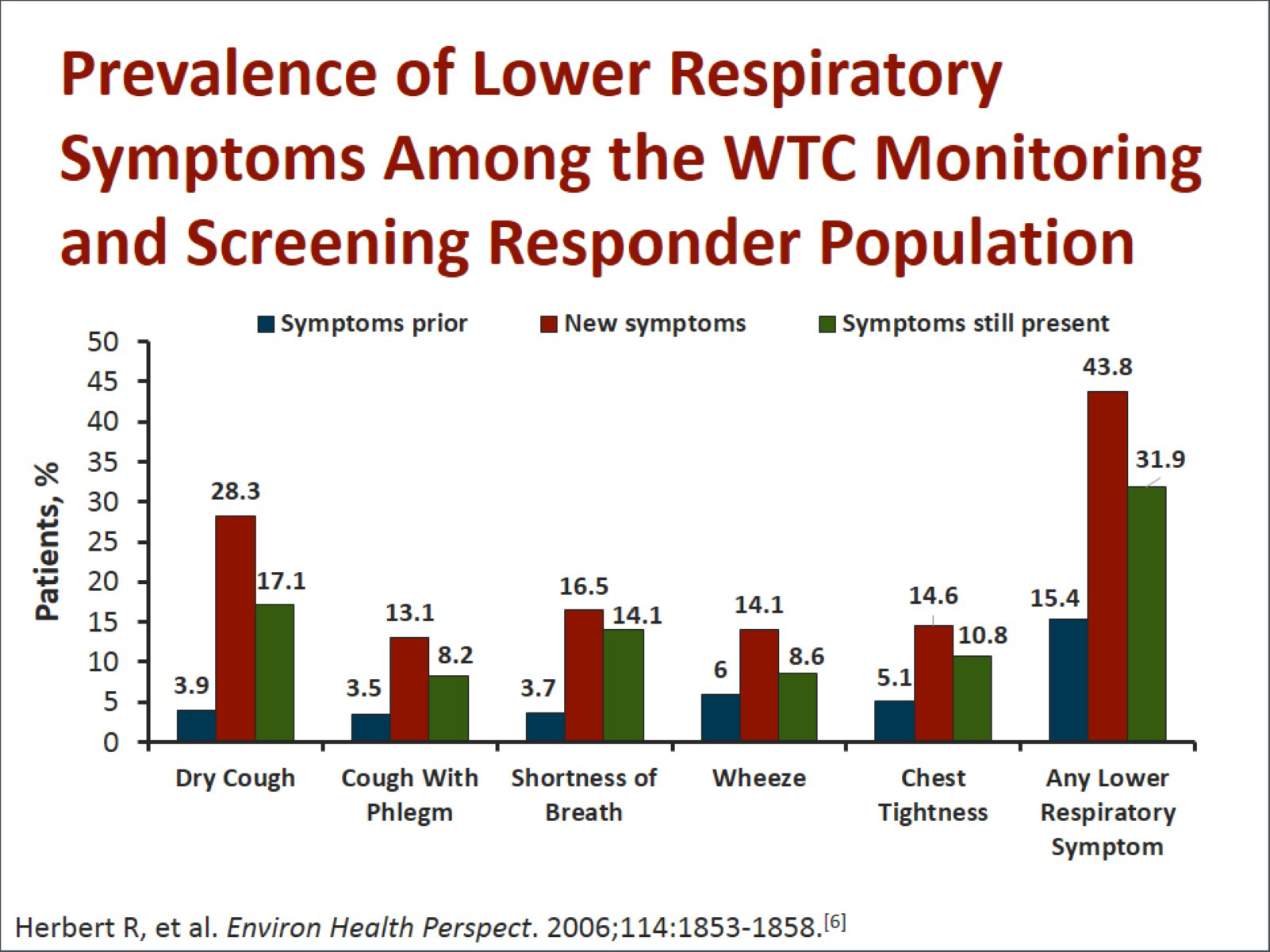
The prevalence of lower respiratory symptoms among responders included many of the same findings as those who were survivors. This included cough, shortness of breath, wheeze, and chest tightness. If we look at the combination of any lower respiratory symptoms, we see that the symptom rate was nearly 44%.
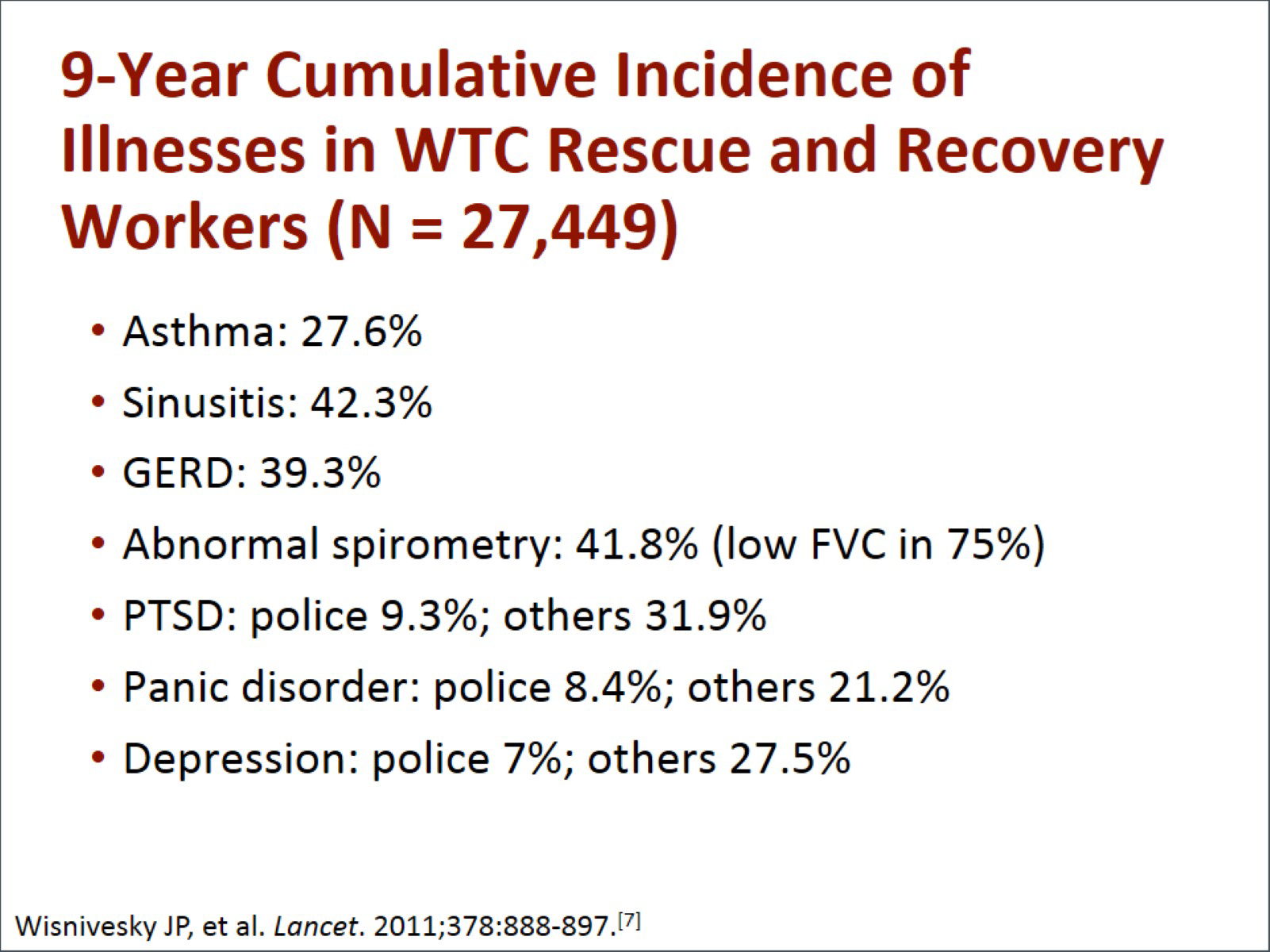
In a look back after 9 years, the cumulative incidence of illnesses in the World Trade Center rescue and recovery workers, nearly 27,500 individuals, included asthma in 27.6% of responders, sinusitis in over 42%, GERD in almost 40%, and abnormal spirometry in 42%. The predominant finding was low forced vital capacity, which was seen in 75% of individuals with abnormal spirometry.
With respect to mental health conditions, PTSD was seen in the police and other responders at different rates. For the police, it was about 9.3%; for all other responders, it was nearly 32%. Panic disorder was seen in 21% of the general responders and in 8.4% of the police. Depression rates were seen in 27.5% of the responders in general and in 7% of the police.
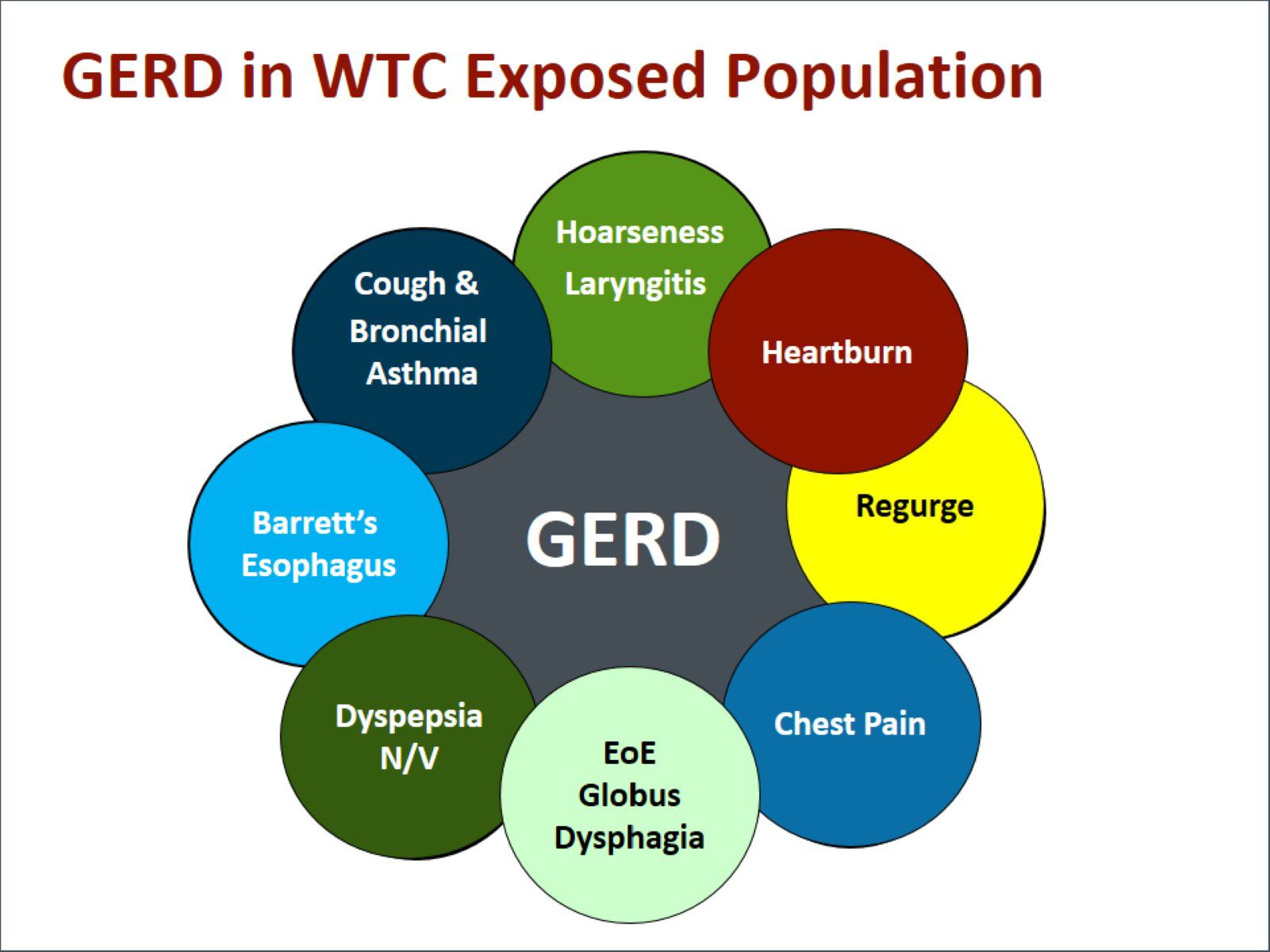
In the World Trade Center population, GERD has been a persistent and common problem related to a variety of other symptoms. This graphic shows the interrelationship between many of the symptoms and problems that we have seen in this population, whether it be chest pain, cough, bronchial asthma, hoarseness, laryngitis, dyspepsia, nausea and vomiting, or Barrett's esophagus, which has the potential to lead to esophageal cancer.
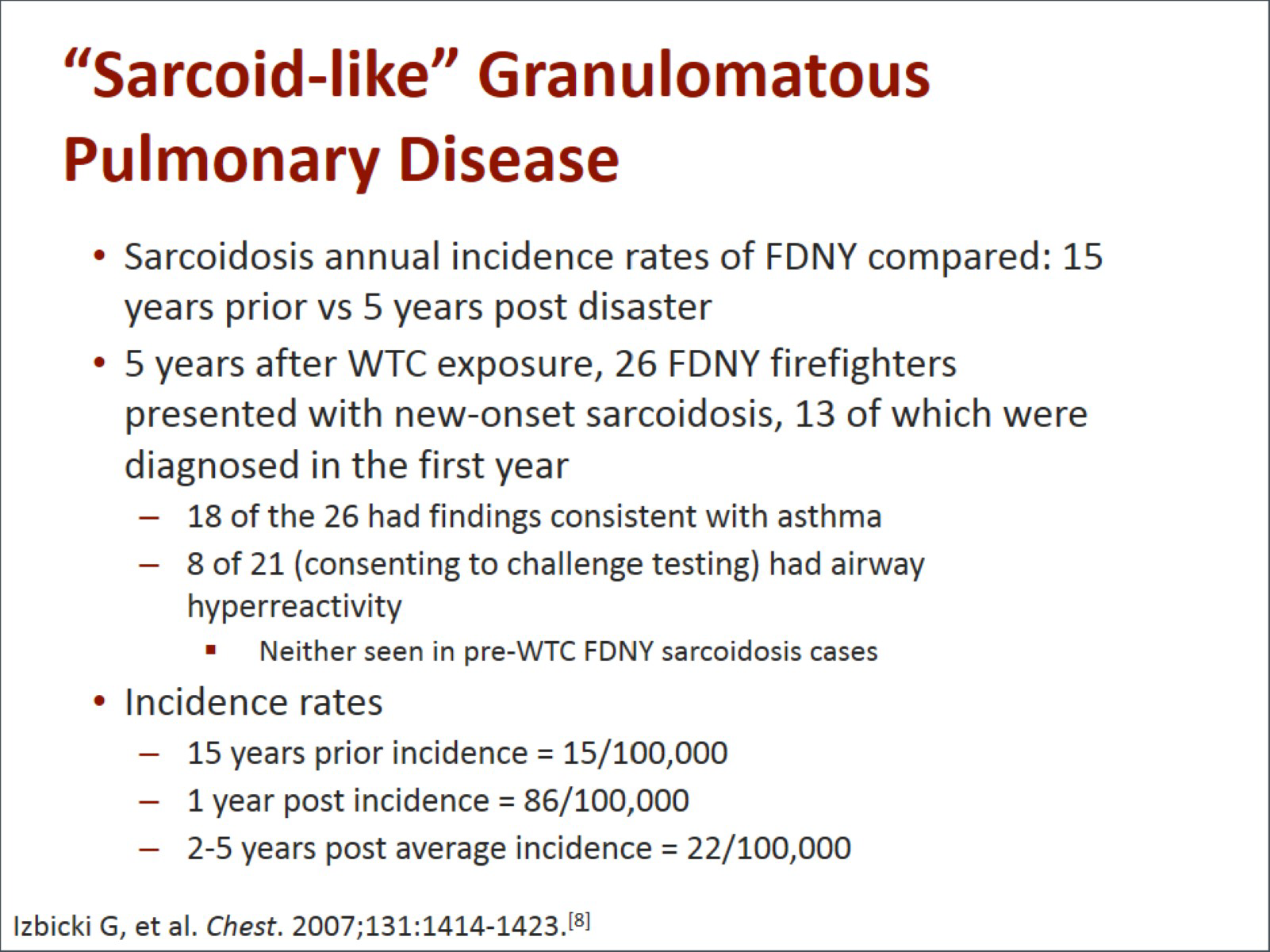
Other diseases have shown up at increased rates. This includes sarcoid-like granulomatous pulmonary disease, which was described in both the New York City Fire Department (FDNY) and in the responder population. Annual incidence rates of sarcoidosis among members of the FDNY were elevated after September 11. The FDNY compared rates 15 years prior to 9/11 and 5 years after the disaster.
In the 5 years after 9/11, 26 firefighters presented with new-onset sarcoidosis, 13 of whom were diagnosed in the first year. Their findings were consistent with asthma, and many of them had airway hyperreactivity. This had not been seen in sarcoidosis cases pre-9/11 in the fire department. Incidence in the 15 years prior was 15/100,000, but within 1 year after 9/11, it had jumped to 86/100,000. The rate declined in the 2 to 5 years after 9/11, but it still remained elevated at 22/100,000.
One of the important elements of the World Trade Center Medical Programs has been an assessment of ongoing mental health. In looking at over 10,000 World Trade Center workers who completed self-administered mental health questionnaires in the 10 to 61 months after the 9/11 attack, 11% had criteria for probable PTSD, 8.8% for probable depression, 5% for probable panic disorder, and 62% met criteria for substantial stress reaction. Extensive comorbidity was observed and included high rates of impairment of social function. Chronic impairment of mental health and social functioning is associated with participation in 9/11 recovery operations.
When we looked at mental health effects among the different responders and the difference between members of the New York City Police Department (NYPD) and nontraditional responders, we saw a stark contrast. Fewer NYPD members than nontraditional responders had probable PTSD. The numbers were quite stark, with 5.9% of the police having probable PTSD vs 23% of the nontraditional responders. This includes construction workers and other folks who were responding to the disaster and were involved in cleanup. Respiratory symptoms were somewhat similar, with 22.5% in the NYPD and 28% in the nontraditional responders.
Exposure among NYPD members was more associated with respiratory symptoms than PTSD or lung function. Some of the hypotheses explaining these differences are that (1) perhaps it has to do with the screening and selection process in becoming a member of the NYPD, or (2) it might be a result of their training and drills, which might mitigate some of these longer-term effects.
There are 2 different parts to the World Trade Center Health Program, as it is now called. The program for responders is called the WTC Workers Monitoring and Treatment Program. This would include those involved in rescue, recovery, and debris removal as well as volunteers at the site. They undergo medical and mental health screening, monitoring, and treatment; the presence of symptoms is not necessary to be eligible for the program. The program for survivors is known as the World Trade Center Environmental Health Center. Survivors include community members, local workers, building reoccupants, residents, students, and cleanup workers. Medical and mental health treatment is included for WTC-related medical and mental health symptoms and cancers. Medical and mental health monitoring is available once people are enrolled in the program. However, it differs from the Responders program in that the presence of symptoms or cancers is necessary to be program eligible.
There are a number of other registries for tracking exposure to disasters or having particular diseases. We talked about the World Trade Center Health Registry, which was the health survey that was sent to those directly exposed to the events of 9/11. Other registries include the Katrina and Rita Exposures (KARE) Registry. There is a National Amyotrophic Lateral Sclerosis (ALS) Registry and a Rapid Response Registry, which is designed to help local, state, and federal public health and disaster response agencies, rapidly established registries for people who are exposed, or potentially exposed to chemicals and other agents during catastrophic events.
What lessons have we learned? Environmental disasters may be natural or man-made; there are high rates of comorbid medical and mental health conditions in rescue workers and survivors of environmental health disasters. There is a need for integrated mental and medical health care, and we must account for the psychological burden of chronic medical illness in those impacted by disasters. The importance of ongoing surveillance even decades after a disaster is critical. Once a disaster has occurred, there should be a comprehensive safety and health risk assessment at the onset of an incident.
Sampling results should be reported in a methodical and diligent manner. There should be a variety of methods used to protect workers and those exposed. Safety and health training should be provided to affected workers, employers, and other agencies. A multidisciplinary approach is needed for disaster programs. Most importantly, referrals to the World Trade Center Health Program can and should still be made for those affected by the 9/11 disaster.


 File Formats Help:
File Formats Help: